Translate this page into:
Cutaneous annular lesions as the first sign of transformation of follicular lymphoma into diffuse large B-cell lymphoma
2 Department of Dermatology, Salamanca University Hospital, Salamanca, Spain
3 Department of Haematology, Salamanca University Hospital, Salamanca, Spain
4 Department of Pathology, Salamanca University Hospital, Salamanca, Spain
Correspondence Address:
Irene Palacios-�lvarez
Department of Dermatology, San Pedro Hospital, Calle Piqueras 98, 26006 Logroño
Spain
| How to cite this article: Palacios-�lvarez I, Rom�n-Curto C, Garc�a-Sancho AM, Santos-Briz �, Santos-Dur�n JC, Fern�ndez-L�pez E. Cutaneous annular lesions as the first sign of transformation of follicular lymphoma into diffuse large B-cell lymphoma. Indian J Dermatol Venereol Leprol 2015;81:495-497 |
Abstract
Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of non-Hodgkin lymphoma with diverse clinical, pathological and genetic features. An 80-year-old woman was diagnosed with a stage IV-X-A (Ann Arbor staging system) low grade systemic follicular lymphoma (FL). Four months after the diagnosis, she developed asymptomatic, indurated, annular erythematous plaques with centrifugal growth on the abdomen, arms and neck. The skin biopsy revealed a dermal infiltration compatible with diffuse large B-cell lymphoma. Light chain restriction by flow cytometry was demonstrated. The variable, diverse and joining genes of immunoglobulin G heavy chains were sequenced and cloned, and showed the same pattern for both the initial follicular lymphoma and the skin infiltration. Translocation t (14;18) was present in both samples. Based on these findings, a diagnosis of transformation of follicular lymphoma into diffuse large B cell lymphoma was made. Although other hematological disorders such as primary cutaneous diffuse large B cell lymphoma, mycosis fungoides and the cutaneous infiltration of chronic juvenile myeloid leukemia can present as annular lesions, we were unable to find any previous reports of these as a manifestation of cutaneous infiltration by systemic non-Hodgkin lymphoma.INTRODUCTION
Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of non-Hodgkin lymphoma [1],[2] with diverse clinical, pathological, and genetic features. [1] Immunochemotherapy with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) is considered the gold-standard treatment in elderly patients. [3] We report the case of a female patient with systemic low-grade follicular lymphoma (FL), who developed cutaneous annular lesions as a first sign of its transformation to diffuse large B cell lymphoma.
Case Report
An 80-year-old woman was diagnosed with stage IV-X-A (Ann Arbor staging system) low grade systemic follicular lymphoma arising from an intra-parotid lymph node. Histopathology showed a lymphoproliferative infiltrate with follicular architecture mainly composed of small lymphocytes, with some histiocytes and plasma cells. Some germinal centers with poorly formed mantle zones were present and contained centrocytes and centroblasts. Immunochemistry was positive for CD20, CD10, BCL2 and BCL6, and negative for CD3 and CD5 [Figure - 1]. Extension studies showed a bulky abdominal mass and bone marrow infiltration. Translocation t (14;18) was present in the bone marrow biopsy. Despite the presence of an abdominal mass, a careful wait and watch approach was decided upon, based on the patient′s age and the absence of symptoms related to the lymphoma.
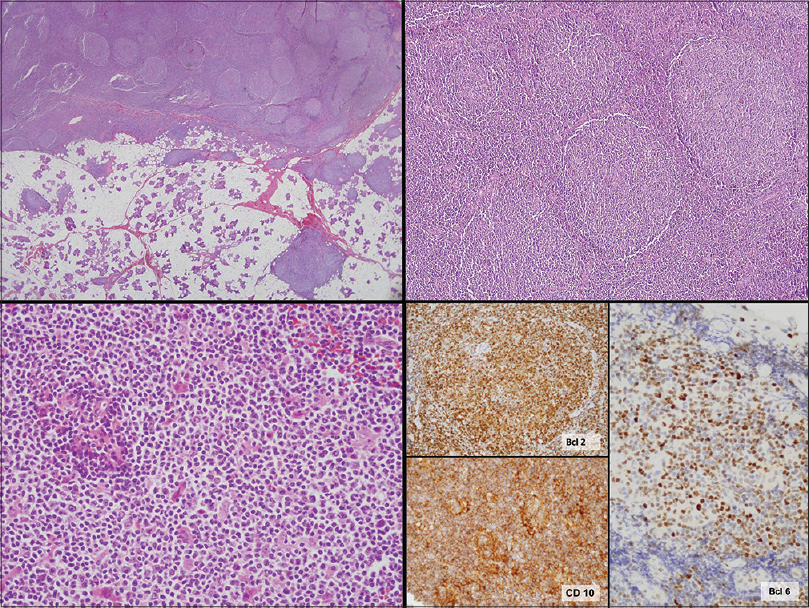 |
| Figure 1: Initial follicular lymphoma. Upper right and left: Lymphocytic infiltrate with follicular architecture (H and E, ×40, ×100). Bottom left: magnification of the infiltrate, which is composed of small lymphoctytes (H and E, ×400). Bottom right: Immunohistochemical staining positive for Bcl-2, CD10 and Bcl-6 (×400) |
Four months after diagnosis, the patient developed asymptomatic, indurated, annular erythematous patches and plaques with centrifugal growth on the abdomen, arms and neck resembling deep erythema annulare centrifugum or granuloma annulare [Figure - 2]. Progression of adenopathies and increased levels of lactate dehydrogenase (LDH) (382 U/L; normal 135-250 U/L) were also seen. The skin biopsy revealed a dermal infiltration of a B-cell lymphoproliferative disorder with epidermal sparing and a prominent subepidermal Grenz zone [Figure - 3]. The infiltrate was composed of sheets of centroblasts and immunoblasts with loss of the follicular architecture [Figure - 4]. Immunohistochemistry was positive for CD20, CD79, CD10, BCL2, and MUM-1, and negative for BCL6, TDT, CD3, CD5, CD23, CD4, CD56, CD43, and CD34. Chromogenic in situ hybridization for Epstein-Barr virus was negative [Figure - 3]. Ki-67 was over 90%. Light chain restriction by flow cytometry was demonstrated. The variable, diverse and joining genes of immunoglobulin G heavy chains were sequenced and cloned, showing the same pattern for both the initial follicular lymphoma and the skin infiltration. Moreover, translocation t (14; 18) was present in both samples.
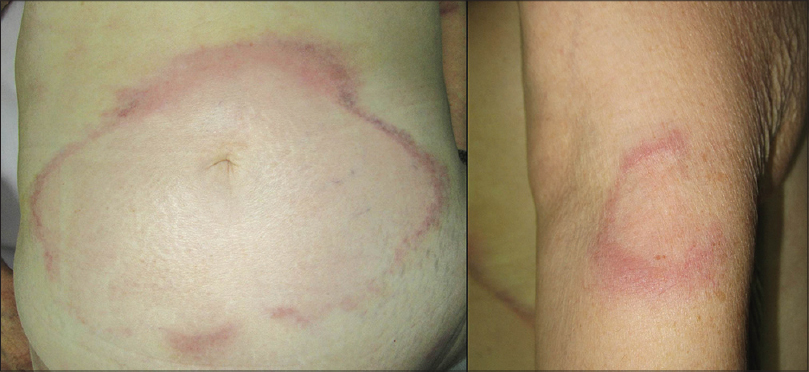 |
| Figure 2: Indurated erythematous and purplish plaques with annular shape and centrifugal growth on the abdomen and left arm corresponding to cutaneous infiltration of diffuse large B-cell lymphoma |
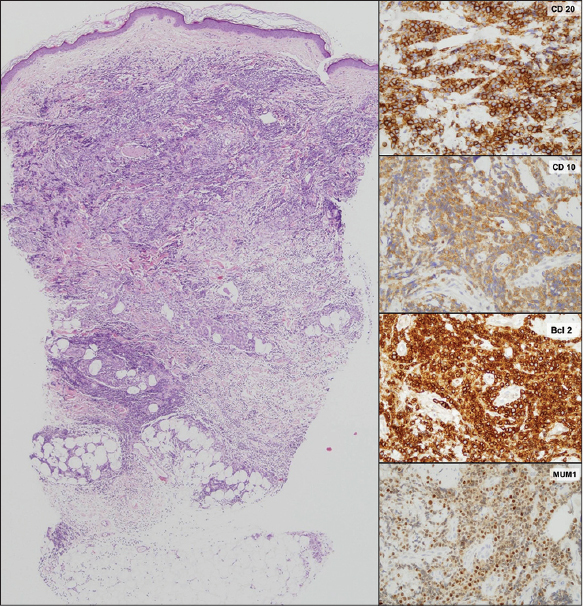 |
| Figure 3: Diffuse large B-cell lymphoma. Left: Dermal infiltration with spared epidermis and a subepidermal Grenz zone (H and E, ×40). Right: Immunohistochemical staining positive for CD20, CD-10, BCL-2, and MUM-1 (×400) |
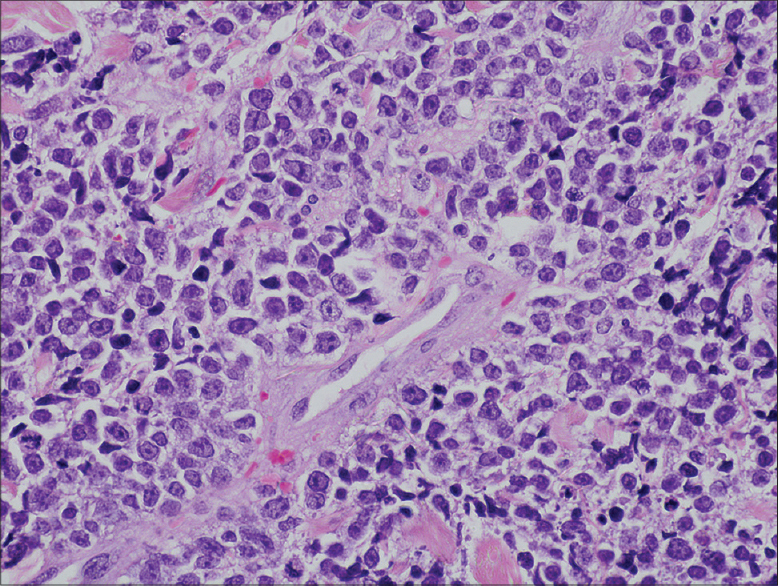 |
| Figure 4: Magnification of the infiltrate of the diffuse large B-cell lymphoma, showing centroblasts and immunoblasts (H and E, ×400) |
A diagnosis of transformation of follicular lymphoma into diffuse large B cell lymphoma was made and treatment was started with R-CHOP. After 6 cycles, complete remission of the nodal disease and a very good, but incomplete, response of the cutaneous lesions was achieved. However, 4 weeks after discontinuation of treatment, new cutaneous lesions and generalized adenopathies appeared, together with elevated LDH levels (467 U/L; normal 135-250) indicating progression of the disease which was confirmed by a fresh skin biopsy. The patient did not respond to second line chemotherapy with intravenous gemcitabine 1000/m 2 and oral dexamethasone 40 mg/m 2 and died.
DISCUSSION
Follicular lymphoma is the second most common non-Hodgkin lymphoma subtype after diffuse large B cell lymphoma. [4] Follicular lymphoma is not usually curable with conventional treatment and there is no evidence to suggest that treating asymptomatic patients improves their survival. [2] The lymphoma can transform to a more aggressive type, usually diffuse large B cell lymphoma. [5] Due to differing definition criteria, biopsy policies and length of follow-up, the reported incidence of histological transformation varies widely from 10% to more than 60% in published series. [4],[5],[6] Diagnosis of transformation should be made based on the histopathological and immunohistochemistry changes, together with the demonstration of the same immunoglobulin heavy chain rearrangement in both the pre-existing and the transformed lymphoma. [4] The most significant features in the biopsy are the development of histological characteristics of diffuse large B cell lymphoma with an increase in the proportion of large cells. [7] In our case, the main histopathological changes that supported the diagnosis of transformation were the loss of follicular architecture, a change in the lymphocytes of the infiltrate which were composed of larger cells and an increased number of immunoblasts and centroblasts in the later biopsy suggesting diffuse large B cell lymphoma. Moreover, molecular techniques confirmed that both the initial follicular lymphoma and the skin infiltration by diffuse large B cell lymphoma were clonally related, as the same traslocation t (14;18) and the same heavy chain rearrangement were present in both biopsies.
In our patient, annular plaques on the skin were the first sign of transformation. Annular lesions are usually seen in other dermatoses. Erythema annulare centrifugum, an inflammatory dermatosis, usually presents similarly and may be associated with lymphomas as a paraneoplastic syndrome. [8] Granuloma annulare also presents as annular skin-colored to erythematous papules and plaques. Its etiology is unknown and its association with systemic diseases has not been proven. [9] Lymphoproliferative disorders such as primary cutaneous diffuse large B cell lymphoma [10] and mycosis fungoides, [11] as well as the cutaneous infiltration of chronic juvenile myeloid leukemia [12] have also been described with annular lesions. However, we were unable to find any previous reports of annular lesions secondary to cutaneous infiltration by a systemic non-Hodgkin lymphoma.
| 1. |
Menon MP, Pittaluga S, Jaffe ES. The histological and biological spectrum of diffuse large B-cell lymphoma in the World Health Organization classification. Cancer J 2012;18:411-20.
[Google Scholar]
|
| 2. |
Shankland KR, Armitage JO, Hancock BW. Non-Hodgkin lymphoma. Lancet 2012;380:848-57.
[Google Scholar]
|
| 3. |
Fields PA, Linch DC. Treatment of the elderly patient with diffuse large B cell lymphoma. Br J Haematol 2012;157:159-70.
[Google Scholar]
|
| 4. |
Conconi A, Ponzio C, Lobetti-Bodoni C, Motta M, Rancoita PM, Stathis A, et al. Incidence, risk factors and outcome of histological transformation in follicular lymphoma. Br J Haematol 2012;157:188-96.
[Google Scholar]
|
| 5. |
Lossos IS, Gascoyne RD. Transformation of follicular lymphoma. Best Pract Res Clin Haematol 2011;24:147-63.
[Google Scholar]
|
| 6. |
Link BK, Maurer MJ, Nowakowski GS, Ansell SM, Macon WR, Syrbu SI, et al. Rates and outcomes of follicular lymphoma transformation in the immunochemotherapy era: A report from the University of Iowa/MayoClinic Specialized Program of Research Excellence Molecular Epidemiology Resource. J Clin Oncol 2013;31:3272-8.
[Google Scholar]
|
| 7. |
de Jong D, de Boer JP. Predicting transformation in follicular lymphoma. Leuk Lymphoma 2009;50:1406-11.
[Google Scholar]
|
| 8. |
Carlesimo M, Fidanza L, Mari E, Pranteda G, Cacchi C, Veggia B, et al. Erythema annulare centrifugum associated with mantle b-cell non-Hodgkin′s lymphoma. Acta Derm Venereol 2009;89:319-20.
[Google Scholar]
|
| 9. |
Thornsberry LA, English JC 3 rd . Etiology, diagnosis, and therapeutic management of granuloma annulare: An update. Am J Clin Dermatol 2013;14:279-90.
[Google Scholar]
|
| 10. |
Belousova IE, Vanecek T, Skreg SV, Rodionov AN, Samtsov AV, Kazakov DV. Unusual clinicopathological presentation of primary cutaneous diffuse large B-cell lymphoma, leg type, with multiple nodules and widespread garland-like lesions. Am J Dermatopathol 2009;31:370-4.
[Google Scholar]
|
| 11. |
Lim DS, Murphy GM, Egan CA. Mycosis fungoides presenting as annular erythema. Br J Dermatol 2003;148:591.
[Google Scholar]
|
| 12. |
Anzai H, Kikuchi A, Kinoshita A, Nishikawa T. Recurrent annular erythema in juvenile chronic myelogenous leukaemia. Br J Dermatol 1998;138:1058-60.
[Google Scholar]
|
Fulltext Views
4,235
PDF downloads
1,494





