Translate this page into:
Squamous cell carcinoma mimicking lupus vulgaris
2 Department of Pathology, J. L. N. Medical College and Associated Group of Hospitals, Ajmer, Rajasthan, India
Correspondence Address:
Surendra Kumar
Quarter Number - AC III/3, J. L. N. Hospital Campus, Near Savitri Girls College, Ajmer - 305 001
India
| How to cite this article: Kumar S, Gondane S, Kasliwal N. Squamous cell carcinoma mimicking lupus vulgaris. Indian J Dermatol Venereol Leprol 2015;81:206-208 |
Sir,
Cutaneous squamous cell carcinoma (SCC) is a malignant tumor arising from keratinocytes of the epidermis and is predominantly a disease of white people, but is the most common type of skin cancer in non-white populations as well. [1] Generally it runs a chronic progressive course and ultimately has a tendency to metastasize; however, in our patient the lesion was regressing at one end and progressing at another end, like lupus vulgaris. We were unable to find any previously published reports of squamous cell carcinoma resembling lupus vulgaris.
A 65-year-old farmer presented to the dermatology out-patient department of our hospital with a slowly enlarging, painless erythematous ulcerated non-scaly nodulo-ulcerative plaque over the dorsal aspect of the left forearm for 5 years. The tumour was reported to bleed even on minor manipulation and trauma. The lesion started from the middle of the dorsal aspect of the forearm as an erythematous papule and gradually increased in size upwards and laterally. In due course, the lesion involved lateral and ventral the aspect of the forearm to form a noduloulcerative plaque, measuring approximately 20 × 1 cm to 2 × 0.8 cm to 1 cm. The proximal progressive end of the lesion was a shiny smooth, erythematous infiltrated non-scaly plaque and the trailing edge was ulcerated and at some places looked black, resembling necrotic tissue [Figure - 1]a and b. As the lesion increased peripherally, it started regressing from the central part which was lustureless, showing atrophic scarring, and loss of hair as compared to normal skin [Figure - 1]c. On diascopy, no resemblance to apple jelly nodules was seen. The lesion was firm at the progressive end, but was soft, friable, and bleeding on touch at the regressing end. There was no significant enlargement of axillary or other lymph nodes.
 |
| Figure 1: Erythematous non-scaly nodulo-ulcerative plaque over the dorsal aspect of the left forearm (a), both ventral and dorsal ends of the lesion (b), centre of the lesion showing skin atrophy and loss of hairs (c). Arrow in 1B denotes where the lesion began |
There was no history suggestive of tuberculosis, anywhere in the body. The patient was a chronic heavy smoker, non-alcoholic, and did not have any significant past history of tuberculosis and other chronic diseases. No one else in the family had a similar illness. The patient denied any history of anti-tubercular treatment and exposure to halogen containing drug or substances in the past.
His routine blood tests were normal, the exception being a hemoglobin of 9.8 g%. Serological tests for human immunodeficiency virus and syphilis and the Mantoux test were negative. Fine needle aspiration cytology from the left axillary lymph node did not show any evidence of metastasis. Biopsy of the axillary lymph node was not performed. An incisional skin biopsy from the lesion showed tumor cells arising from stratified sqaumous epithelium with large hyperchromatic nuclei, prominent nucleoli, granular chromatin and deep eosinophilic cytoplasm forming keratin pearls. At places, blunt broad papillae were also present along with increased mitoses. Focal areas of micro-invasion were also seen.The hair follicles and skin adnexa were normal suggestive of a well differentiated squamous cell carcinoma [Figure - 2] and [Figure - 3]. Ziehl-Neelsen staining of the skin biopsy specimen showed absence of acid fast bacilli. The atrophic area of scar tissue showed only collagen deposition and there was no evidence of lupus vulgaris or of any carcinomatous change. Periodic Acid-Schiff staining from the skin biopsy specimen revealed no fungal filaments. A final diagnosis of primary well differentiated squamous cell carcinoma was made. The patient was referred to the surgery department and the lesion was excised with a wide margin. Multiple sections of the entire excised tissue were subjected to histopathological examination and showed findings similar to the incisional skin biopsy. The patient is asymptomatic till date on follow-up.
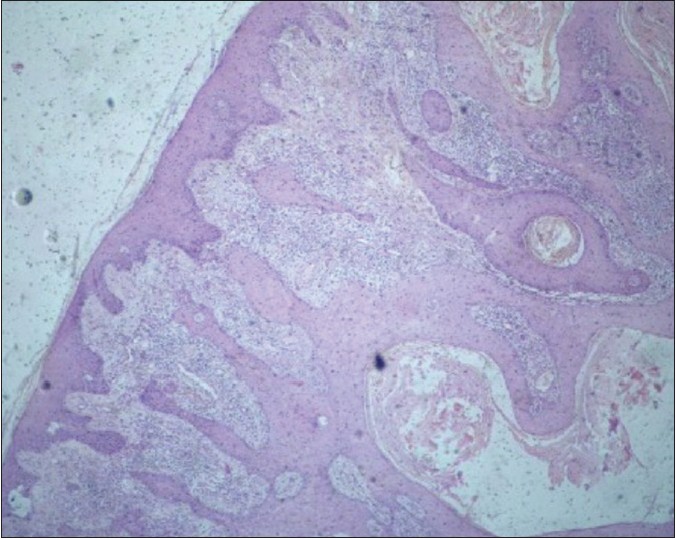 |
| Figure 2: The tumor arises from the epidermis. (H and E, x4) |
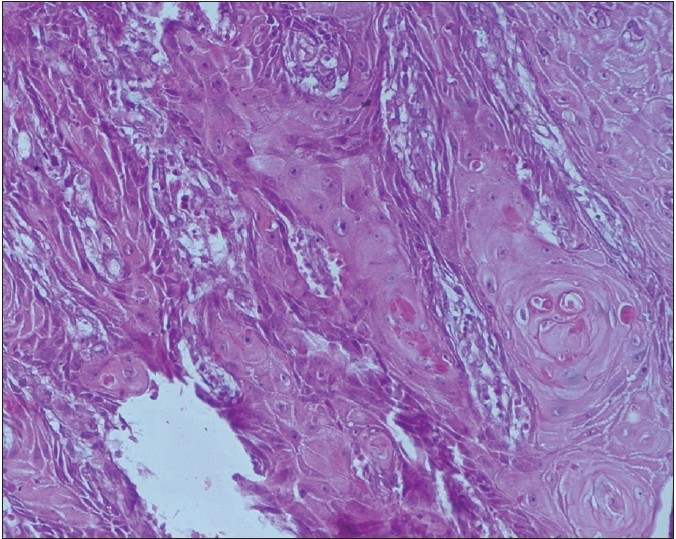 |
| Figure 3: Keratinocytes show large hyperchromatic nuclei, prominent nucleoli, granular chromatin, and deep eosinophilic cytoplasm forming keratin pearls (H and E, x20) |
Resolution at one end of the lesion and progression at another end is a feature that has been described in lesions of lupus vulgaris, the most common type of cutaneous tuberculosis. Lupus vulgaris is a chronic, progressive, post-primary, paucibacillary form of cutaneous tuberculosis, occurring in a person with a moderate or high degree of immunity. The characteristic lesion is a plaque composed of soft, reddish-brown papules which on diascopy show an appearance resembling apple jelly. The edges of the lesion gradually extend in some areas and heal with scarring in others. [2] The incidence of squamous cell carcinoma varies between 0.5% and 10.5% of lupus vulgaris cases. This occurs mostly in patients in their fourth and fifth decades. Usually it takes about 25-30 years to develop a carcinoma within a plaque of lupus vulgaris. [3] However, in our case, there was absence of any primary focus of tuberculosis. In addition, the non-scaly nature of the lesion, the negative Mantoux test, and the absence of typical features on histopathology did not favour the possibility of a primary lupus vulgaris. In addition, the duration of the lesion, of approximately 5 years, is significantly shorter than has been previously reported for lupus vulgaris to show malignant changes. These features suggest that this was not a case of lupus vulgaris with malignant transformation but one of squamous cell carcinoma mimicking lupus vulgaris, a rare presentation that dermatologists should be aware of.
| 1. |
Quinn AG, Perkins W. Non-Melanoma skin cancer and other epidermal skin tumours. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's textbook of dermatology. 8 th ed. Oxford: Blackwell; 2010. p. 52.1-48.
th ed. Oxford: Blackwell; 2010. p. 52.1-48.'>[Google Scholar]
|
| 2. |
Yates VM. Mycobacterial Infections. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's textbook of dermatology. 8 th ed. Oxford: Blackwell; 2010. p. 31.1-41.
th ed. Oxford: Blackwell; 2010. p. 31.1-41.'>[Google Scholar]
|
| 3. |
Zawirska A, Adamski Z, Stawicka E, Schwartz RA. Cutaneous squamous cell carcinoma developing in lupus vulgaris exfoliativus persistent for 40 years. Int J Dermatol 2009;48:125-7.
[Google Scholar]
|
Fulltext Views
2,463
PDF downloads
2,051





