Translate this page into:
Generalized facial pigmentation: An uncommon presentation of cutaneous lupus erythematosus
2 Department of Dermatology, Hospital Fundación Jiménez Díaz, Madrid, Spain
3 Department of Anatomopathology, Universitary Hospital 12 de Octubre, Madrid, Spain
Correspondence Address:
Alba Calleja Algarra
Department of Dermatology, Universitary Hospital 12 de Octubre, Avenida de Córdoba, S/N, 28041 Madrid
Spain
| How to cite this article: Calleja Algarra A, Aragón Miguel R, Prieto Barrios M, Llamas Martín R, Zarco Olivo C, Haro Ramos MR, Rodríguez Peralto JL, Ortiz Romero PL, Llorente CP. Generalized facial pigmentation: An uncommon presentation of cutaneous lupus erythematosus. Indian J Dermatol Venereol Leprol 2020;86:431-435 |
Sir,
Post-inflammatory hyperpigmentation occurs when the basement membrane of the skin is damaged and this is seen in many inflammatory skin diseases such as lupus erythematosus. It appears in the late phase of many skin lesions and hampers the identification of specific histological features which are characteristic of the triggering disease.[1]
Post-inflammatory pigmentation is widely seen in the periphery of the skin lesions of discoid lupus erythematosus or in the late phase of acute cutaneous lupus erythematosus. However, cutaneous lupus erythematosus presenting predominantly with macular pigmentation is uncommon and often misdiagnosed.[2],[3]
We present six patients who came with diffuse cutaneous facial pigmentation, as the main manifestation of cutaneous lupus erythematosus, showing histological features of cutaneous lupus.
Our patients included four men and two women from Hospital 12 de Octubre and Hospital Fundación Jiménez Díaz (Madrid, Spain) with an average age of 51.33 years and medium-dark phototypes (III-V). Time until diagnosis ranged from 3 months to 10 years.
Clinically, they showed a diffuse, non well-demarcated grey-brown pigmentation, mainly on the forehead, temples and cheeks [Figure - 1], [Figure - 2], [Figure - 3], [Figure - 4]. Patient no. 1 showed involvement of the ear lobes and patient no. 4 had pigmentation in the V area of the neck as well. Five cases showed concomitant facial erythema, although pigmentation was the predominant feature in all of them. In patient no. 4, who had features of systemic lupus erythematosus, the worsening of pigmentation was observed concurrently with disease outbreaks and the onset of other general manifestations, particularly joint-related symptoms. Besides, this patient had subcutaneous nodules in buttocks and thighs concurrently with one of the outbreaks of the systemic disease. Lupus panniculitis was suspected; however, the biopsy did not show any specific finding. All the patients showed positive autoimmunity markers [Table - 1].
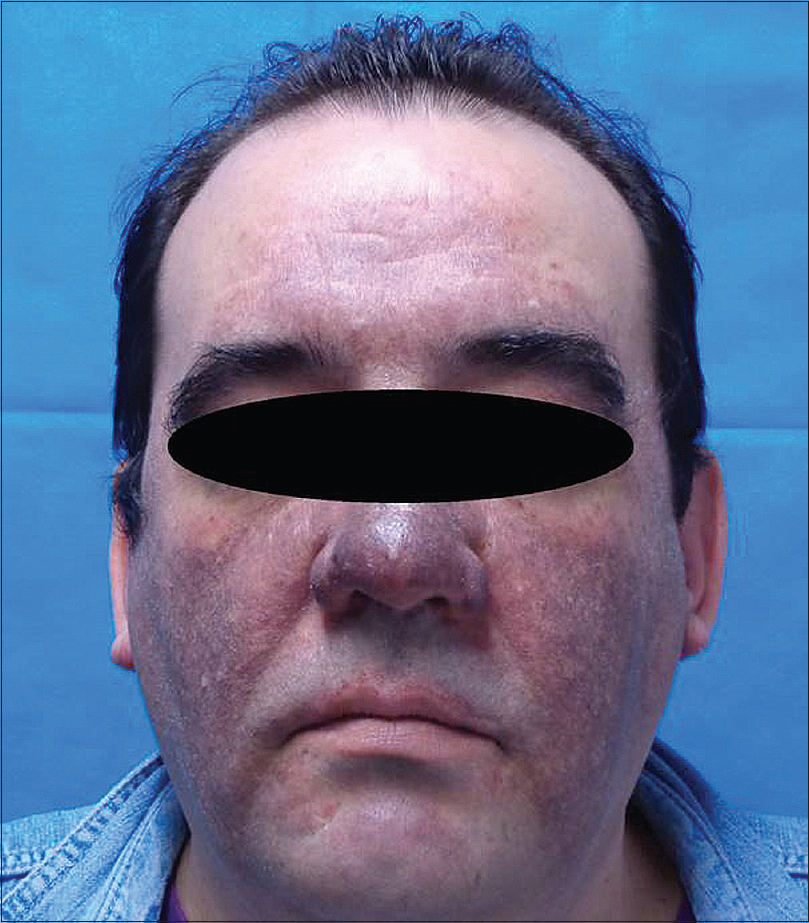 |
| Figure 1: Patient 1 with diffuse slate-grey pigmentation on face with mild erythema |
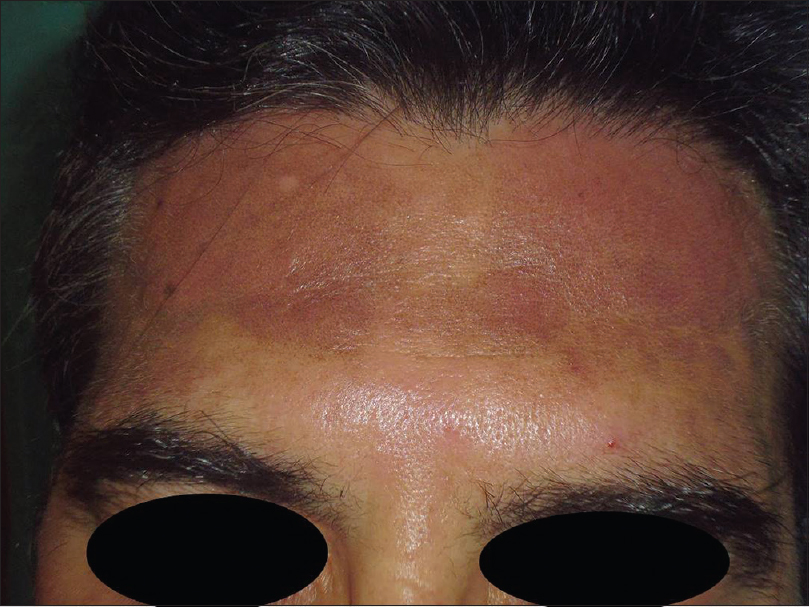 |
| Figure 2: Patient 2 with brownish pigmentation on the forehead with marked erythema |
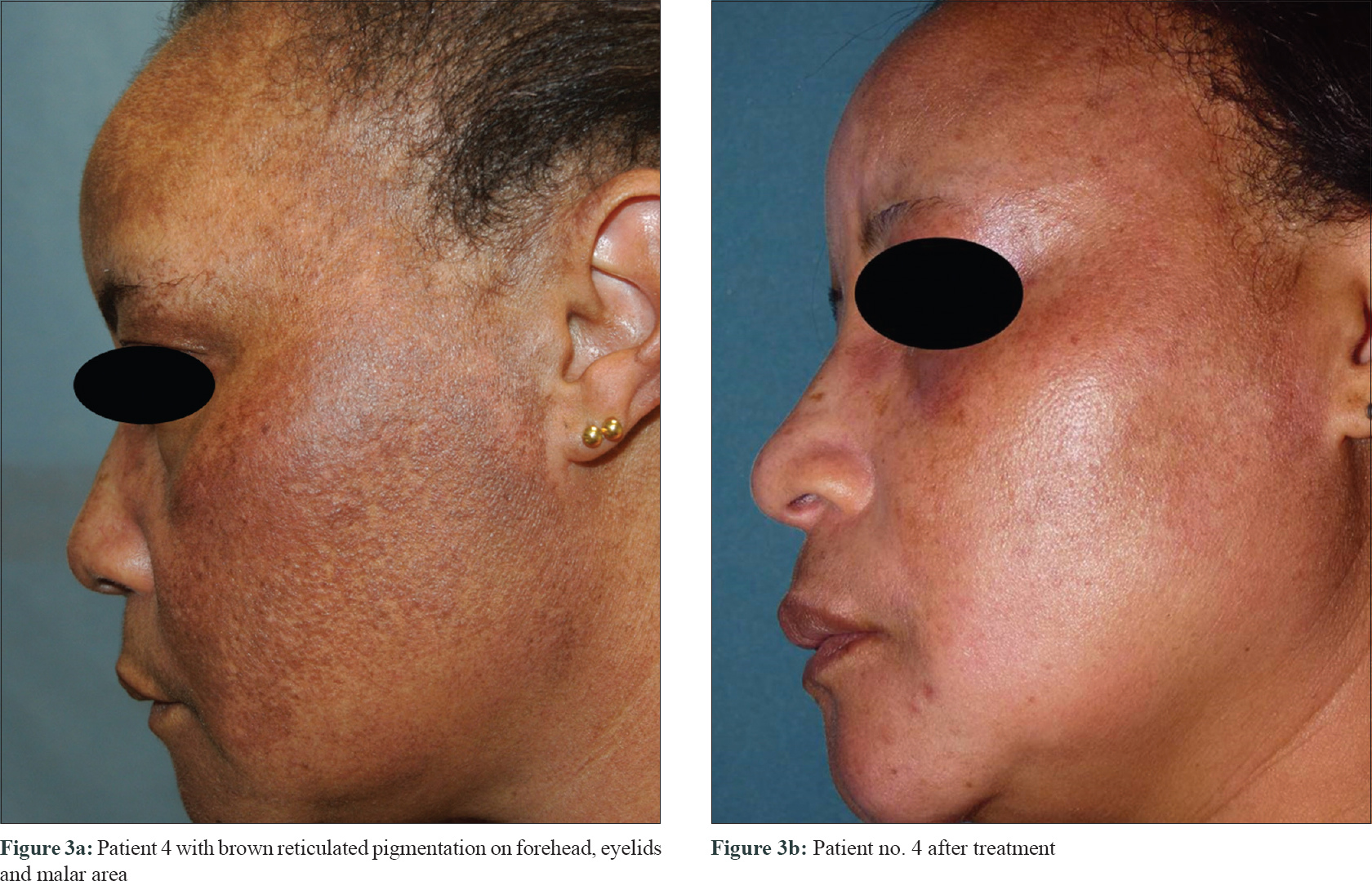 |
| Figure 3: |
 |
| Figure 4: Patient 6 with brownish pigmentation limited to malar and mandibular area with marked skin erythema |
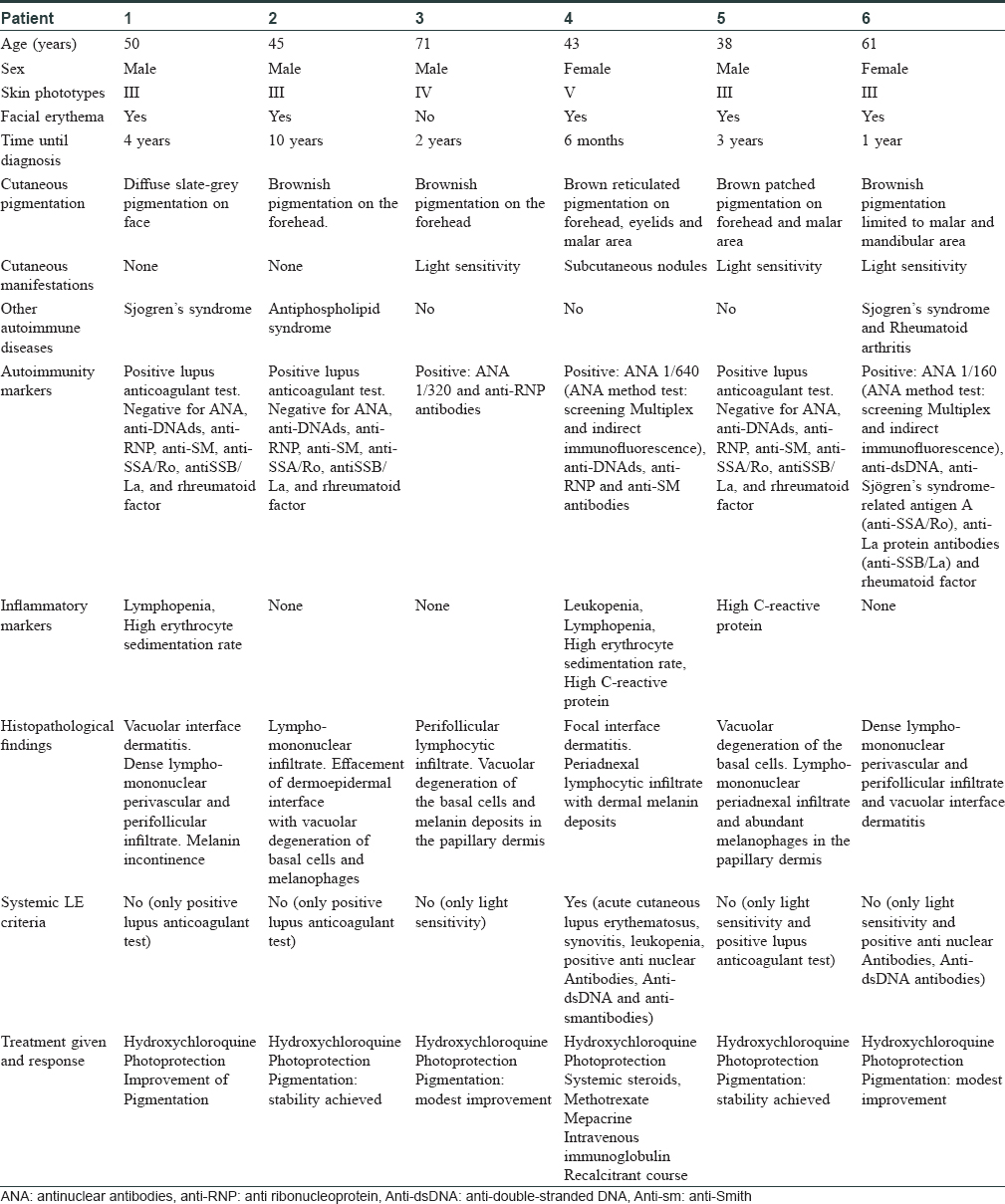
In all cases, drug-induced skin pigmentation was ruled out and epicutaneous patch tests were performed with GEIDAC's (Spanish Research Group on Contact Dermatitis and Cutaneous Allergy) standard battery which showed negative results.
The area of skin which showed maximum pigmentation was selected for skin biopsy. Histological examination was carried out in all cases and it revealed interface dermatitis with vacuolar degeneration of the basal cells, a dense lympho-mononuclear perivascular and perifollicular infiltrate with abundant melanophages in the papillary and high reticular dermis. The colloidal iron technique revealed mucin deposits in the dermis in all cases. This was compatible with pigmented lupus erythematosus [Figure - 5] and [Figure - 6]. More than one biopsy was needed to reach the diagnosis in three of the patients. Due to the nonavailability of the direct immunofluorescence technique at our hospital, this procedure was not performed. Each of the patient received hydroxychloroquine at a dose of 400 mg daily, together with strict photoprotection. Pigmentation on the forehead of patient no. 1 improved with hydroxychloroquine and strict photoprotection by wearing a hat. Pigmentation also improved in patient no. 3, but in rest of the patients pigmentation remained unchanged. Patient no. 4 had a recalcitrant clinical course which was controlled only with intravenous immunoglobulin infusions. She received 16 monthly cycles of intravenous immunoglobulin at a dose of 400 mg/kg/day for 5 consecutive days, achieving non-pregression of the facial pigmentation [Figure - 3]b and [Figure - 3]b.
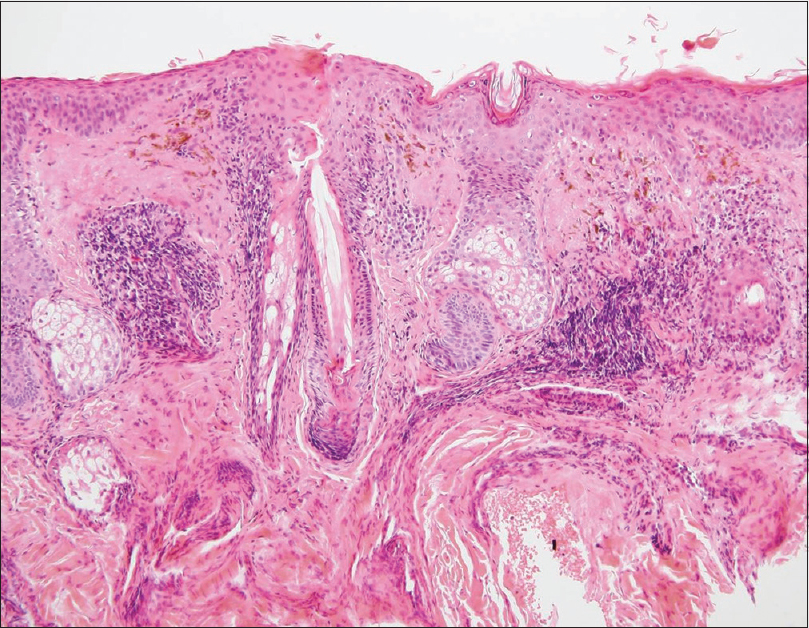 |
| Figure 5: Patient 1: Histopathological examination showing vacuolar interface dermatitis with dense lympho-mononuclear perivascular and perifollicular infiltrate and melanin incontinence (H and E, ×40) |
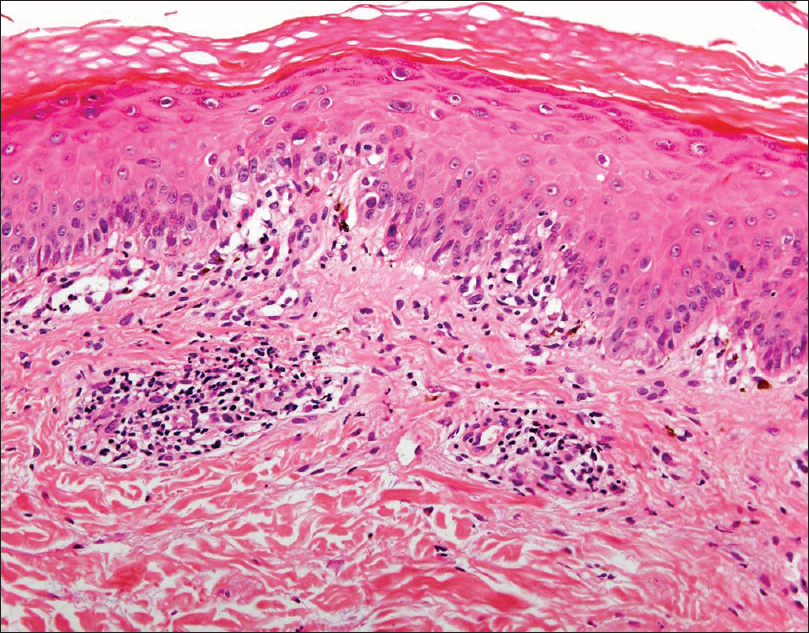 |
| Figure 6: Patient 4: Histopathological examination showing focal interface dermatitis and superficial perivascular lymphocytic infiltrate in papillary dermis with melanin deposits (H and E, ×400) |
Although not often recognized, cutaneous lupus erythematosus may present itself with diffuse facial pigmentation as the predominant disease manifestation. Boyd reported eleven patients who presented with solitary pigmented macules with histological features of discoid lupus erythematosus. These authors conclude that this peculiar presentation occurs in older patients and shows a good response to topical corticosteroids.[4] Later, Taddio et al. reported the case of a 14-year-old girl with diffuse facial pigmentation showing histological characteristics of cutaneous lupus erythematosus in the context of a first systemic disease outbreak which was resolved with specific treatment.[5]
Recently, Khullar et al. reported three patients with generalized brownish-grey facial pigmentation with a diagnosis of pigmented lupus erythematosus.[6]
Reaching this diagnosis can be tricky and other causes of post-inflammatory pigmentation such as Riehl's melanosis, lichen planus pigmentosus and drug-related pigmentation should be included in the differential diagnosis. It is especially relevant to exclude hydroxychloroquine-associated pigmentation since it can lead to discontinuation of a beneficial treatment. Histopathological examination is the key and would show granular deposits of yellow-brown pigment and no inflammation.
We believe our patients have a true form of cutaneous lupus erythematosus whose main dermatological manifestation is pigmentation. Our series suggests that this feature is more common among patients with medium-dark phototypes and being the predominant skin manifestation it could be a marker of cutaneous lupus activity in such patients. There is a great clinical variability in the degree and distribution of pigmentation. The most common pigmentation pattern is a spotted or reticular brown pigmentation on the forehead, temples and malar areas. However, sometimes the lesions have a scattered pattern. This heterogeneity makes the patient's clinical context and skin biopsy essential for diagnosis.
In conclusion, when we come across a patient with generalized facial pigmentation, pigmented lupus erythematosus should always be consdered and histological evaluation should be done to confirm this diagnosis. Dermatologists should be aware of this possibility since it can be the only feature of lupus erythematosus.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Hejazi EZ, Werth VP. Cutaneous lupus erythematosus: An update on pathogenesis, diagnosis and treatment. Am J Clin Dermatol 2016;17:135.
[Google Scholar]
|
| 2. |
Walling HW, Sontheimer RD. Cutaneous lupus erythematosus: Issues in diagnosis and treatment. Am J Clin Dermatol 2009;10:365-81.
[Google Scholar]
|
| 3. |
Obermoser G, Sontheimer RD, Zelger B. Overview of common, rare and atypical manifestations of cutaneous lupus erythematosus and histopathological correlates. Lupus 2010;19:1050-70.
[Google Scholar]
|
| 4. |
Boyd AS. Localized chronic cutaneous lupus erythematosus masquerading as pigmented lesions: A new clinical subset? Lupus 2006;15:292-5.
[Google Scholar]
|
| 5. |
Taddio A, Franzil A, Lepore L. Postinflammatory hyperpigmentation (PIH): The presenting sign of systemic lupus erythematosus. Clin Exp Rheumatol 2008;26:156.
[Google Scholar]
|
| 6. |
Khullar G, De D, Narang T, Saikia UN, Saikia B, Handa S. Pigmented macular variant of chronic cutaneous lupus erythematosus: An under-recognized subset in dark skin. Clin Exp Dermatol 2017;42:793-5.
[Google Scholar]
|
Fulltext Views
9,804
PDF downloads
2,660





