Translate this page into:
Alexandrite (755 nm) laser hair removal therapy reduces recurrence rate of pilonidal sinus after surgery
Correspondence Address:
H Jorn Bovenschen
Department of Dermatology, Máxima Medical Center Eindhoven, De Run 4600, P. O. Box 7777, 5500 MB, Veldhoven, Eindhoven
The Netherlands
| How to cite this article: Luijks HG, Luiting-Welkenhuyzen HA, Greijmans EG, Bovenschen H J. Alexandrite (755 nm) laser hair removal therapy reduces recurrence rate of pilonidal sinus after surgery. Indian J Dermatol Venereol Leprol 2020;86:451-453 |
Sir,
Pilonidal sinus is characterized by chronic abscess and sinus formation in the natal cleft region. Excessive hair growth has a pivotal pathogenetic role due to the penetration of broken terminal hairs into the subcutaneous tissue with subsequent inflammatory granuloma development and potential secondary infection. Primary treatment of pilonidal sinus is generally a surgical procedure which is often followed by a recurrence with relapse rates as high as up to 30%. 1 Hence, patients may benefit from permanent laser hair removal. The 755nm Alexandrite laser is one of the most effective hair removal lasers available. 2 We performed a retrospective study to determine the recurrence rate of pilonidal sinus, safety issues and patient satisfaction of Alexandrite laser hair removal therapy post-surgery.
Questionnaires were sent by postal mail to 153 consecutive patients treated between 2007 and 2016 with Alexandrite laser. The questionnaire contained queries on four domains: patient characteristics/demographic data, pilonidal sinus recurrences, safety issues and patient satisfaction. Patients reported on 5 or 10-point Likert scales; efficacy scale for hair removal: 1 = not effective to 10 = extremely effective; pain scale: 1–10; 0 = no pain, 10 = unbearable pain; hair extent scale: 0 = no hair, 1 = mild, 2 = moderate, 3 = severe, 4 = excessive. All patients had surgical pilonidal sinus treatment and were referred for laser hair removal after the surgical wound had completely healed. Treatments were standardized (same laser therapists, same laser, standard settings) with a 755nm wavelength Alexandrite laser (GentleMax, Candela); spot-size 15–18mm, pulse duration 3–10ms, energy 18–26 J/cm[2], dynamic cooling device settings 30/20. The treatment interval was 6–8 weeks. Safety and recurrences were assessed by reviewing patients' medical records. All patient characteristics are included in [Table - 1].
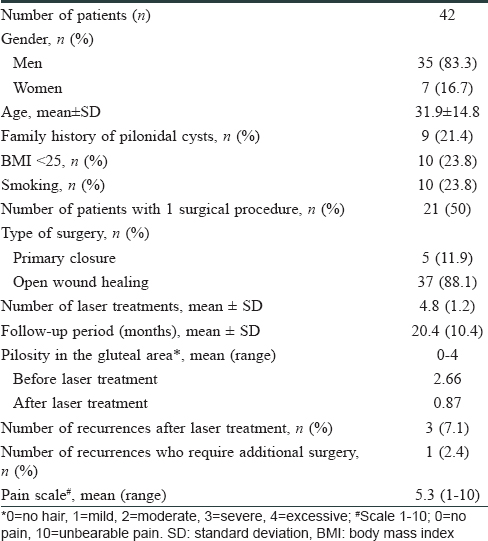
Forty two questionnaires (27.5%) were eligible for analyses. All patients were Caucasian with Fitzpatrick skin type I–III. Half of the patients (50%) were treated only once for pilonidal sinus in the past, whereas the other 21 (50%) patients had a history of recurrent pilonidal sinus. In 37 (88%) patients, the surgical wound healed with secondary granulation. The mean number of necessary laser treatments to achieve full hair removal was 4.8 ± 1.2 (mean ± SD)[Table - 2]. Alexandrite laser treatment was highly effective in reducing hair growth in all patients[Figure - 1]a. The extent of hair growth reported on a 5-point Likert scale (mean ± SD) was 2.7 ± 0.9 before Alexandrite laser treatment and 0.9 ± 0.8 after Alexandrite laser treatment. Recurrence of the pilonidal sinus was reported by three (7.1%) patients but only one (2.4%) patient required additional surgery. Mean pain score during treatment (± SD) was 5.3 ± 2.0. Only two (4.8%) patients reported residual hyperpigmentation. No other side effects or complications were reported [Figure - 1]b. All patients would recommend Alexandrite laser hair removal post-surgery [Figure - 1]c.
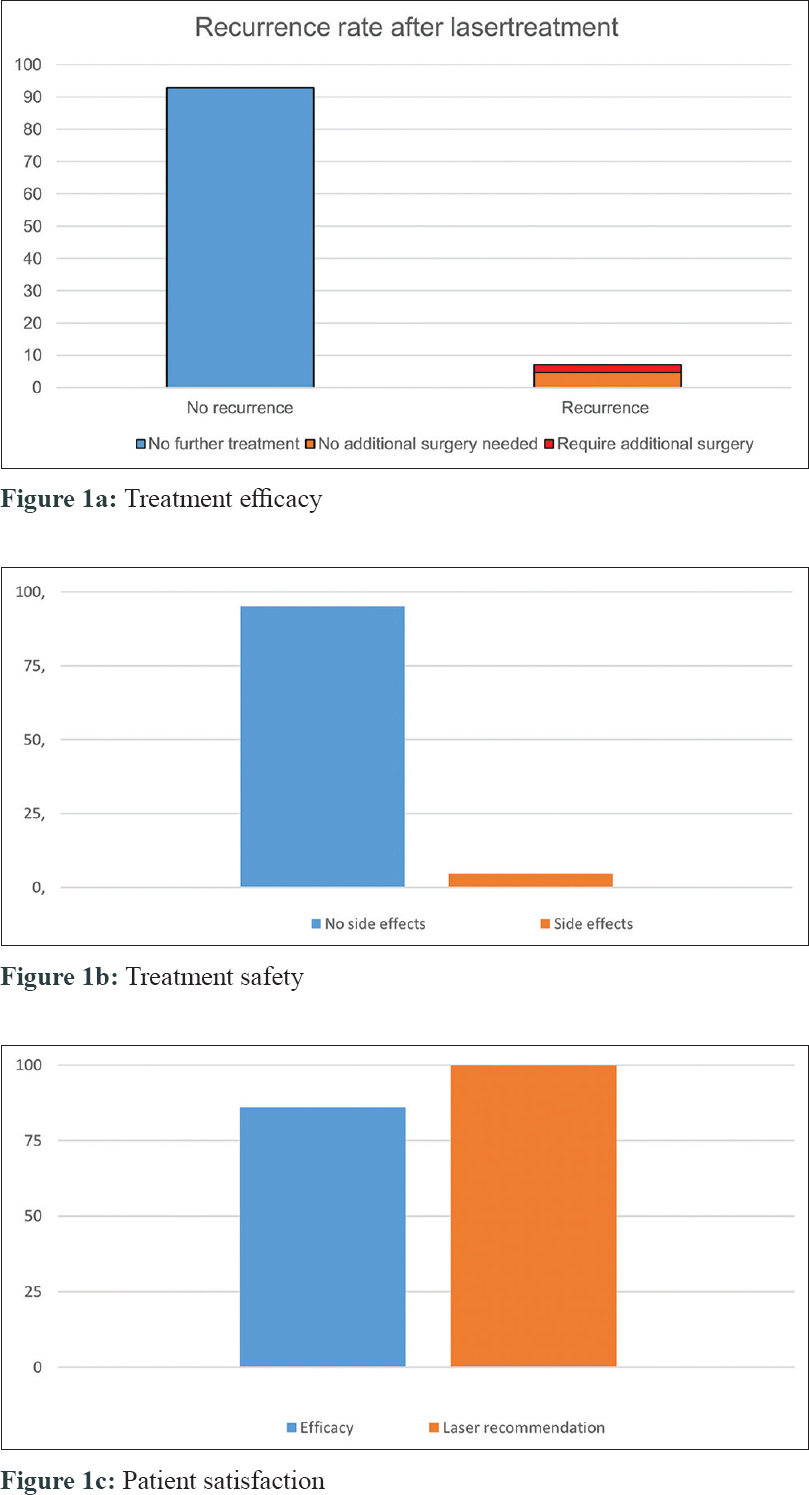 |
| Figure 1: |
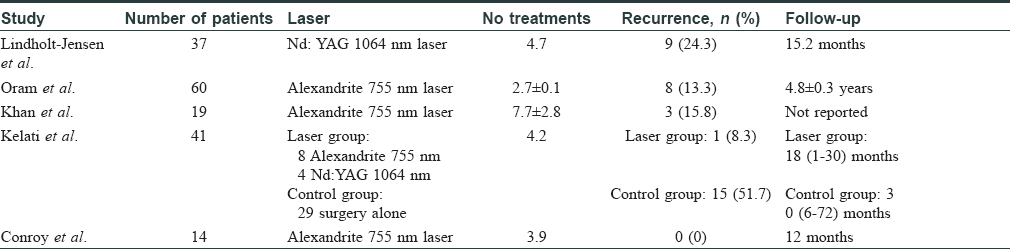
In literature, several laser hair removal studies have previously been conducted with variable results. Oram et al. reported a 13.3% recurrence rate of pilonidal sinus after a mean number of 2.7 Alexandrite laser treatments. 3 Recurrence rate after excision and primary closure was high (38%) and excision and flap reconstruction provided the best results with a relapse rate of only 7.3%. Therefore, it is attractive to speculate that the choice of surgical technique influences pilonidal sinus recurrence rate. In another study, three pilonidal sinus recurrences were observed out of 19 patients (15.8%) treated with Alexandrite laser. 2 In a retrospective case-control study, comparing Alexandrite laser and Nd: YAG laser hair removal after pilonidal sinus surgery versus surgery alone, the recurrence rate was 8.3% for the “laser after surgery” group and 51.7% in the “surgery alone”group. 4 further Mutus et al. showed zero recurrences in 32 patients treated with laser versus 21/268 (7.8%) relapses without laser hair removal. [5] The results of our present study show relatively high efficacy in preventing pilonidal sinus relapse after surgery and the beneficial effects of laser therapy are in concordance with previous studies. A literature overview is presented in [Table - 1].
In general, Alexandrite lasers are not usually used in darker skin as they are shorter wavelengths and prone to adverse effects. In the present study, we only treated patients with Fitzpatrick's skin type I–III. However, in our center, we use the same laser for people with skin types IV and V with the following settings without any complications and with similar success rates: IV: spot-size 15, pulse duration 3ms, energy 20–24 J/cm[2], dynamic cooling device settings 40/20; V: spot-size 15, pulse duration 10ms, energy 12–18 J/cm[2], dynamic cooling device settings 40/20. We are not familiar withtreating patients with Fitzpatrick skin type VI.
The strength of the present study includes a large number of patients who were consecutively referred by surgeons post-pilonidal sinus surgery, as well as standardization of the Alexandrite laser treatment procedure. Limitations of our study are the retrospective study design with its potential biases, for example, recall bias is possible as patients may not recall the pain scores after a longer period. Furthermore, the low number of respondents to the questionnaire (27.5%) and the variable follow-up period are issued to consider.
Notably, we observed a 100% score with respect to patient satisfaction: all patients would recommend Alexandrite laser hair removal to others. The excellent treatment tolerance/safety profile and limited pain/side effects make Alexandrite laser hair removal therapy ultimately suited as a secondary prevention measure after surgery for pilonidal sinus.
In conclusion, post-surgery 755 nm Alexandrite laser hair removal therapy is effective and highly satisfactory for pilonidal sinus patients in reducing recurrence rates, although prospective analysis is needed to confirm our results.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Doll D, Krueger CM, Schrank S, Dettmann H, Petersen S, Duesel W. Timeline of recurrence after primary and secondary pilonidal sinus surgery. Dis Colon Rectum 2007;50:1928-34.
[Google Scholar]
|
| 2. |
Khan MA, Javed AA, Govindan KS, Rafiq S, Thomas K, Baker L, et al. Control of hair growth using long-pulsed alexandrite laser is an efficient and cost effective therapy for patients suffering from recurrent pilonidal disease. Lasers Med Sci 2016;31:857-62.
[Google Scholar]
|
| 3. |
Oram Y, Kahraman F, Karincaoǧlu Y, Koyuncu E. Evaluation of 60 patients with pilonidal sinus treated with laser epilation after surgery. Dermatol Surg 2010;36:88-91.
[Google Scholar]
|
| 4. |
Kelati A, Lagrange S, Le Duff F, Lacour JP, Benasaid R, Breaud J, et al. Laser hair removal after surgery vs. surgery alone for the treatment of pilonidal cysts: A retrospective case-control study.J Eur Acad Dermatol Venereol 2018;32:2031-3.
[Google Scholar]
|
| 5. |
Mutus HM, Aksu B, Uzun E, Gulcin N, Gercel G, Ozatman E, et al. Long-term analysis of surgical treatment outcomes in chronic pilonidal sinus disease. J Pediatr Surg 2018;53:293-4.
[Google Scholar]
|
Fulltext Views
6,338
PDF downloads
2,545





