Translate this page into:
Dermoscopy in tungiasis
Correspondence Address:
Karina Cataldo
Vicu�a Mackenna 4686, Santiago
Chile
| How to cite this article: Abarzua A, Cataldo K, Alvarez S. Dermoscopy in tungiasis. Indian J Dermatol Venereol Leprol 2014;80:371-373 |
Sir,
A 24-year-old Chilean male complained of a painful white papule with a brownish central area on the lateral aspect of his left foot [Figure - 1]. He noticed it immediately after returning from a 1-week trip to Paraguay. On dermoscopic examination, we observed a round lesion with a dark central pore, an incomplete radiated crown and a pigmented peripheral ring, arranged from the inner to outer aspect [Figure - 2]. Additionally, blue-black blotches and whitish oval structures linked together forming chain like structures were noted [Figure - 2]. A clinical diagnosis of tungiasis was made, and we shaved the lesion with evacuation of the eggs and fecal material [Figure - 3]. This was followed by cryotherapy and tetanus vaccination.
 |
| Figure 1: White papule with a brownish central area on the lateral aspect of the left foot |
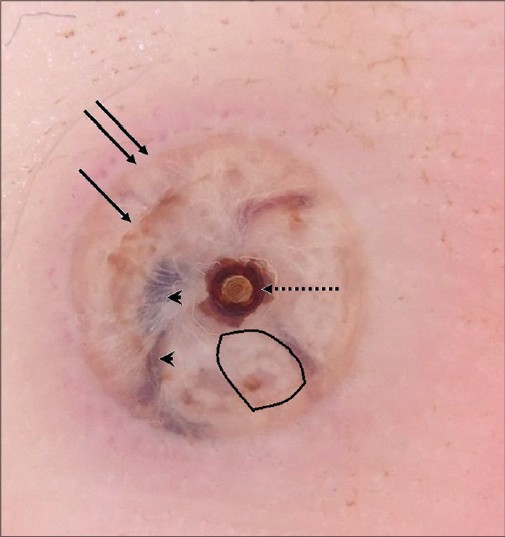 |
| Figure 2: Round lesion with a dark central pore (discontinued arrow), an incomplete radiated crown (single arrow) and a pigmented peripheral ring (double arrow). Within the papule, blue-black blotches (arrow heads) and whitish oval structures linked together forming chain-like structures (demarcated area) can be seen |
 |
| Figure 3: Dermoscopic view of the evacuated eggs and feces |
Tungiasis is a cutaneous infestation, originally from Central and South America, which then spread to sub-Saharan Africa and Asia up to the west coast of India. [1] It is caused by the female flea Tunga penetrans. The flea inhabits dry, sandy soils. The prevalence in endemic areas may reach up to 50%, [2] whereas in non-endemic areas a few cases may be observed among tourists. Skin infections and infestations are the most frequent morbidity encountered among tourists, with tungiasis in the list of top ten dermatological diagnoses among them. [1]
The infestation cycle of the flea lasts for about a month. The fertilized flea introduces itself into the epidermis of the host. It affects humans, dogs, pigs, birds, and other species. The flea fixes its mouth to the blood vessels in the superficial dermis and feeds on blood. Four to five days later, a white papule or nodule appears with a central black dot (the abdominal and genital opening), and the eggs start to develop. The flea grows to about 1 cm in length and from the 8 th to 10 th day onwards, it expels 150 to 200 eggs per day for about 7 to 10 days through the genital opening along with feces, after which it dies.
White papules or nodules with a central black dot can be seen especially over the feet, but any site can be affected. The most common symptom is pruritus, but foreign body sensation has also been reported. [1]
Diagnosis in endemic areas is usually clinical. Dermoscopy, which allows visualization of the submacroscopic epidermal and superficial dermal structures, can be a valuable diagnostic tool in non-endemic areas and in cases with an atypical distribution. A black central pore can be seen, which corresponds to the genital opening of the flea, with a peripheral pigmented ring that corresponds to the posterior abdomen. [3] A radial crown has been described between the pore and the peripheral ring, which is a zone of columnar hemorrhagic parakeratosis in a radial arrangement. [4] Blue-black blotches have also been reported, which are presumed to be the eggs [4] or hematin in the gastrointestinal tract. [3] In some specimens, whitish oval structures linked together forming chain-like structures can be noted, which correspond to the eggs in the flea′s abdomen. [5]
| 1. |
O'Brien BM. A practical approach to common skin problems in returning travellers. Travel Med Infect Dis 2009;7:125-46.
[Google Scholar]
|
| 2. |
Lefebvre M, Capito C, Durant C, Hervier B, Grossi O. Tungiasis: A poorly documented tropical dermatosis. Med Mal Infect 2011;41:465-8.
[Google Scholar]
|
| 3. |
Bauer J, Forschner A, Garbe C, Röcken M. Viariability of dermoscopic features of tungiasis. Arch Dermatol 2005;141:643-4.
[Google Scholar]
|
| 4. |
Marazza G, Campanelli A, Kaya G, Braun RP, Saurat JH, Piguet V. Tunga penetrans: Description of a new dermoscopic sign-the radial crown. Arch Dermatol 2009;145:348-9.
[Google Scholar]
|
| 5. |
Bakos RM, Bakos L. 'Whitish chains': A remarkable in vivo dermoscopic finding of tungiasis. Br J Dermatol 2008;159:991-2.
in vivo dermoscopic finding of tungiasis. Br J Dermatol 2008;159:991-2.'>[Google Scholar]
|
Fulltext Views
7,280
PDF downloads
2,155





