Translate this page into:
Multiple morphological presentations of skin tuberculosis in a patient
Correspondence Address:
Neelakantababu Rasineni
Department of Dermatology, Venereology and Leprology, Sri Venkateswara Ramnarayan Ruia Government General Hospital, Sri Venkateswara edical College, Tirupathi - 517507, Andhra Pradesh
India
| How to cite this article: Rasineni N, Ramana P V, Kota S, Gandikota RK. Multiple morphological presentations of skin tuberculosis in a patient. Indian J Dermatol Venereol Leprol 2014;80:347-349 |
Sir,
Cutaneous tuberculosis constitutes about 1.5% of all forms of extra pulmonary tuberculosis and manifests as different types like lupus vulgaris, tuberculosis verrucosa cutis (TVC), scrofuloderma, tuberculous gumma, tuberculous chancre, miliary tuberculosis, papulonecrotic tuberculid and lichen scrofulosorum. [1] Coexistence of different types of cutaneous tuberculosis is occasionally reported. [2],[3] Multifocal presentation of cutaneous tuberculosis is also reported. [4] Tuberculous osteomyelitis and arthritis commonly involve spine and weight bearing joints, while elbow, wrist and interphalangeal joints are less commonly involved. [5] We report a case of multifocal presentation of different types of cutaneous tuberculosis along with a rare form of joint tuberculosis.
A 42-year-old married woman presented with a 4-month history of a painless swelling over the left wrist and right great toe followed by spontaneous ulceration. She had warty lesions over the left sole and left index finger that were slowly enlarging for the past two months. There was significant weight loss. Several topical and systemic medications including oral steroids had been used for two months without any improvement.
Examination showed a well-defined verrucous plaque in the center of left sole, 3 × 5 cm in size, and another on the dorsum of left index finger, 3 × 2 cm in size [Figure - 1](a) and [Figure - 2]. The base of the lesions were not fixed to deeper structures. In addition, there were two indurated ulcers over the flexor aspect of swollen left wrist and the dorsum of right great toe, 0.5 × 1 cm and 3 × 4 cm in size, respectively [Figure - 3](a) and [Figure - 4], with irregular margins, undermined edges, surrounded by hyperpigmentation and fixed to underlying structures. There was a BCG scar. Two discrete, mobile, non-tender lymph nodes of 3 × 2 cm and 3 × 4 cm were noted in the left inguinal region. Chest and abdomen were normal on examination.
 |
| Figure 1: (a) Tuberculosis verrucosa cutis over left sole (b) Tuberculosis verrucosa cutis showing remarkable clearance after 1 month of starting anti-tubercular therapy |
 |
| Figure 2: Tuberculosis verrucosa cutis over dorsum of left index finger |
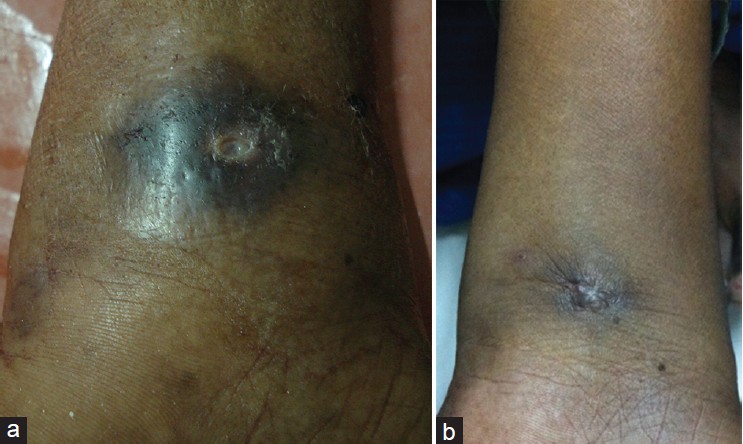 |
| Figure 3: (a) Scrofuloderma over left wrist (b) Scrofuloderma over wrist 6 months after taking anti-tubercular therapy. The ulcer has healed with a puckered scar |
 |
| Figure 4: Scrofuloderma over right great toe joint |
Complete blood picture was normal except for raised erythrocyte sedimentation rate (ESR) of 72 mm. Serology was negative for HIV. Smears taken from ulcers were negative on examination with potassium hydroxide (KOH) preparation and on staining for acid-fast bacilli (AFB). Mantoux test was negative at the initial visit. As the patient was on long-term steroid therapy earlier, we repeated the Mantoux test one month after starting treatment, and it was positive showing an induration of 20 mm. Sputum for AFB was negative. Fine needle aspiration cytology (FNAC) of left inguinal lymph nodes showed features of tuberculosis. Chest X-ray and abdomino-pelvic ultrasonography were normal. X-rays of involved parts showed decreased joint space and regional osteoporosis over the left wrist and destruction of proximal phalanx of the great toe [Figure - 5]. Biopsy from the verrucous lesion on the sole revealed prominent hyperkeratosis along with numerous lymphocytes, epithelioid cells and Langhans giant cells in the dermis consistent with tuberculosis verrucosa cutis. Punch biopsy from the edge of the ulcer on the great toe and synovial biopsy of the affected wrist showed a well-defined granuloma with Langhans giant cells and lymphocytes consistent with tuberculosis. Hence, the ulcers over wrist and great toe represented scrofuloderma that resulted after breakdown of skin overlying contiguous joint tuberculosis.
 |
| Figure 5: X-ray right foot with destruction at 1st interphalangeal joint |
Category II anti tuberculous therapy was started with rifampicin, isoniazid, pyrazinamide and ethambutol. One month later, there was remarkable clearance of tuberculosis verrucosa cutis [Figure - 1]b. After five months of treatment, there was complete clearance of the verrucous lesions leaving an atrophic scar while scrofuloderma over the left wrist healed with a puckered scar [Figure - 3]b. A repeat X-ray showed increase in density of the carpal bones.
Cutaneous tuberculosis is perceived to form a spectrum of manifestations with scrofuloderma, an endogenous and multibacillary form resulting from involvement and breakdown of skin overlyinging a contiguous tubercular focus in a person with low immunity and tuberculosis verrucosa cutis, an exogenous and paucibacillary form occurring after accidental superinfection or autoinoculation or post-traumatic inoculation with infected sputum occurring in a person with good immunity. [1]
Coexistence of these types of cutaneous tuberculosis with tuberculosis verrucosa cutis developing after scrofuloderma in nearby skin was reported previously by Sethuraman et al.,[3] . Müzeyyen et al.,[2] reported a case where tuberculosis verrucosa cutis was located distant from scrofuloderma. Tuberculosis verrucosa cutis coexisting with articular tuberculosis was reported by Marquet et al.,[6] while scrofuloderma overlying the acromio-clavicular joint was reported by Tan et al.[7]
In our patient, two lesions of tuberculosis verrucosa cutis and two lesions of scrofuloderma with underlying joint involvement were seen in different areas of the hands and feet. The co-existence of multifocal cutaneous tuberculosis of different forms with joint involvement is rare.
| 1. |
Sethi A.Tuberculosis and infections with atypical mycobacteria. In: Goldsmith LA, Katz SI, Gilcherst BA, Paller AS, Leffell DJ, Wolff K, editors. Fitzpatrick's Dermatology in General Medicine. 8 th ed. New York: McGraw-Hill; 2012. p. 1225-36.
th ed. New York: McGraw-Hill; 2012. p. 1225-36.'>[Google Scholar]
|
| 2. |
Gönül M, Gül U, Kilic A, Soylu S, Demiriz M, Kubar A. Coexistence of tuberculosis verrucosa cutis with scrofuloderma. Turk J Med Sci 2008;38:495-9.
[Google Scholar]
|
| 3. |
Sethuraman G, Kaur J, Nag HL, Khaitan BK, Sharma VK, Singh MK. Symmetrical scrofuloderma with tuberculosis verrucosa cutis. Clin Exp Dermatol 2006;31:475-7.
[Google Scholar]
|
| 4. |
Rajan J, Mathai AT, Prasad PV, Kaviarasan PK. Multifocal tuberculosis verrucosa cutis. Indian J Dermatol 2011;56:332-4.
[Google Scholar]
|
| 5. |
Martinez SF, Mihalko MJ. Tuberculosis and other unusual infections. In: Canale ST, Beaty JH, editors. Campbell's Operative Orthopaedics. 11 th ed. Philadelphia: Mosby Company; 2008. p. 753-71.
th ed. Philadelphia: Mosby Company; 2008. p. 753-71.'>[Google Scholar]
|
| 6. |
Marquet A, Moya L, Aldanondo I, Muñoz-Zato E, Carrillo R, Jaén P. Coexistence of tuberculosis verrucosa cutis and articular tuberculosis in the same patient. Actas Dermosifiliogr 2006;97:56-8.
[Google Scholar]
|
| 7. |
Tan WP, Tang MB, Tan HH. Scrofuloderma from the acromioclavicular joint presenting as a chronic ulcer in an immunocompetent host. Singapore Med J 2007;48:e243-5.
[Google Scholar]
|
Fulltext Views
3,169
PDF downloads
1,961





