Translate this page into:
Extrafacial rosacea with predominant scalp involvement
2 Department of Pathology, Hospital Ramon y Cajal, E-28034 Madrid, Spain
Correspondence Address:
Laura Miguel-Gomez
Department of Dermatology, Hospital Ramon y Cajal, E-28034 Madrid
Spain
| How to cite this article: Miguel-Gomez L, Fonda-Pascual P, Vano-Galvan S, Carrillo-Gijon R, Mu�oz-Zato E. Extrafacial rosacea with predominant scalp involvement. Indian J Dermatol Venereol Leprol 2015;81:511-513 |
Sir,
Extrafacial rosacea is infrequent. It usually accompanies the most serious cases of rosacea, but may also appear with only mild facial lesions. [1]
A 42-year-old male presented with a 4-day history of pruritic lesions on the scalp and cheeks. There was history of similar outbreaks in the past 3 years with worsening of lesions on sun exposure. He had not received any oral or topical treatment for the condition. There were no ocular symptoms. Examination revealed multiple tiny papules and non-follicular pustules coalescing into an erythematous plaque over the scalp and cheeks [Figure - 1]a and b. Microbiological culture of pustules were sterile. Biopsy of the scalp lesion revealed non-caseating epithelioid granulomas in the dermis, solar elastosis and Demodex folliculorum in some hair follicles [Figure - 2]. Based on the clinical and histological features, a diagnosis of extrafacial rosacea with predominant scalp involvement was made. Oral doxycycline, 100 mg daily and topical metronidazole were administered for 20 days with marked improvement, leading to remission in 6 weeks [Figure - 3]a and b. In addition, rosacea improved with daily use of sunscreen. The patient was followed up for 6 months without relapse. He has sometimes needed to use topical metronidazole since.
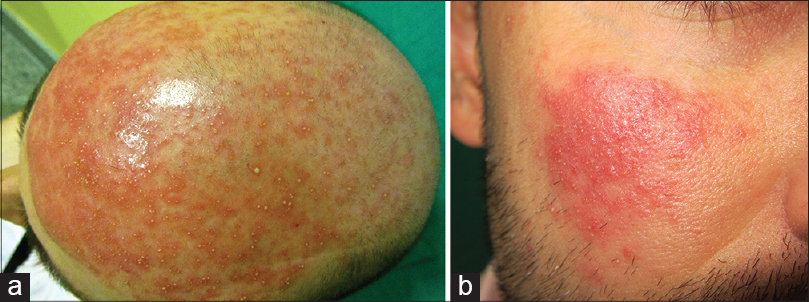 |
| Figure 1: Small papules and nonfollicular pustules coalescing into an erythematous plaque distributed over (a) the scalp and (b) both cheeks |
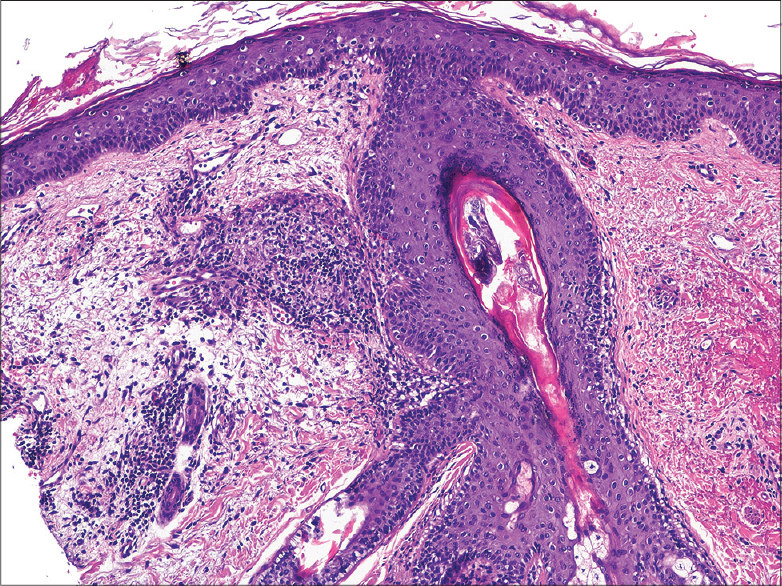 |
| Figure 2: Non-caseating epithelioid granuloma in the dermis, solar elastosis and mite in hair follicle (H and E, ×200) |
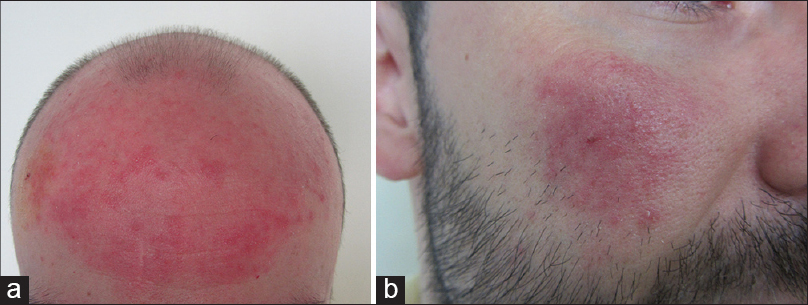 |
| Figure 3: Regression in lesions (a) on scalp and (b) face after after 20 days of oral doxycycline and topical metronidazole |
Rosacea is a common, chronic inflammatory entity with a wide range of clinical features such as telangiectasias, papules, pustules and erythema primarily affecting the "T-zone" (forehead and nose) and cheeks. It is more frequent in pale-skinned people, affecting up to 5% of the North American Caucasian population even though any ethnicity may be affected. Pathogenesis remains uncertain. Several factors have been implicated such as disorders of vascular reactivity, genetic predisposition, weather conditions and immune response against microorganisms such as Demodex folliculorum and Helicobacter pylori. There are four different well described definite subtypes of rosacea: (i) erythematotelangiectatic (vascular) rosacea with a recurrent blush becoming long-lasting and finally permanent; (ii) papulopustular (inflammatory) rosacea with small papules and pustules and even nodules resembling acne as was seen in our patient; (iii) phymatous rosacea with overgrowth and hyperplasia of sebaceous glands in certain facial areas causing disfigurement (rhinophyma, gnatophyma, etc.); and (iv) ocular rosacea with blepharitis or conjunctivitis. Furthermore, two rare variants of rosacea have been reported: (a) granulomatous variant, which can manifest with erythematous and monomorphic papules or nodules with periorificial location; and (b) rosacea fulminans, characterized by the sudden eruption of cystic nodules, papules and pustules over the chin, cheeks and forehead. Rosacea most commonly affects young women. [2] The etiopathogenesis of extrafacial rosacea is unknown but it is believed that solar elastosis in chronically sun-exposed skin and disseminated infestation by D. folliculorum play an important role. [3] Extrafacial rosacea predominantly affects men and is a diagnostic challenge due to its atypical clinical pattern. [4] The granulomatous variant is more common in extrafacial lesions and up to 15% of patients with granulomatous rosacea have extrafacial involvement. Characteristically, scalp involvement is predominantly pustular, as in our case. [4]
Histopathological findings of rosacea are not usually diagnostic since they vary depending on the disease stage. In the early stage, there is edema and vascular ectasia. As the disease advances, a perivascular and perifollicular lympho-histiocytic infiltrate may appear along with non-caseating epithelioid granulomas surrounded by lymphocytes. Finally, there is development of sebaceous hyperplasia with elastosis. Lack of comedo formation helps to differentiate this condition from acné. [2]
Rosacea is a challenging disease to diagnose, and many other entities have to be considered in the differential diagnosis. Seborrheic dermatitis predominantly involves the eyebrows, periauricular, paranasal and, glabellar region. Keratosis pilaris rubra presents with marked erythema and keratotic follicular papules affecting the cheeks and the proximal arms. Lupus erythematous is characterized by the presence of erythema over the cheeks and nasal bridge (malar rash). Haber syndrome, which is a rare genodermatosis, is characterized by rosacea-like facial eruption with telangiectasias and multiple truncal keratotic lesions. Acne vulgaris is a common skin condition and is characterized by comedones, papules, and pustules in teenagers and young adults.
In rosacea, basic skin care such as daily use of sunscreen offers significant benefits. Topical therapies like metronidazole or azelaic acid, along with oral tetracyclines (doxycycline or minocycline 100 mg once daily for 3 weeks with gradual tapering to the least effective dose over several weeks or months) are the most appropriate management strategy for treating rosacea because they can reduce inflammatory lesion counts by their anti-inflammatory action. [5] Low dose isotretinoin (0.1-0.2 mg/kg/day) is given in severe rosacea and in some cases of extrafacial rosacea, and is found to be effective and safe. [1],[4] Other oral antibiotics such as azithromycin or erythromycin have achieved good results. Laser and surgery are used in selected cases. [2]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Pereira TM, Vieira AP, Basto AS. Rosacea with extensive extrafacial lesions. Int J Dermatol 2008;47:52-5.
[Google Scholar]
|
| 2. |
Barco D, Alomar A. Rosacea. Actas Dermosifiliogr 2008;99:244-56.
[Google Scholar]
|
| 3. |
Wong CS, Kirby B. Demodicidosis in scalp rosacea? Clin Exp Dermatol 2004;29:318-9.
[Google Scholar]
|
| 4. |
Bostanci O, Borelli C, Schaller M. Treatment of extrafacial rosacea with low-dose isotretinoin. Acta Derm Venereol 2010;90:409-10.
[Google Scholar]
|
| 5. |
Smith LA, Meehan SA, Cohen DE. Rosacea fulminans with extrafacial lesions in an elderly man: Successful treatment with subantimicrobial-dose doxycycline. J Drugs Dermatol 2014;13:763-5.
[Google Scholar]
|
Fulltext Views
6,981
PDF downloads
2,583





