Translate this page into:
Severe abdominal wall defect leading to dehiscence in focal dermal hypoplasia (Goltz syndrome)
Correspondence Address:
Nilendu Sarma
PN Colony, Sapuipara, Bally, Howrah - 711 227, West Bengal
India
| How to cite this article: Sarma N, Chakraborty S, Neogi S, Hansda S. Severe abdominal wall defect leading to dehiscence in focal dermal hypoplasia (Goltz syndrome). Indian J Dermatol Venereol Leprol 2015;81:188-190 |
Sir,
Focal dermal hypoplasia (FDH), Goltz syndrome, or Goltz-Gorlin syndrome (OMIM #305600) is a rare X-linked dominant disease. Mutation in the PORCN gene (Xp11.23) causes defective Wnt signaling and results in widespread dysplasia of ectoderm and mesoderm. [1],[2] The most distinctive change is skin atrophy that appears as streaky atrophic plaques, unilateral or bilateral, along the Blaschko′s lines. Atrophic plaques contain dermal fat dysplasia and may develop nodular outpouching. Other classical changes are papillomatous growths around lips, anus, and eyes, patchy alopecia, aplasia cutis, palmoplantar hyperkeratosis and hyperhidrosis, abnormalities in the bones and eyes, presence of hernias, and a typical facial appearance. Herein, we report two cases of focal dermal hypoplasia with large and extreme abdominal wall dehiscence.
The first case was a 2-month-old male child who was delivered vaginally and born at term with low birth weight to non-consanguineous parents. He presented with respiratory distress and an extremely thin abdominal wall with bulged out intra-abdominal organs. There were multiple, cribriform, depigmented, atrophic, small plaques over the trunk, limbs, and face along the Blaschko′s lines. In addition, sternal cleft, cleft palate and lip, syndactyly of multiple toes of both feet, and lobster claw deformity of the right foot were present [Figure - 1]. There were no signs of neurological abnormality or any malignancy. Histological examination of a skin biopsy from the atrophic plaque on abdomen revealed thinned out dermis with separated sparse collagen with herniation of the subcutaneous fat extending into the dermis and reaching up to the subepidermal level [Figure - 2].
 |
| Figure 1: Images of the first patient showing: (A) large area of abdominal wall dehiscence that has been operated; (B) many hypopigmented atrophic plaques along Blaschko's lines on the lateral abdominal wall; (C) lobster claw deformity in the right foot; (D) syndactyly in the right foot |
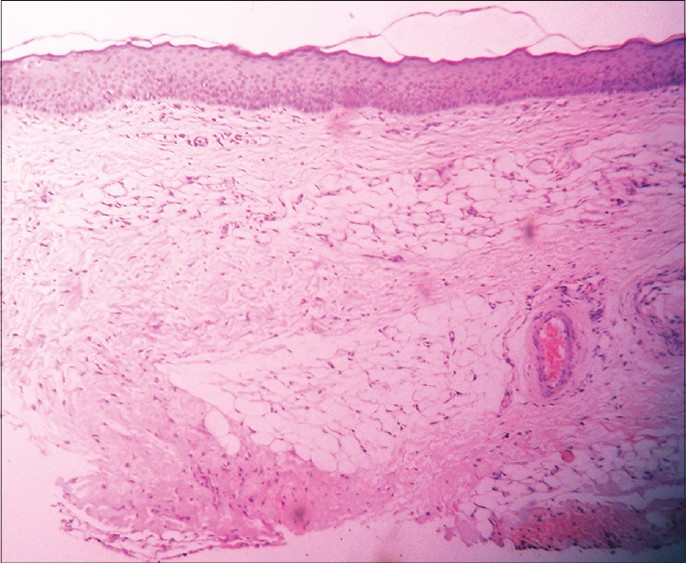 |
| Figure 2: Abdominal skin of the first patient shows grossly thin dermis. Superficial and mid-dermis show fatty herniation with collection of mature adipocytes and occasional telangiectatic blood vessels (H and E, ×100) |
The second case was a 4-month-old female child (born to non-consanguineous parents) who presented with an extremely thin membranous lower abdominal wall below the umbilicus. There was a history of two consecutive spontaneous abortions of male fetuses at around 4-5 months of pregnancy before this child. Large lobular soft masses bulged out over the affected area. The urinary bladder was protruded out (exostrophy), symphysis pubis widely separated, and the intestinal coils were visible through the thin abdominal wall [Figure - 3]. Numerous atrophic depigmented plaques were present bilaterally over the trunk, limbs, and face distributed along the Blaschko′s lines. Multiple grouped yellowish soft nodules were present below the right knee, and papillomatous lesions were noted on the chin. In addition, polydactyly and syndactyly in the right foot were observed. The fourth finger of the right hand, and the distal phalanx in a few other fingers and toes were found to be absent. Histopathologic examination of a skin biopsy from the back of the trunk showed a thinned out epidermis and dermis, with subcutaneous fat reaching up to the upper dermis. The abdominal wall defect was repaired surgically on an urgent basis in both cases. The post-operative period was uneventful and both children showed satisfactory development during the next one year of follow-up.
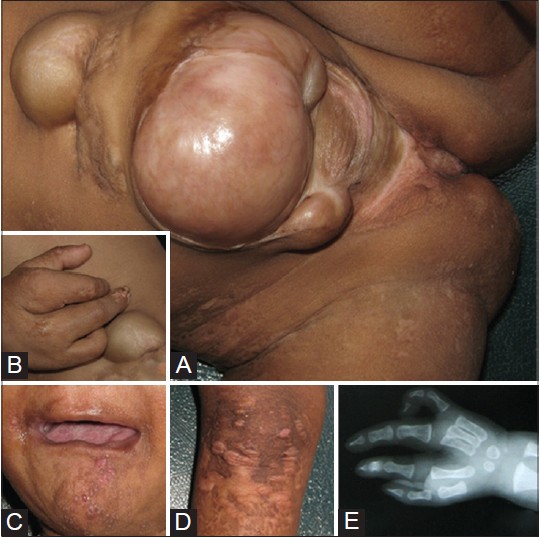 |
| Figure 3: Images of the second patient showing: (A) gross defect of lower abdominal wall with bulged out intra-abdominal organs and urinary bladder (exostrophy); (B) deformity of the hand; (C) soft papillomatous growth on chin; (D) atrophic plaques on upper leg; (E) Absent digit in right hand |
Focal dermal hypoplasia is characterized by multisystem abnormalities involving skin, bone, nails, hair, limbs, teeth, eyes, and gastrointestinal, cardiovascular, and central nervous systems. Skeletal defects are common (80% of the cases) and manifest as syndactyly, polydactyly, lobster deformity of hands and feet, and absence of part of long bones. The facial appearance is often very characteristic. This includes asymmetry, pointed chin, maxillary hypoplasia, broad nasal tip and narrow bridge, cleft lip, cleft palate, and protruding and thin ears. Mucosal leukokeratosis and gum hyperplasia may also appear. Chorioretinal coloboma, microphthalmia, microcornea, corneal clouding, keratoconus, strabismus, mental retardation, various structural defects of the central nervous system, intestinal tract, kidney, heart, and diaphragmatic, epigastric, or hiatus hernia are also noted. Severity of the condition may vary widely. Hemizygous involvement in focal dermal hypoplasia both in males and females is incompatible with life, leading to intrauterine fetal death. Females are commonly affected with this condition as they harbor lyonization or functional mosaicism. Rarely, males having somatic mosaicism are seen (approximately 10% of all cases). Thus, male cases are always sporadic.
The distinctive presentation usually assists in making a straightforward clinical diagnosis even in the absence of mutation analysis (which is often not available everywhere). It should be differentiated from other clinically similar conditions such as microphthalmia with linear skin defect (MLS), [3] angioma serpiginosum, pentalogy of Cantrell, [4] Van-Allen Myhre syndrome, nevus lipomatosus cutaneous superficialis (Hoffmann-Zurhelle), anetoderma, and pigmentary mosaicism of Ito type. Atrophic plaques may be erythematous, hypopigmented, depigmented, or hyperpigmented. Large plaques may appear "cribriform" or show protrusion of soft lipomatous masses, as seen in our cases. Protruding lipomatous masses develop due to dermal fat dysplasia and not subcutaneous fat herniation.
Umbilical, epigastric, inguinal hernias and omphalocele are known to occur in cases with gross atrophy. [5] However, extremely severe defects of the abdominal wall leading to a large area of dehiscence as seen in these two unrelated cases is considered exceedingly rare.
| 1. |
Grzeschik KH, Bornholdt D, Oeffner F, König A, del Carmen Boente M, Enders H, et al. Deficiency of PORCN, a regulator of Wnt signaling, is associated with focal dermal hypoplasia. Nat Genet 2007;39:833-5.
[Google Scholar]
|
| 2. |
Bornholdt D, Oeffner F, Konig A, Happle R, Alanay Y, Ascherman J, et al. PORCN mutations in focal dermal hypoplasia: Coping with lethality. Hum Mutat 2009;29:E618-28.
[Google Scholar]
|
| 3. |
Happle R, Daniels O, Koopman RJ. MIDAS syndrome (microphthalmia, dermal aplasia, and sclerocornea): An X-linked phenotype distinct from Goltz syndrome. Am J Med Genet 1993;47:710-3.
[Google Scholar]
|
| 4. |
Smigiel R, Jakubiak A, Lombardi MP, Jaworski W, Slezak R, Patkowski D, et al. Co-occurrence of severe Goltz-Gorlin syndrome and pentalogy of Cantrell-Case report and review of the literature. Am J Med Genet A 2011;155A: 1102-5.
[Google Scholar]
|
| 5. |
Patel JS, Maher ER, Charles AK. Focal dermal hypoplasia (Goltz syndrome) presenting as a severe fetal malformation syndrome. Clin Dysmorphol 1997;6:267-72.
[Google Scholar]
|
Fulltext Views
2,337
PDF downloads
1,640





