Translate this page into:
Tinea barbae presenting as kerion
2 Department of Pathology, All India Institute of Medical Sciences, New Delhi, India
Correspondence Address:
Savita Yadav
Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi
India
| How to cite this article: Singh S, Sondhi P, Yadav S, Ali F. Tinea barbae presenting as kerion. Indian J Dermatol Venereol Leprol 2017;83:741 |
Sir,
Inflammatory boggy nodular swellings over the face often pose a diagnostic challenge to the dermatologist. We present a case who presented with inflamed solitary boggy nodular swelling over the beard area and was found to have an unusual etiology on further evaluation.
A 59-year-old male presented with progressively increasing, mildly painful, boggy swelling in the left mandibular area, which was extending to the upper part of the left side of neck since 1 month. There was prominent yellowish crusting in its anterior portion interspersed with multiple follicular pustules [Figure - 1]a. Hair were easily pluckable from the lesion. Gram staining did not reveal any organism. Potassium hydroxide (KOH) mount from pustule showed multiple septate branched hyphae compatible with dermatophytes [Figure - 1]d. However, fungal culture was not ordered. His routine blood investigations including fasting blood sugar were normal, and retroviral status was negative. No lesions were found elsewhere on the skin, mucosae or nails and systemic examination was within normal limits. The source of infection could not be established because there was no history of animal exposure. Histopathology of a skin biopsy specimen revealed moderately dense lymphohistiocytic inflammatory infiltrate with eosinophils and occasional giant cells in both interstitial and perifollicular location [Figure - 2]a and [Figure - 2]b. Periodic acid–Schiff (PAS) and Gomori Methanamine silver (GMS) staining did not reveal any fungal hyphae [Figure - 3]a and [Figure - 3]b. A final diagnosis of inflammatory tinea barbae with kerion-like morphology was made. Patient noticed significant improvement after 3 weeks of 250 mg terbinafine orally once daily [Figure - 1]b. and was stopped after completion of 4 weeks of treatment. Patient reported back after 6 months with complete resolution of the lesion with thin hypertrophic scarring on anterior part and few tiny asymptomatic papules [Figure - 1]c.
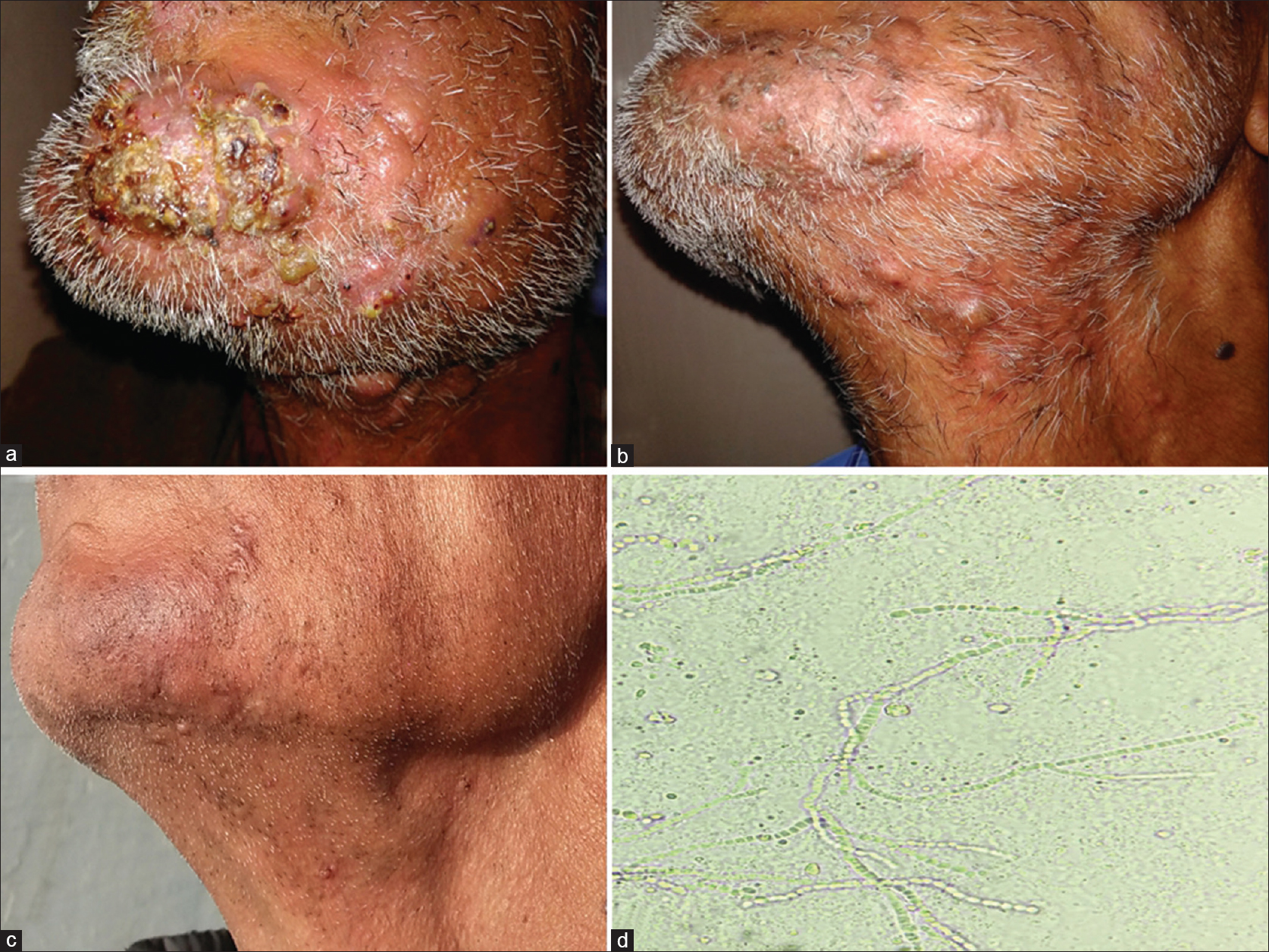 |
| Figure 1: (a) Involvement of the left side of beard area in the form of boggy swelling with prominent crusting and pustulation. (b) Significant improvement after 3 weeks of oral terbinafine. (c) Persistent residual thin scarring at the end of 6 months. (d) Potassium hydroxide scraping showing multiple branched septate hyphae |
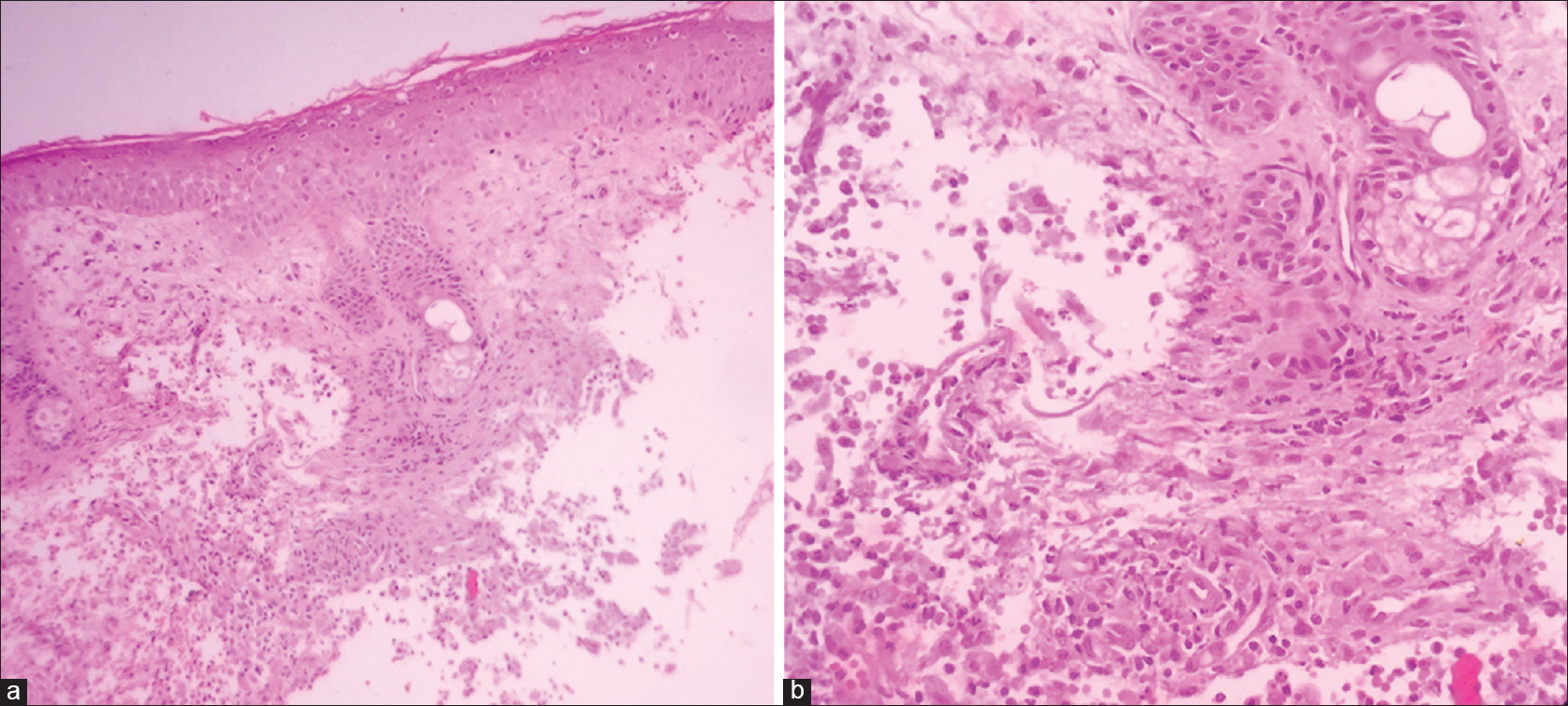 |
| Figure 2: (a) Involvement of dermis in the form of moderately dense infiltrate in both interstitial and perifollicular locations (H and E, ×100). (b) Involvement of dermis in the form of moderately dense infiltrate consisting of lymphocytes, histiocytes, and many eosinophils with occasional giant cells in both interstitial and perifollicular location (H and E, ×400) |
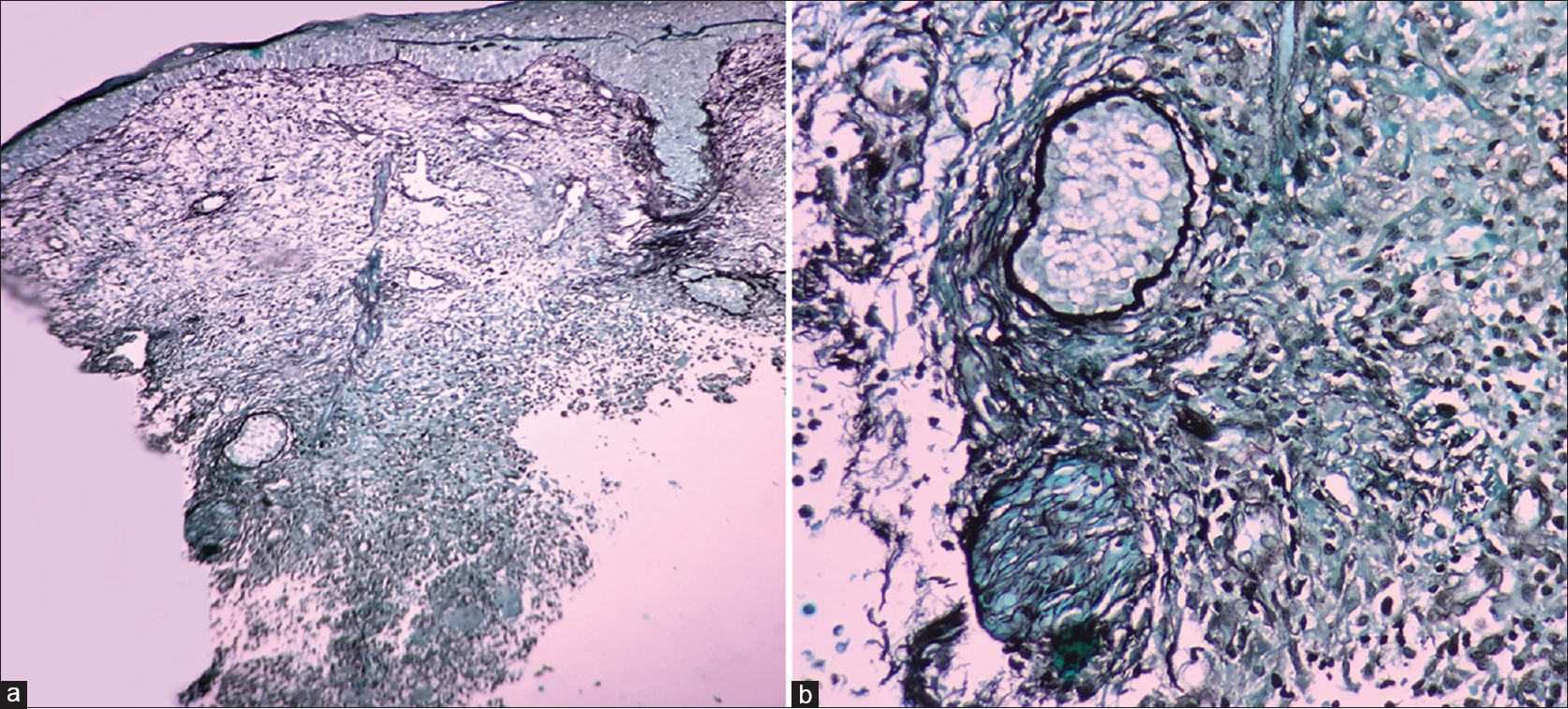 |
| Figure 3: (a and b) Moderately dense inflammatory infiltrates in interstitial and perifollicular location (GMS, ×100 and ×400) |
Tinea barbae is a dermatophytic infection of the beard area of the face and neck. It is seen almost exclusively in young adult males. Frequently, animals (e.g., cattle, horses, cats, dogs) constitute the source of infection.[1] Some authors have reported infection as an autoinoculation from fingernails or tinea pedis.[2] Tinea barbae was observed more frequently in the past and was frequently attributed to transmission due to unsanitary razors used by barbers. Because of this, it was previously termed as barber's itch.[3] Now, because the practice of single-use razors has increased, the disease has become uncommon.[4]
It is most commonly caused by zoophilic species, i.e. Trichophyton verrucosum and T. mentagrophytes.[4] This is responsible for the intense immunological reaction to fungal antigens which play a role in its etiopathogenesis.
Clinically, two types of morphology are described which include inflammatory, deep, kerion-like plaques and noninflammatory superficial scaly lesions resembling tinea corporis or bacterial folliculitis. Kerion-like morphology is the usual presentation, which is seen as an inflammatory plaque with pustules and draining sinuses with crusting over the surface. Hair are loose or broken and depilation is easy and painless. Constitutional symptoms such as fever, malaise, and regional lymphadenopathy can also be present. Noninflammatory superficial tinea barbae presents as flat, scaly erythematous plaque with an active border which can show papules, vesicles, and/or crusts.
The diagnosis is confirmed by KOH mount of skin scarpings and culture. KOH mount shows typical septate hyphae and/or arthroconidia. Culture on Sabouraud dextrose agar with chloramphenicol and cycloheximide takes approximately 3 to 4 weeks. Histopathological examination is rarely necessary for diagnosis. Fungal elements are often missed on hematoxylin and eosin staining and PAS staining may be useful for the same.
Treatment requires oral therapy with either terbinafine 250 mg once daily or itraconazole 200 mg daily for 4 weeks.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Davis DF, Petri WH, Hood AF. Dairy farmer with a rapidly enlarging lip lesion: Tinea barbae. Arch Dermatol 2006;142:1059-64.
[Google Scholar]
|
| 2. |
Kawada A, Aragane Y, Maeda A, Yudate T, Tezuka T, Hiruma M. Tinea barbae due to Trichophyton rubrum with possible involvement of autoinoculation. Br J Dermatol 2000;142:1064-5.
[Google Scholar]
|
| 3. |
Rao R, Prabhu S, George M, Shenoi SD. Inflammatory pruritic nodules and plaques on the face. Indian J Dermatol Venereol Leprol 2007;73:142.
[Google Scholar]
|
| 4. |
Xavier MH, Torturella DM, Rehfeldt FV, Alvariño CR, Gaspar NN, Rochael MC, et al. Sycosiform tinea barbae caused by Trichophyton rubrum. Dermatol Online J 2008;14:10.
[Google Scholar]
|
Fulltext Views
3,262
PDF downloads
2,538





