Translate this page into:
Coping strategies and quality of life among patients with chronic psoriasis and eczema/dermatitis
Correspondence Address:
Xing-Hua Gao
Department of Dermatology, No. 1 Hospital of China Medical University, 155N, Nanjing Street, Shenyang 110001
P. R. China
| How to cite this article: Amer AA, Gao XH, Li JH, Qi R, Zhang YJ, Chen HD. Coping strategies and quality of life among patients with chronic psoriasis and eczema/dermatitis. Indian J Dermatol Venereol Leprol 2017;83:699-701 |
Sir,
Psoriasis and eczema/dermatitis are two chronic, relapsing skin diseases commonly seen in the dermatology clinic and have shown increasing prevalence during the past decades.[1],[2] Both disorders are characterized by erythematous, scaly plaques and it may be difficult to differentiate them, especially on hands and feet.[3]
The chronic and irritative nature of psoriasis as well as the intense symptoms of eczema both has shown a significant impact on different aspects of daily life. Long-term treatment of both diseases increases patient's costs leading to many economic and financial difficulties.[4]
Numerous patients with either psoriasis or eczema we encountered in our hospital ( first hospital of China Medical University, China) showed varied degrees of confusion due to the misunderstanding of their conditions, some indicated that their outdoor activities are restricted only to their physician visits, and others were anxious that people or friends may be put-off by their appearance and prefer to avoid them.
Our study is designed to assess coping methods and life quality of psoriasis patients and eczema patients, and their reactions according to different situations. In order to achieve this goal, 77 patients (42 psoriasis and 35 eczema) aged at least 18 years old with disease duration of at least 3 months were evaluated. Coping strategies of the patients were measured using the Chinese language version of the medical coping modes questionnaire (MCMQ), a simple, brief, and easily explained questionnaire designed by Feifel et al. in 1987 to assess coping strategies and associated features of medically ill patients, the questionnaire consists of 20 items which were designed to assess three illness-related coping strategies (confrontation, avoidance, and acceptance-resignation) and is scored using a four-point rating scale ranged between 1 (never) and 4 (very often). Additionally, the quality of life was evaluated using the dermatology life quality index (DLQI); a 10-item questionnaire developed in 1994 by Finlay et al. to assess limitations caused by the impact of skin disease, each item is scored on a four point scale and total score ranges from 0 to 30, a total score of 0-1 is regarded as a normal quality of life, 2-5 as a small effect, 6-10 as a moderate, 11-20 as a large effect, and >20 as an extremely large effect on the quality of life. Higher scores indicate a more severely affected quality of life. Both questionnaires are self-administered, easy to complete, and designed for usage by patients who are over the age of 16 years.
After the exclusion of patients with systemic and/or chronic conditions, the final sample included 42 patients of psoriasis with mean age of 44 years (26 men and 16 women) and 35 patients of eczema with mean age of 49 years (17 men and 18 women). There were no significant differences found in most demographic characteristics in both groups. However, the psoriasis group showed a longer disease duration than the eczema group (10.69 y ± 9.36, 5.67 y ± 6.45, respectively) (P = 0.009). Additionally, the mean score for the disease severity in the psoriasis group (Psoriasis Area and Severity Index, PASI) is 21.76 ± 8.78 (range 4.2-45), and for the eczema group (EASI) was 14.61 ± 6.05 (range 4.9–26.8).
The study showed similar scores in the strategies for both the psoriasis patients and the eczema patients [Figure - 1]. Also, there were similarities in both groups in respect to all subscales of the quality of life index except for symptoms where the eczema patients tend to suffer from itchiness and pain problems more than the psoriasis patients, P < 0.001 [Figure - 2].
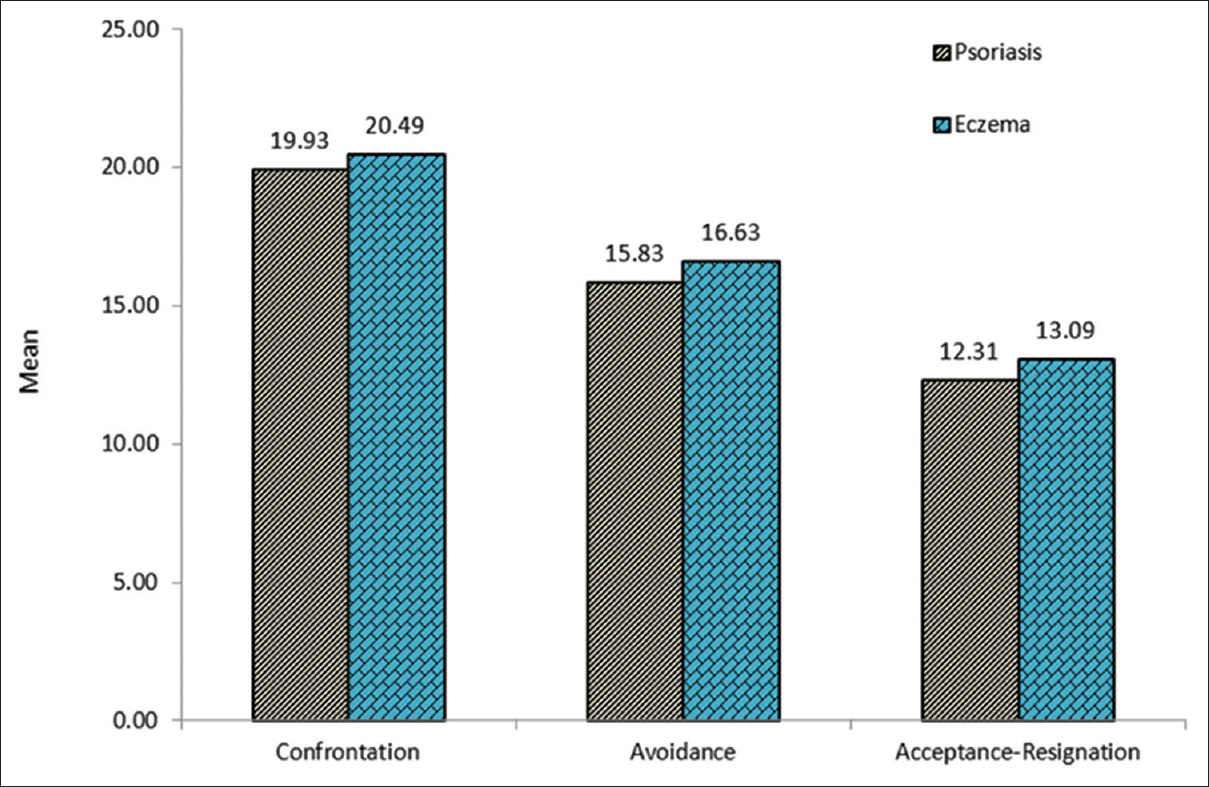 |
| Figure 1: Mean scores for the Medical Coping Modes Questionnaire in both psoriasis and eczema groups |
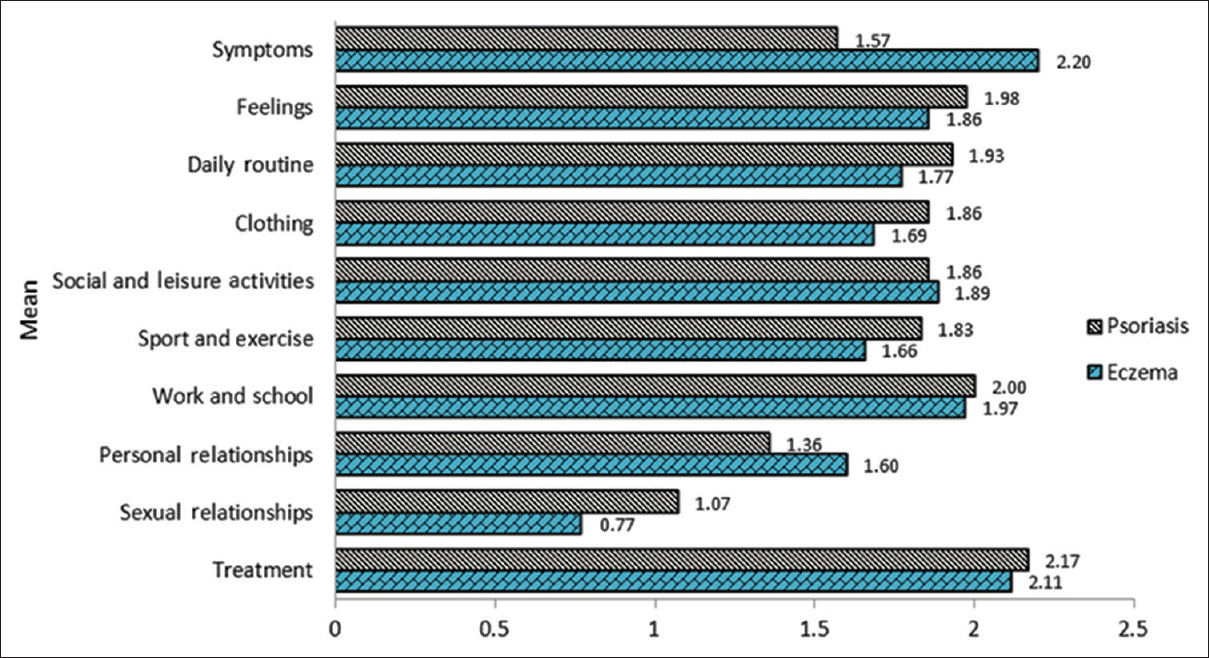 |
| Figure 2: Mean scores for the Dermatology Life Quality Index in both psoriasis and eczema groups |
In general, the study revealed evidence of an impaired quality of life in patients with chronic psoriasis and eczema as the hypothesis predicted. Furthermore, the mean of total score of the DLQI in psoriasis group was 17.62 ± 5.7 ( range 2-27) and 17.51 ± 5.1(range 3-26) for the eczema group, indicating a severe effect of quality of life.
Moreover, both groups revealed a similar range in life quality impact. This similarity could be due to the homogeneity in features regarding degree of annoyance, chronic nature, treatment difficulty, and the recurrence of both diseases.
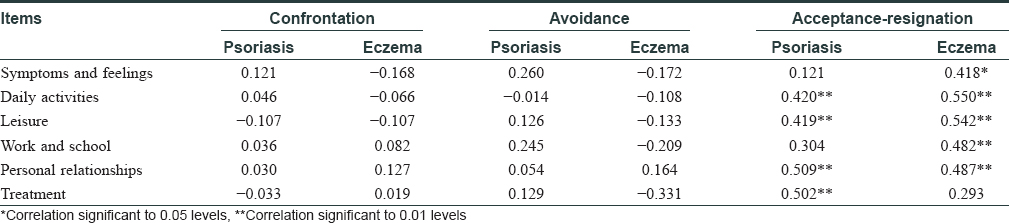
As shown in [Table - 1], we found that the DLQI scores correlated only with the acceptance/resignation component of the medical coping modes questionnaire scores. This implies that patients who gave up on their disease were more likely to have a negative impact on the quality of life, as compared to those adopting a confrontation or avoidance strategies.
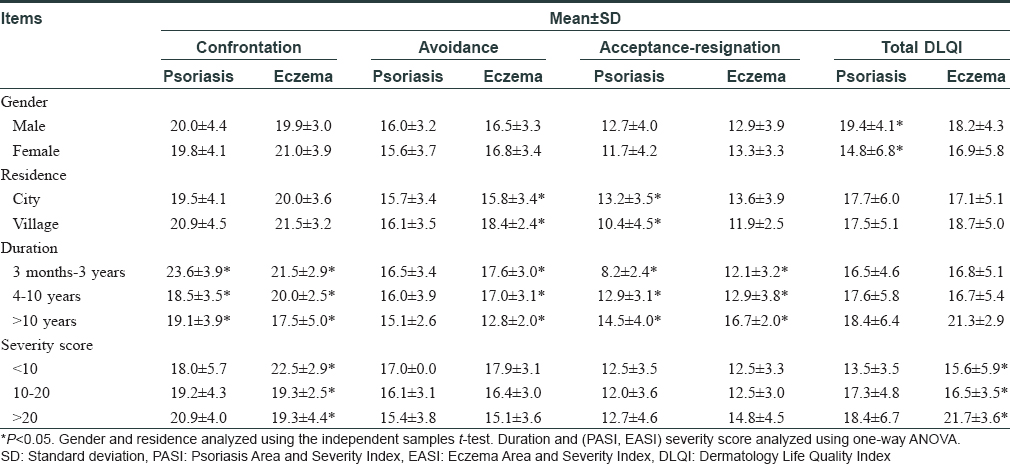
The study revealed no relationship between the coping strategies and patients' gender, age, education level, occupation, or even the monthly income in both groups. However, the urban psoriasis-patients were more ill-fated and conceding to their disease, while villager eczema-patients were more likely to forget and turn away.
As expected, patients with short disease duration in both groups showed more optimism towards treatment and more facing strategy than those with longer duration.
Disease severity showed no impact on psoriasis patients regarding both coping strategies and quality of life. Nonetheless, patients with lower severity scores in the eczema group (eczema area and severity index <10) showed more willingness to face and fight against their condition, P = 0.031.
This study also highlighted that male patients in the psoriasis group experienced more quality of life impairment than females (P = 0.008). While in the eczema group, it showed that high disease severity was associated with a greater impairment in the quality of life (P = 0.011) [Table - 2].
To conclude, both psoriasis and eczema tend to have a notable impact on the patients' quality of life which adversely influences their responding strategies. As a result of their poor quality of life, both groups of patients are likely to adapt the acceptance-resignation as coping style which could increase their sufferings. Specialists are advised to pay more attention to patients in early stages to prevent adverse ramifications. Furthermore, psychological interventions are consequentially as important as physical applications regarding the treatment of both diseases. The exclusion of patients with systemic diseases limited the sample size of this study.
Acknowledgment
This work was supported by Public Welfare Programme, Ministry of Health, China (20120 2013), and innovative research team in universities, Liaoning Bureau of Education (LT2012012).
Financial support and sponsorship
Supported by Public Welfare Programme, Ministry of Health, China (2012 02013).
Conflicts of interest
There are no conflicts of interest.
| 1. |
Gupta R, Debbaneh MG, Liao W. Genetic epidemiology of psoriasis. Curr Dermatol Rep 2014;3:61-78.
[Google Scholar]
|
| 2. |
Deckers IA, McLean S, Linssen S, Mommers M, van Schayck CP, Sheikh A. Investigating international time trends in the incidence and prevalence of atopic eczema 1990-2010: A systematic review of epidemiological studies. PLoS One 2012;7:e39803.
[Google Scholar]
|
| 3. |
Guttman-Yassky E, Nograles KE, Krueger JG. Contrasting pathogenesis of atopic dermatitis and psoriasis – Part I: Clinical and pathologic concepts. J Allergy Clin Immunol 2011;127:1110-8.
[Google Scholar]
|
| 4. |
Lundberg L, Johannesson M, Silverdahl M, Hermansson C, Lindberg M. Quality of life, health-state utilities and willingness to pay in patients with psoriasis and atopic eczema. Br J Dermatol 1999;141:1067-75.
[Google Scholar]
|
Fulltext Views
2,332
PDF downloads
530





