Translate this page into:
Peripheral T-cell lymphoma, not otherwise specified with prominent cutaneous involvement
2 Department of Emergency Medicine, Henry Ford Hospital, Detroit, MI, 48202, USA
Correspondence Address:
Ben Jacob Friedman
Department of Dermatology, 3031 West Grand Blvd., 8th Floor, Detroit, MI 48202
USA
| How to cite this article: Friedman BJ, McHargue CA, Nauss MD. Peripheral T-cell lymphoma, not otherwise specified with prominent cutaneous involvement. Indian J Dermatol Venereol Leprol 2015;81:535-537 |
Sir,
A 39-year-old African American man presented to our emergency department with an approximately 1-year history of painful, enlarging skin nodules. The first lesion reportedly appeared on the thigh, with the most recent ones developing on the face and scalp. He also complained of subjective fevers and night sweats. Examination revealed multiple, variably-sized, indurated skin nodules, with central ulceration and yellow-brown crusting distributed on the scalp, face, umbilicus, buttocks, bilateral thighs and right arm [Figure - 1]. In addition, there was prominent edema of the head and neck with palpable matted lymphadenopathy in both the axillae and groin.
 |
| Figure 1: Multiple ulcerated large nodules involving the scalp, forehead, and right side of the face with associated edema |
Multiple skin biopsies and an excisional lymph node biopsy from the right axillae were obtained. Histopathological analysis of the skin revealed a nodular lympho-histiocytic infiltrate filling the dermis, which consisted of many large and atypical lymphocytes [Figure - 2] and [Figure - 3]. No significant epidermotropism was identified though there were some focal areas of peri-follicular necrosis. A T-cell gene rearrangement study revealed a monoclonal population of cells which, on further immunotyping, was consistent with a mature CD4+ T-cell lymphoma [Figure - 4]. Similar analysis together with flow cytometry of the sampled lymph node revealed identical morphologic and immunophenotypic features of lymphoma as detected in the skin. A staging positron emission tomography-computed tomography scan revealed intense fluorodeoxyglucose uptake in the lymph nodes of neck, parotid glands, axillae, inguinal and iliac chains, as well as spleen. Bone marrow biopsy, flow cytometry of the blood and bone marrow and human T-cell lymphotropic virus-1/2 serologies were negative. In view of these findings, a diagnosis of peripheral T-cell lymphoma, not otherwise specified (PTCL- NOS) was rendered with a stage of IIIES.
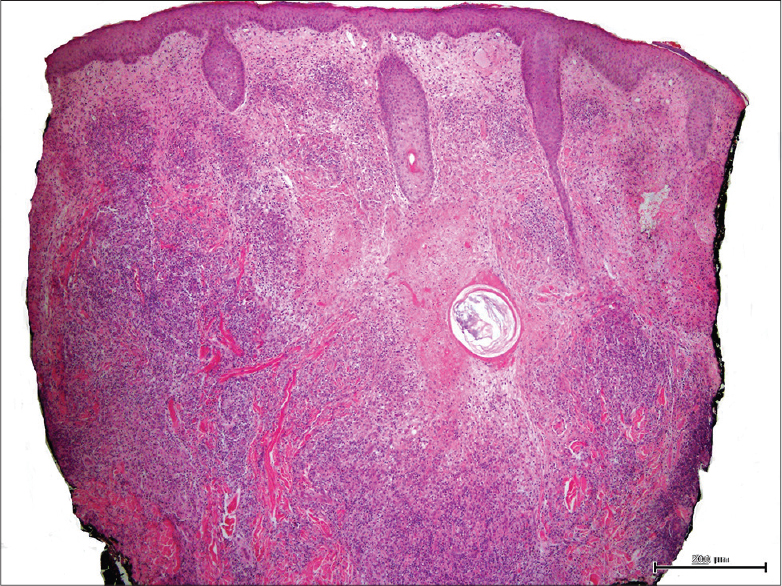 |
| Figure 2: Nodular lymphohistiocytic infiltrate filling the dermis, with some peri-follicular necrosis (H and E, ×50) |
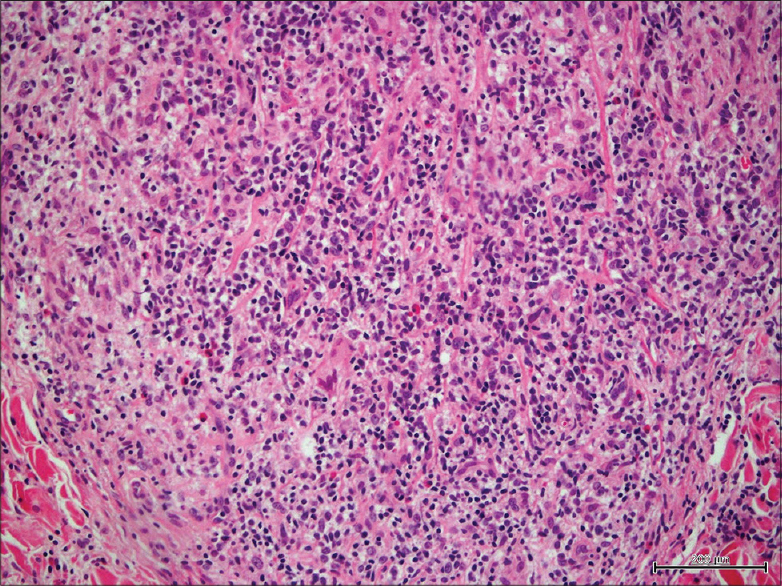 |
| Figure 3: Numerous large lymphocytes with irregular rims, admixed with epithelioid histiocytes and scattered eosinophils (H and E, ×400) |
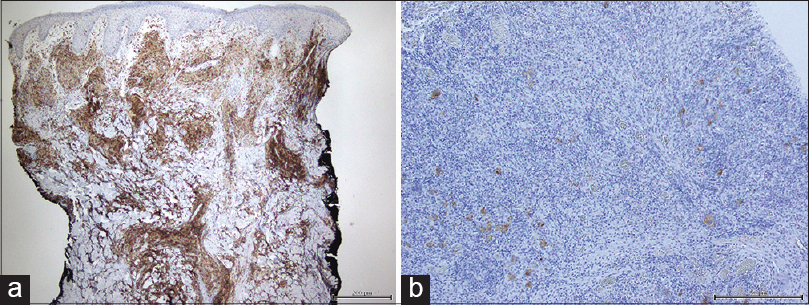 |
| Figure 4: (a) CD4 stain demonstrating expression in the majority of the atypical cells (×50). (b) CD30 stain demonstrating only focal expression in a minority of cells (×100) |
Lymphomas presenting in the skin are most commonly of T-cell origin, typically falling under the category of primary cutaneous T-cell lymphoma. Mycosis fungoides and Sézary syndrome comprise the majority of these cases. When skin nodules develop de novo, without preceding or co-existent patches, plaques or erythroderma more typical of mycosis fungoides, other less common entities should be considered. These may include other primary cutaneous T-cell lymphomas as well as systemic T-cell lymphomas with secondary cutaneous metastasis. In our patient, the prominent ulceration and coexistent widespread nodal and splenic involvement was suggestive of an aggressive peripheral T-cell lymphoma. Furthermore, the immunophenotypical characteristics in this case were not consistent with a CD30+ lymphoproliferative disorder, CD8+ aggressive epidermotropic T-cell lymphoma or primary cutaneous γδ T-cell lymphoma. [1]
Peripheral T-cell lymphoma-not otherwise specified (PTCL-NOS), is a poorly defined and heterogeneous group of predominantly nodal T-cell lymphomas not meeting histopathological or immunophenotypical criteria for the other well-defined subtypes of peripheral T-cell lymphoma. [2] The disease is rare in relation to other subtypes of cutaneous T-cell lymphoma, with only 82 (9%) patients being classified as PTCL-NOS in one large cutaneous T-cell lymphoma registry. [3] In the limited reports to date, patients with PTCL-NOS tend to present with generalized lymphadenopathy with or without the extranodal disease. [3],[4] The skin and gastrointestinal tract represent the most commonly involved extranodal sites, with the cutaneous disease typically presenting as disseminated nodules. [3],[4] In one description of 82 cases of cutaneous PTCL-NOS, 17 (20.7%) patients were observed to have concurrent nodal involvement at the time of presentation. [3]
Initial treatment may include cyclophosphamide, hydroxydaunorubicin, oncovin and prednisone -based chemotherapy, radiation therapy and/or autologous hematopoietic cell transplantation. [5] The prognosis is considered poor, with previously reported 5-year survival rates of under 20%. [3] Negative prognostic indicators include multifocal skin involvement, concurrent extracutaneous disease, lack of spontaneous improvement, age older than 70 years and large cell morphology (of which, the first three were seen in our patient). [3]
Prior to completion of the workup, our patient was placed on a prolonged course of narcotic analgesics, oral steroids and antibiotics to treat his pain, swelling and methicillin-resistant Staphylococcus aureus superinfection respectively. He then received radiation to reduce the size of the larger and most symptomatic tumors. He has completed 4 out of 6 planned cycles of cyclophosphamide, hydroxydaunorubicin, oncovin and prednisone plus etoposide. The follow-up positron emission tomography-computed tomography revealed interval resolution of all the previously identified foci of lymphoma. His pain and constitutional symptoms have subsided, and the skin nodules have resolved with atrophic hypopigmented scars.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Kempf W, Rozati S, Kerl K, French LE, Dummer R. Cutaneous peripheral T-cell lymphomas, unspecified/NOS and rare subtypes: A heterogeneous group of challenging cutaneous lymphomas. G Ital Dermatol Venereol 2012;147:553-62.
[Google Scholar]
|
| 2. |
Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. Lyon, France: IARC Press; 2008.
[Google Scholar]
|
| 3. |
Bekkenk MW, Vermeer MH, Jansen PM, van Marion AM, Canninga-van Dijk MR, Kluin PM, et al. Peripheral T-cell lymphomas unspecified presenting in the skin: Analysis of prognostic factors in a group of 82 patients. Blood 2003;102:2213-9.
[Google Scholar]
|
| 4. |
Weisenburger DD, Savage KJ, Harris NL, Gascoyne RD, Jaffe ES, MacLennan KA, et al. Peripheral T-cell lymphoma, not otherwise specified: A report of 340 cases from the International Peripheral T-cell Lymphoma Project. Blood 2011;117:3402-8.
[Google Scholar]
|
| 5. |
Schmitz N, Trümper L, Ziepert M, Nickelsen M, Ho AD, Metzner B, et al. Treatment and prognosis of mature T-cell and NK-cell lymphoma: An analysis of patients with T-cell lymphoma treated in studies of the German High-Grade Non-Hodgkin Lymphoma Study Group. Blood 2010;116:3418-25.
[Google Scholar]
|
Fulltext Views
3,375
PDF downloads
1,362





