Translate this page into:
Unilateral facial and upper truncal anhidrosis and absence of physiological flushing: A case of idiopathic harlequin syndrome
2 National Skin Centre; Department of General Medicine, Lee Kong Chian School of Medicine, Singapore
Correspondence Address:
Hong Liang Tey
National Skin Centre, 1 Mandalay Road
Singapore
| How to cite this article: Yu Phuan CZ, Tey HL. Unilateral facial and upper truncal anhidrosis and absence of physiological flushing: A case of idiopathic harlequin syndrome. Indian J Dermatol Venereol Leprol 2017;83:740 |
Sir,
Unilateral absence of physiological facial heat-induced flushing and sweating is a very rare and unique presentation. These features characterize the Harlequin syndrome,[1] a rare autonomic disorder, which occasionally also involves the neck, upper thoracic region, and the arm.[1] It results from sympathetic deficits localized to the anhidrotic side, but can involve the parasympathetic neurons in the posterior and ciliary ganglia.[2]
A 13-year-old girl presented at the National Skin Centre, Singapore with unilateral anhidrosis and absence of heat-induced flushing over her left face, neck, and upper chest. Her symptoms started 5 years prior and had remained the same. Her medical history comprised a single afebrile seizure at 12 years of age; she was otherwise well. There were no birth complications or developmental delay. She was not on any medications and had no history of prior surgeries. There was no significant family history.
On examination, her vital signs were normal and there was no drop in postural blood pressure. A detailed neurological examination was unremarkable; specifically, there was no ptosis or miosis and pupils were equally responsive to light and accommodation; deep tendon reflexes were normal. She underwent a thermoregulatory sweat test using a method we have previously described.[3] After exercising in a temperature- and humidity-control room for 20 minutes, an absence of heat-induced vasodilatory response on her left face, neck, upper chest, and arm was observed. Minor starch-iodine test revealed associated unilateral well-demarcated anhidrosis in the same locations [Figure - 1].
 |
| Figure 1: Starch-iodine test after heat-induction revealed well-demarcated unilateral anhidrosis on the left side of the face, neck, chest and arm. There were normal amounts of sweating on the right side of the body and from left T4 dermatome downwards, which had turned the starch-iodine powder admixture purple |
Her complete blood count, blood glucose, thyroid, liver, renal, and electrolyte panels were normal. Chest X-ray with apical lung views, brain magnetic resonance imaging, and electroencephalogram revealed no abnormalities. The patient was counselled on the benign nature of her condition, for which no medical treatment was required.
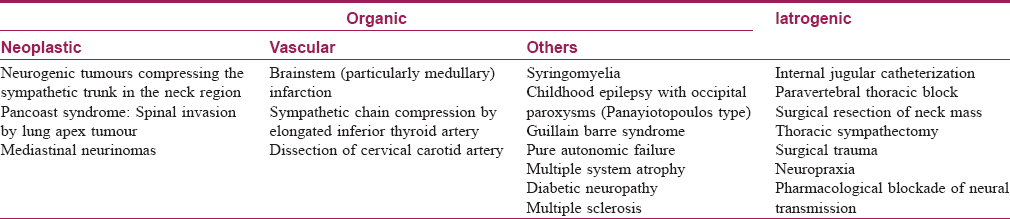
Harlequin syndrome has been increasingly accepted within the spectrum of partial dysautonomias, which affect the facial, and occasionally, brachial pupillary, sudomotor, and vasomotor responses. Physical signs of partial dysautonomias include the harlequin sign, generalized dysautonomia, Holmes–Adie pupils, and Ross and Horner Syndromes, which are found in more than 50% of harlequin syndrome patients.[4] Most cases of Harlequin syndrome in adults are primary in nature,[5] but the majority of childhood cases have been found to be secondary.[4] Such secondary causes of Harlequin syndrome [Table - 1][5] should be excluded before the condition is diagnosed to be primary in etiology. In dermatology literature, only three cases of Harlequin syndrome have been previously reported.
Based on neuroanatomy, the T1 preganglionic sympathetic neurons which innervate the eye were intact, as our patient had no oculomotor symptoms. Sympathetic outflow to the upper extremities and trunk, innervated by the T4 and 5 preganglionic sympathetic neurons, were intact, as sweating was normal, below our patient's chest. Theoretically, harlequin syndrome in our patient may be caused by the occlusion of the anterior radicular artery, which solely supplies the second and third spinal thoracic segment and does not significantly contribute to the overall spinal cord blood flow.[1] However, one limitation of this study is that the identification of this possible abnormalityin vivo will be difficult, as the vessel and the area involved is very small.
Sympathetic cutaneous adrenergic vasoconstrictor nerves are known to co-locate with sympathetic cutaneous vasodilator nerves, and the latter are activated during hyperthermia.[2] Our patient had idiopathic disruption of her left sympathetic fibres, which can result in an increased expression of alpha-adrenoreceptors in denervated vessels. This can sensitize the cutaneous vessels to circulating catecholamines and result in increased vasoconstriction.[2]
With regards to the management of primary Harlequin syndrome, patients should be educated regarding the benign nature of their condition, which requires no medical treatment. Several techniques such as contralateral sympathectomy, botulinum toxin injections, stellate ganglion block, and costotransversectomy for symptomatic relief have been attempted in those who experience debilitating social embarrassment with variable results.[5]
Patients with anhidrosis or cutaneous vascular response abnormalities typically consult dermatologists. We presented a rare and unique presentation of unilateral anhidrosis and absence of physiologic vasodilation on the face due to primary Harlequin syndrome. Dermatologists' knowledge of this syndrome will enable expedient diagnosis and screening of secondary causes in patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Lance JW, Drummond PD, Gandevia SC, Morris JG. Harlequin syndrome: The sudden onset of unilateral flushing and sweating. J Neurol Neurosurg Psychiatry 1988;51:635-42.
[Google Scholar]
|
| 2. |
Charkoudian N. Skin blood flow in adult human thermoregulation: How it works, when it does not, and why. Mayo Clin Proc 2003;78:603-12.
[Google Scholar]
|
| 3. |
Lim JH, Choo W, Chang JH, Tey HL, Chong WS. Application of iodinated starch powder using an atomizer spray gun-A new and effective tool to evaluate hypohidrosis. Skin Res Technol 2016;22:370-4.
[Google Scholar]
|
| 4. |
Bremner F, Smith S. Pupillographic findings in 39 consecutive cases of Harlequin syndrome. J Neuroophthalmol 2008;28:171-7.
[Google Scholar]
|
| 5. |
Willaert WI, Scheltinga MR, Steenhuisen SF, Hiel JA. Harlequin syndrome: Two new cases and a management proposal. Acta Neurol Belg 2009;109:214-20.
[Google Scholar]
|
Fulltext Views
3,958
PDF downloads
1,606





