Translate this page into:
Multiple inguinal basal cell carcinomas in the setting of intertrigo
2 Department of Dermatology, The University of Texas MD Anderson Cancer Center, Houston, Texas, USA
Correspondence Address:
Michael R Migden
Department of Dermatology, The University of Texas MD Anderson Cancer Center, 1400 Pressler Street, Unit 1452, Houston, Texas 77030
USA
| How to cite this article: Aria AB, Rosenbaum LE, Migden MR. Multiple inguinal basal cell carcinomas in the setting of intertrigo. Indian J Dermatol Venereol Leprol 2020;86:469 |
Sir,
Genital basal cell carcinoma is an uncommon entity, which may be triggered by certain factors like poor hygiene, longstanding local skin irritation or previous radiotherapy. We present an interesting case of multiple basal cell carcinomas involving the left groin in the setting of intertrigo.
A 72-year-old male presented to his dermatologist with a discrete pearly telangiectatic papule in the left inguinal fold within a background area clinically consistent with intertrigo. The patient had a history of two basal cell carcinomas on the face removed 8–10 years ago and a 1-year history of intertrigo in the left inguinal fold treated with clotrimazole–betamethasone. Biopsy of the discrete pearly papule revealed basal cell carcinoma. He then developed two new biopsy-proven lesions adjacent to the original basal cell carcinoma. Due to concern for locoregional metastasis, he was referred to our clinic for further evaluation.
There was no relevant family history or clinical evidence to suggest a genetic disorder, such as basal cell nevus syndrome. Physical examination revealed a 3.2 × 2.0 cm pink, scaly, thin plaque in the left groin along with a 1.0 × 0.8 cm pink, scaly plaque located distally and a 1.6 × 0.8 cm pink plaque located proximally. Inguinal lymph nodes were non palpable. A computed tomography scan also ruled out pathologically enlarged lymph nodes.
We performed Mohs micrographic surgery for all the lesions, as metastasis was not evident. Histopathologic findings of all lesions demonstrated atypical aggregates of basaloid cells, consistent with the diagnosis of basal cell carcinoma [Figure - 1]. At the time of surgery, background erythema with mild scale was noted in the left inguinal fold on opposing surfaces suggestive of intertrigo [Figure - 2]. We performed surgical excision along with tissue repair for all the lesions, which healed satisfactorily within 1 month. The patient was started on topical ketoconazole (antifungal agent) in the groin to treat his persistent intertrigo [Figure - 3]. Seven weeks later (about 3 months after surgery), we observed complete healing of the surgical areas along with clearing of the intertrigo [Figure - 4].
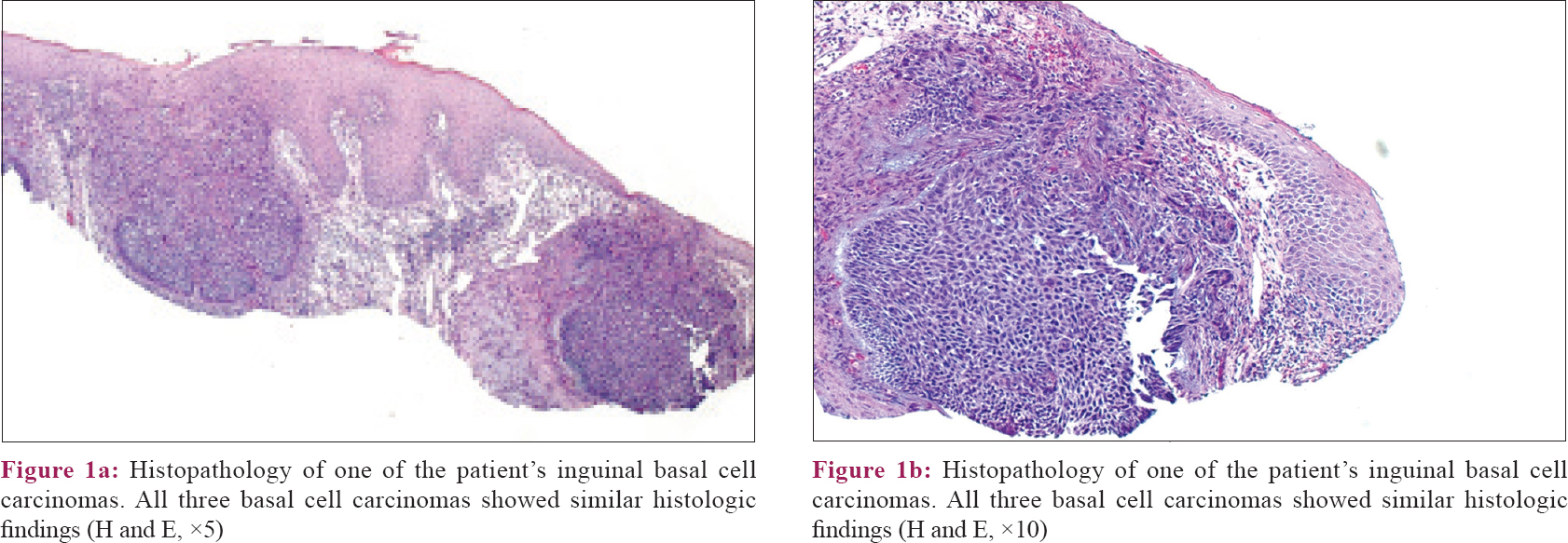 |
| Figure 1: |
 |
| Figure 2: Three basal cell carcinomas outlined with a skin-marking pen in the left inguinal fold. Surrounding erythema and mild scale were noted in a kissing distribution in the inguinal fold |
 |
| Figure 3: One month after surgery, the area was healing well. Significant erythema, scale, and satellite pink macules again in a kissing distribution in the left inguinal fold were noted |
 |
| Figure 4: Three months after surgery, the patient's surgical sites were well-healed and his intertrigo had cleared with the use of three times per week ketoconazole shampoo |
Sun-protected areas of the body rarely develop basal cell carcinoma and its etiology in such anatomic locations is unclear. Betti et al. evaluated 3254 consecutive basal cell carcinomas and found head and neck to be the most common site [1766 (54.3%)], followed by trunk [1113 (34.2%)] limbs [362 (11.1%)] and genitalia [13 (11.1%)].[1] Our patient's risk factors included age, prior history of basal cell carcinoma on the face, and possibly chronic skin inflammation due to intertrigo. It has been suggested that local factors like concave shape, reduced skin tension, and skin folds favour the development of basal cell carcinoma in sun-protected areas like axillae and groin (as in our case).[2],[3] Heckmann et al. concluded that reduced dermal thickness, altered connective tissue arrangements, altered expression of metalloproteinases, and reduced numbers of integrins at these sites may also contribute to the development of this disorder.[2]
Intertrigo is an inflammatory condition most commonly due to a Candida infection and which involves skin folds such as the inguinal folds, axillae, intergluteal folds, and scrotum. It can be speculated that pre-existing intertrigo in our patient could have increased the risk of basal cell carcinoma in a sun-protected area due to chronic local skin inflammation and irritation. Hau et al. reported Candida albicans induced robust activation of T-helper 17 cells, resulting in increased release of interleukin (IL)-17 and IL-22.[4]
Nardinocchi et al. demonstrated a high infiltration of IL-17 + and IL-22 + T-cells in basal cell carcinomas.[5] IL-17 and IL-22 also increased proliferation and migration of the basal cell carcinoma cell line M77015 in anin vitro study.[5] Several reports suggest that IL-17 upregulates nuclear factor kappa light chain enhancer of activated B cells' (NFκB) signaling and IL-22 activates the signal transducer and activator of transcription 3 (STAT3) pathway, which are molecular signaling pathways known to promote carcinogenesis of basal cell carcinoma.[5],[6]
Based on these data, we suggest that Candidal intertrigo led to increased levels of IL-17 and IL-22 in our patient's inguinal area through a natural immune response, thus creating an inflammatory microenvironment favorable for basal cell carcinoma development. However, this proposed relationship warrants further investigation and study. To conclude, physicians should be aware of potential risk factors which may modify a patient's immune profile, altering their risk for developing basal cell carcinoma in sun-protected areas.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Betti R, Radaelli G, Bombonato C, Crosti C, Cerri A, Menni S. Anatomic location of basal cell carcinomas may favor certain histologic subtypes. J Cutan Med Surg 2010;14:298-302.
[Google Scholar]
|
| 2. |
Heckmann M, Zogelmeier F, Konz B. Frequency of facial basal cell carcinoma does not correlate with site-specific UV exposure. Arch Dermatol 2002;138:1494-7.
[Google Scholar]
|
| 3. |
LeSueur BW, DiCaudo DJ, Connolly SM. Axillary basal cell carcinoma. Dermatol Surg 2003;29:1105-8.
[Google Scholar]
|
| 4. |
Hau CS, Tada Y, Kanda N, Watanabe S. Immunoresponses in dermatomycoses. J Dermatol 2015;42:236-44.
[Google Scholar]
|
| 5. |
Nardinocchi L, Sonego G, Passarelli F, Avitabile S, Scarponi C, Failla CM, et al. Interleukin-17 and interleukin-22 promote tumor progression in human nonmelanoma skin cancer. Eur J Immunol 2015;45:922-31.
[Google Scholar]
|
| 6. |
Feehan RP, Shantz LM. Molecular signaling cascades involved in nonmelanoma skin carcinogenesis. Biochem J 2016;473:2973-94.
[Google Scholar]
|
Fulltext Views
6,033
PDF downloads
1,943





