Translate this page into:
Sporotrichoid cutaneous tuberculosis
Correspondence Address:
T S Nagesh
No 1586, 'Niharika', 17th 'A' main, 1st stage, 5th block, HBR layout, Bangalore - 560 043, Karnataka
India
| How to cite this article: Nagesh T S, Akhilesh A. Sporotrichoid cutaneous tuberculosis. Indian J Dermatol Venereol Leprol 2014;80:279 |
Sir,
Sporotrichoid skin infections refer to conditions that simulate the subcutaneous linear lymphangitic form of sporotrichosis. [1] Various infections have been reported to cause such a distribution, among which atypical mycobacterial infections are more commonly implicated. [2] So far only a few sporadic cases of sporotrichoid cutaneous tuberculosis have been reported. [3]
A 27-year-old male presented with an asymptomatic verrucous growth over the dorsum of the right great toe since one and a half years. He also had history of a lesion over the thigh which had developed three months after the initial lesion. There was a history of thorn prick injury before the onset of these lesions. He had presented to us with the same complaints nine months back; however, he did not take any treatment at that time.
On examination, a verrucous nodule measuring 2 × 2 cm was present over the dorsum of the right great toe extending up to the base of the toe [Figure - 1]. A hyperpigmented plaque measuring 5 × 5 cm was present over the medial side of the right thigh [Figure - 2]. Skin over the plaque showed atrophy and cribriform scarring at one end and elevated borders at the other. A few healed hyperpigmented macules/patches were also seen over the medial side of the right leg. All these lesions were distributed in a linear pattern [Figure - 3]. There was no regional lymphadenopathy. Systemic examination was unremarkable. The hemogram was normal though the erythrocyte sedimentation rate (ESR) was elevated. Mantoux test was negative. Chest X-ray and other biochemical parameters were within normal limits.
 |
| Figure 1: Warty paroncyhial growth over the dorsum of great toe |
 |
| Figure 2: Plaque over the right thigh with scarring |
 |
| Figure 3: Linear distribution of lesions |
Skin biopsy taken from both the dorsum of the toe and nodular margin of the plaque showed epithelioid granulomas with Langhans giant cells and a mixed inflammatory infiltrate. [Figure - 4] The lesion over the toe showed pseudoepitheliomatous hyperplasia. Periodic acid-Schiff (PAS) stain was negative for any fungal elements and fungal culture did not yield any growth.
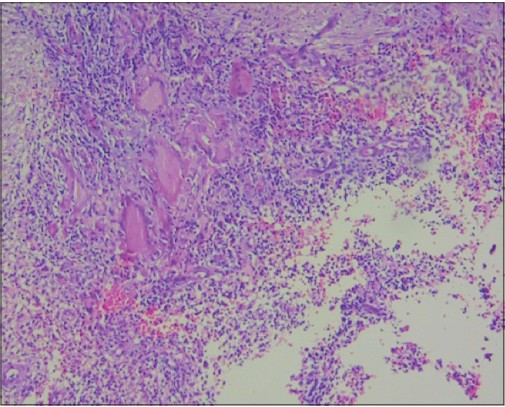 |
| Figure 4: Epitheloid granuloma with Langhans giant cell (H and E, x100) |
Based on the clinical and histopathological findings, a final diagnosis of sporotrichoid cutaneous tuberculosis was made and the patient was treated with standard antitubercular treatment of the Revised National Tuberculosis Control Programme (RNTCP) Cat I regimen. The lesions showed a significant response within two months of starting treatment [Figure - 5].
 |
| Figure 5: Resolving lesion after starting treatment |
Sporotrichoid lymphocutaneous infection is a syndrome characterized by development of superficial cutaneous lesions that progress along dermal and subcutaneous lymphatics. The term "sporotrichoid" is described after the infection caused by the dimorphic fungus Sporothrix schenckii. [2] Other cutaneous infections which occasionally can present in a sporotrichoid distribution include atypical mycobacteriosis (M. kansasii, M. marinum and M. chelonae), nocardiosis, cutaneous leishmaniasis, cutaneous tuberculosis, leprosy and deep mycoses (blastomycosis, histoplasmosis, cryptococcosis, chromoblastomycosis). [3]
Lupus vulgaris remains the most common form of cutaneous tuberculosis. [4],[5] The disease is acquired exogenously by direct inoculation of the bacilli or endogenously by hematogenous or lymphatic spread from an underlying infected focus. Various morphological patterns have been described including papular, nodular, plaque, ulcerative, vegetative and tumid lesions. Unusual forms such as framboesiform, gangrenous or ulcero-vegetative types which are more common in immunocompromised individuals have also been reported. [3] Given its worldwide prevalence and the rising incidence of HIV, it is important for clinicians to recognize the variants and promptly treat the patient.
In our case, the patient had lesions with two different morphologies. The lesion on the great toe was that of a warty paronychial type whereas the one on the thigh was a plaque with an advancing edge with residual scarring. He also had healed hyperpigmented macules over the medial side of the leg. This linear arrangement of lesions mimicked a sporotrichoid distribution. However, our diagnosis of lupus vulgaris was based mainly on the morphology of lesions, histopathological findings of tuberculoid granuloma, the absence of growth on fungal culture and the response to anti-tubercular therapy.
| 1. |
Ramesh V. Sporotrichoid cutaneous tuberculosis. Clin Exp Dermatol 2007;32:680-2.
[Google Scholar]
|
| 2. |
Tobin EH, Jih WW. Sporotrichoid lymphocutaneous infections: Etiology, diagnosis and therapy. Am Fam Physician 2001;63:326-32.
[Google Scholar]
|
| 3. |
Khandpur S, Nanda S, Reddy BS. An unusual episode of lupus vulgaris masquerading as sporotrichosis. Int J Dermatol 2001;40:336-9.
[Google Scholar]
|
| 4. |
Varshney A, Goyal T. Incidence of various clinico-morphological variants of cutaneous tuberculosis and HIV concurrence: A study from the Indian subcontinent. Ann Saudi Med 2011;31:134-9.
[Google Scholar]
|
| 5. |
Wozniacka A, Schwartz RA, Sysa-Jedrzejowska A, Borun M, Arkuszewska C. Lupus vulgaris: Report of two cases. Int J Dermatol 2005;44:299-301.
[Google Scholar]
|
Fulltext Views
2,272
PDF downloads
1,344





