Translate this page into:
Retiform hemangioendothelioma: A rare entity at atypical site
2 Department of Pathology, PGIMER and Dr. RMLH, New Delhi, India
Correspondence Address:
Seema Rani
Department of Dermatology, PGIMER and Dr. RMLH, New Delhi - 110 001
India
| How to cite this article: Rani S, Singh J, Ahuja AK, Bhardwaj M. Retiform hemangioendothelioma: A rare entity at atypical site. Indian J Dermatol Venereol Leprol 2016;82:550-552 |
Sir,
Hemangioendothelioma is the term used for vascular neoplasms that show a borderline biological behavior, intermediate between the entirely benign hemangiomas and the highly malignant angiosarcomas. Retiform haemangioendothelioma is a rare variant of low-grade angiosarcoma with a tendency for local aggressive behavior.
A 23-year-old woman presented with a painless, reddish swelling on her scalp for the last 2 years. Her previous medical history was unremarkable except for a single episode of seizures during childhood following trauma to the head. Clinical examination revealed a well-defined, erythematous, soft, compressible, non-tender, 1–2 cm nodule situated on the left temporal side of the scalp [Figure - 1]. A clinical diagnosis of pilar cyst was made and the lesion was biopsied. Histopathological examination revealed orthokeratotic stratified squamous epithelium showing mild spongiosis, follicular plugging and irregular rete pegs. The superficial dermis showed edema and a mild perivascular infiltrate [Figure - 2]. A small focus in the superficial dermis and a larger focus in the deeper dermis, extending upto the subcutaneous tissue, showed long, arborizing, branching blood vessels which were lined by monomorphic endothelial cells with prominent, protuberant hobnail nuclei and scanty cytoplasm. Some interspersed lymphocytes were also seen [Figure - 3]. In addition, immunohistochemistry showed CD34 positivity [Figure - 4]. The immunostain Ki-67 indicated occasional positivity suggestive of cell proliferation. The labeling index was low (approximately 3–4%) [Figure - 5]. Based on these histopathological findings, a diagnosis of retiform hemangioendothelioma was made and the tumor was subsequently excised.
 |
| Figure 1: Single, well-defined erythematous, soft, compressible nodule on the left temporal scalp |
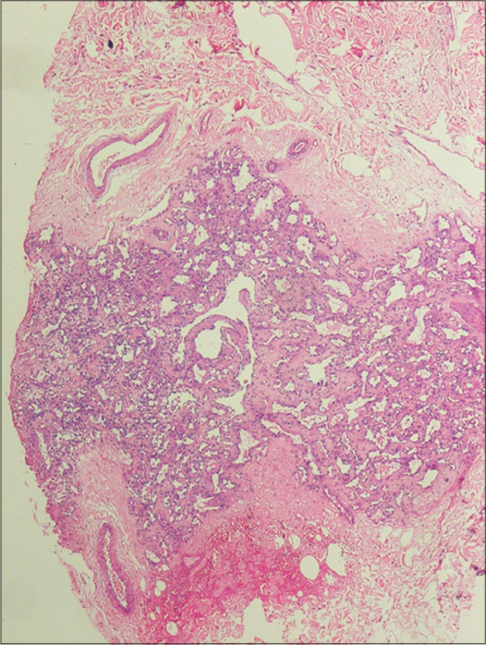 |
| Figure 2: Branching slit-like blood vessels in the reticular dermis (H and E, ×100) |
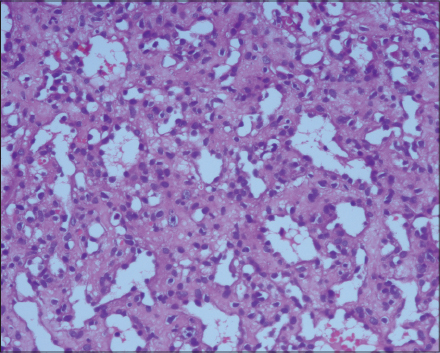 |
| Figure 3: Blood vessels lined by bland monomorphic hobnail endothelial cells with lymphocytic infiltrates (H and E, ×400) |
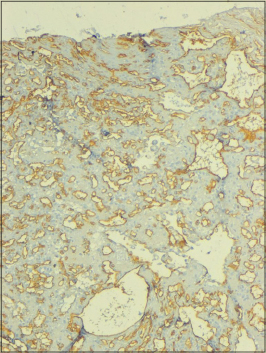 |
| Figure 4: CD34 positive tumor cells (IHC, ×200) |
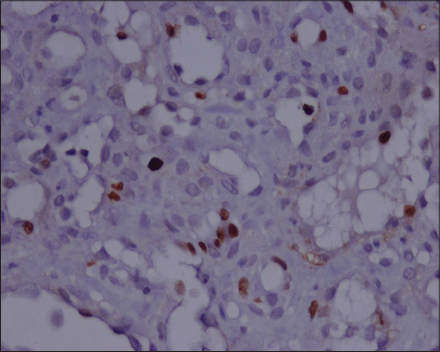 |
| Figure 5: A few cells with nuclear immunopositivity for Ki-67 antibody. The labeling index was low (approximately 3–4%) |
Retiform hemangioendothelioma is a rare distinctive variant of low-grade cutaneous angiosarcoma typically present on the extremities.[1],[2] The term “retiform hemangioendothelioma” was coined to indicate the resemblance of its vascular channels with the rete testis (retiform) and its borderline malignant behavior (hemangioendothelioma), in contrast to the benign angioma and the malignant angiosarcoma.[1] Clinically, it presents as a slowly growing mass, a plaque-like lesion or a dermal or subcutaneous nodule. The differential diagnoses for retiform hemangioendothelioma are Dabska tumor, hobnail hemangioma and angiosarcoma. These conditions can be differentiated from retiform hemangioendothelioma by their morphological and histopathological findings. The most characteristic finding in Dabska tumor is papillary tufts with a central hyaline core lined by hobnail-like endothelial cells protruding into the lumina whereas in retiform hemangioendothelioma, instead of papillary tufts there are some papillary infoldings along with retiform type of blood vessels, which are not seen in Dabska tumor.[3] Hobnail hemangioma is mostly seen in young adults as small erythematous papules surrounded by an ecchymotic halo. On histopathological examination, it reveals elongated vascular structures lined by hobnail-like endothelial cells that are confined to the superficial layers of skin without extending to the deep dermis or subcutaneous tissue and are accompanied by hemosiderin deposits.[4] Finally, angiosarcoma can be easily differentiated from retiform hemangioendothelioma by the presence of nuclear atypia and mitotic figures and the absence of a retiform pattern of blood vessels. Further, angiosarcoma is more invasive than retiform hemangioendothelioma with higher chances of recurrence and metastasis.[5] Retiform hemangioendothelioma has a predilection towards women with the ratio of 2:1,[6 ] mostly present in the second to fourth decade of life with a mean age of 36 years.[1],[6] Local recurrence occurs in 60% of cases.[1] Regional lymphnode metastasis was reported in a single patient and in another patient, it had spread locally to soft tissue.[7] So far, there is one report of death due to retiform hemangioendothelioma.[2] Surgical excision is the most effective treatment.[5] Our patient had a solitary nodule on the left temporal scalp, which is an atypical site. We found only two previous case reports of retiform hemangioendothelioma on the scalp.[2],[8] Immunohistochemically, retiform hemangioendothelioma cells have been reported to react with CD31, CD34 and factorVIII-related antigen.[1] In our case, the tumor cells showed CD34 positivity. The tumor cells were occasionally positive for the cell proliferative marker Ki-67, indicating that a low proliferative potential is a feature of the tumor (approximately 3–4%). We treated our patient surgically and the patient is under regular follow-up for the last 18 months. Till date, the patient has not shown any recurrence at the site of surgery or elsewhere.
Financial support and sponsorship
We are grateful to the financial support provided by the Departments of Dermatology and Pathology, PGIMER, and Dr. RMLH, New Delhi.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Calonje E, Fletcher CD, Wilson-Jones E, Rosai J. Retiform hemangioendothelioma. A distinctive form of low-grade angiosarcoma delineated in a series of 15 cases. Am J Surg Pathol 1994;18:115-25.
[Google Scholar]
|
| 2. |
Zhang G, Lu Q, Yin H, Wen H, Su Y, Li D, et al. Acase of retiform-hemangioendothelioma with unusual presentation and aggressive clinical features. Int J Clin Exp Pathol 2010;3:528-33.
[Google Scholar]
|
| 3. |
Requena L, Kutzner H. Hemangioendothelioma. Semin Diagn Pathol 2013;30:29-44.
[Google Scholar]
|
| 4. |
Trindade F, Kutzner H, Tellechea Ó, Requena L, Colmenero I. Hobnail hemangioma reclassified as superficial lymphatic malformation: A study of 52 cases. J Am Acad Dermatol 2012;66:112-5.
[Google Scholar]
|
| 5. |
Hirsh AZ, Yan W, Wei L, Wernicke AG, Parashar B. Unresectable retiform hemangioendothelioma treated with external beam radiation therapy and chemotherapy: A case report and review of the literature. Sarcoma 2010;2010. pii: 756246.
[Google Scholar]
|
| 6. |
Bhutoria B, Konar A, Chakrabarti S, Das S. Retiform hemangioendothelioma with lymph node metastasis: A rare entity. Indian J Dermatol Venereol Leprol 2009;75:60-2.
[Google Scholar]
|
| 7. |
Mentzel T, Stengel B, Katenkamp D. Retiform hemangioendothelioma. Clinico-pathologic case report and discussion of the group of low malignancy vascular tumors. Pathologe 1997;18:390-4.
[Google Scholar]
|
| 8. |
Botros MF, Abdo I, Foda S, Amer H, Attia N, Saad S,et al. Retiform hemangioendothelioma. Egypt Dermatol Online J 2005;1:1-7.
[Google Scholar]
|
Fulltext Views
3,799
PDF downloads
1,518





