Translate this page into:
Efficacy of red light alone and methyl-aminolaevulinate-photodynamic therapy for the treatment of mild and moderate facial acne
2 Department of Public Health, Facultad de Medicina, Universidad de La Frontera, Temuco, Chile, Clinical Epidemiology Research and Training Center (CERTC), Public Health Doctoral Student, Universidad de Chile, Santiago, Chile
3 Department of Anatomic Pathology, Facultad de Medicina, Pontificia Universidad Cat�lica de Chile, Santiago, Chile
4 Department of Dermatology, Facultad de Medicina, Pontificia Universidad Cat�lica de Chile, Santiago, Chile
Correspondence Address:
Fabiola Schafer
Department of Medical Specialties, Facultad de Medicina, Universidad de La Frontera, Claro Solar St, Temuco
Chile
| How to cite this article: Pinto C, Schafer F, Orellana JJ, Gonzalez S, Hasson A. Efficacy of red light alone and methyl-aminolaevulinate-photodynamic therapy for the treatment of mild and moderate facial acne. Indian J Dermatol Venereol Leprol 2013;79:77-82 |
Abstract
Background: Photodynamic therapy (PDT) has been shown to be an effective alternative for acne. However, there is little information comparing the efficacy of red light alone and methyl aminolaevulinate (MAL)-PDT. Aims: To compare the efficacy and tolerability of red light alone and MAL-PDT in patients with mild to moderate facial acne. Methods: Thirty six patients with mild to moderate acne were enrolled. Eighteen patients recieved MAL-PDT and 18 received red light alone in two sessions, 2 weeks apart. Acne grade and lesion counts were assessed by blinded evaluators at baseline, 2, 4 and 10 weeks. Results: At week 2, clinical improvement from acne grade II-IV to 0-I was observed in 82.3% of MAL-PDT group and 14.2% of red light alone group. Red light alone group had a gradual clinical improvement over time with a 77% response at week 10. In contrast, MAL-PDT group had a rapid clinical improvement with total response at week 10. Both treatments were significantly effective for improving acne lesions. However, MAL-PDT group had a greater response (P < 0.001). Histologically, decreased amounts of sebocytes and lipids along with atrophic sebaceous glands were observed after MAL-PDT. Conclusion: MAL-PDT has a quicker onset of action with a higher response than red light alone. MAL-PDT may induce a reduction in the size of the sebaceous glands and then long-term acne remission.Introduction
Acne vulgaris is a common, chronic inflammatory skin disease that affects mainly adolescents and young adults. [1] There is a wide variety of acne treatments, which reflects the complex and multifactorial pathogenesis of acne. Conventional therapies such as retinoids, benzoyl peroxide and antibiotics are the cornerstone for acne treatment. However, these therapies may not be effective in some cases, leading to refractory acne. In addition, propionibacterial resistance to antibiotics has been increasing over the last years, leading to the constant changing of the guidelines for acne management. [2] Furthermore, cutaneous and systemic side effects including birth defects are important issues stemming from the use of oral isotretinoin. Therefore, alternative treatments are being studied.
Light therapies such as photodynamic therapy (PDT) have been taking an important place in dermatological practices. These procedures may offer alternatives to people who seek topical treatments, quicker onset of action, non-serious side effects and decreased antibiotic resistance rates.
The use of light therapy comes from the fact that Propionibacterium acnes, anaerobic and commensal bacteria on human skin produce endogenous porphyrins, particularly coproporphyrin III (CPIII). Porphyrins may contribute to the inflammatory reaction by producing cytotoxic effects in the sebaceous glands. [3],[4] On the other hand, benefits from the photosensitizing effect of endogenous porphyrins have been described with exposures to blue and/or red light sources. These studies have been shown to reduce 49-75% of inflammatory lesions in treated patients versus 10-25% in untreated patients. [5],[6],[7] Also, acne can respond well to photodynamic therapy using topical porphyrin precursors such as 5-aminolaevulinic acid (ALA) or methyl aminolevulinate (MAL). Photoactivated porphyrins produce the formation of singlet oxygen and other potent oxidizers that induce transient antimicrobial and anti-inflammatory effects. [8] Moreover, red light ALA-PDT has been proven to cause a direct photodynamic destruction of sebaceous glands and then long-term remission of acne. [9] Even though MAL-PDT has been shown to be as effective as antibiotics with a 68% reduction in the number of inflammatory lesions, [10] there is little information comparing the efficacy of red light alone and MAL-PDT treatment.
Therefore, our aim was to compare the efficacy and tolerability of red light alone and MAL-PDT in patients with mild to moderate facial acne. In addition, we investigated the pattern of treatment response for each treatment.
Methods
Patients
Thirty-six patients participated in the study. The protocol was approved by the local ethics committee of the Pontificia Universidad Catolica de Chile and patients signed an informed consent. Patients were recruited from the Department of Dermatology, at the Pontificia Universidad Catolica de Chile from August 2009 to January 2010. An interview was conducted with each patient to determine age, gender, acne grade and medical prescriptions. All patients were older than 15 years of age and had a total of at least 10 inflammatory facial acne lesions. Acne severity grade was classified into mild or moderate facial acne. Patients did not have a history of topical and oral acne treatment within 3 and 6 months of the initiation of the study, respectively. However, all patients had previously been treated with topical retinoids and oral/topical antibiotics. They had relapses and did not respond to this therapy. Also, some women did not want to take oral isotretinoin due to the risk of birth defects.
Treatment
Patients participated in a controlled, investigator-blinded trial. Patients were assigned to MAL-PDT or red light alone group. Dermatologists blinded to treatment evaluated the patients in every follow-up visit. We used a commercial MAL cream 160 mg g 1 ((Metvix® , Laboratory Galderma S.A.) plus red light on one group (18 patients) and red light alone on the other group (18 patients). MAL cream was applied in a 1-mm-thick layer on the whole face (excluding the nose and a 1-cm periocular area). MAL cream was covered with a light impermeable dressing for 90 min and then, both groups were illuminated with non-coherent red light from a Waldman® PDT 1200 lamp (average wavelength 635 nm, light dose 37 J/cm 2 and a fluence rate of approximately 70 mW/cm 2 ) for 9 min. Both treatments were repeated two times, 2 weeks apart.
Evaluation
Patients received either red light alone or MAL-PDT treatment at baseline (0 day) and week 2. They were evaluated at baseline and week 2, 4 and 10. Acne severity grade, inflammatory and non-inflammatory lesions were measured at baseline and at every follow-up visit.
Acne severity grade was evaluated using a six-point rating scale. According to the grading scale, [11] treatment was considered successful when patients achieved grade 0 or I and unsuccessful treatment with grade II to V. In addition, a skin biopsy was performed on one patient in order to analyze morphologic changes of the sebaceous glands.
Furthermore, patients were asked to evaluate their pain during illumination and after treatment. Pain was assessed by means of a numeric scale ranging from 0 to 10 in which 0 is no pain and 10 is the worst imaginable pain. Any other side effects were assessed. Clinical photographs were taken before and after treatment and at every follow-up visit. Patients were also contacted by telephone and e-mail in order to avoid withdrawal from the study.
Statistical Analysis
The sample size was calculated assuming a reported efficacy in reducing acne lesions at the end of the treatment of 75% and 30% for MAL-PDT and red light alone, respectively. [10],[11],[12],[13],[14],[15] With regard to a statistical significant level of 0.05 and a statistical power of 80%, 18 patients on each group were needed.
Statistical summaries using frequency tables, graphs and statistics such as ranks, percentiles, averages and standard deviation were used to describe the study groups.
Inferential analyses were carried out by means of non-parametric tests (Wilcoxon rank-sum and Fisher′s exact test). The statistical model used was GEE for repeated measurements using as a link function the logarithmic function, the family distribution of the dependent variables (number of inflammatory and non-inflammatory lesions was the Poisson distribution) and as a correlation matrix the unstructured matrix. For the dichotomized variable level of acne 0-1/2-4, the family distribution was binomial and the link function was the Inverse Gaussian Cumulative instead of logarithmic because with this function the convergence was not achieved.
Results
Baseline Characteristics
Baseline characteristics for each group are shown in [Table - 1]. Both groups had no statistical differences in age distribution, gender and history of previous treatment (P > 0.05). The average of age was 20.7 (± 3.8) and 22.1 (± 5.8) in the red light alone and MAL-PDT group, respectively. 16.7% and 72.2% of the patients had moderate facial acne (grade III) in the red light alone and MAL-PDT group, respectively (P = 0.001). The median of inflammatory lesion counts was 15 and 52 for the red light alone and MAL-PDT group, respectively (P = 0.0003). The median of non-inflammatory lesion counts was 24 and 33 for the red light alone and MAL-PDT group, respectively (P = 0.038).

Efficacy
Observed efficacy
Clinical improvement was seen 2 weeks after the first MAL-PDT treatment; 82.3% of the patients who had grade II-IV achieved grade 0-I. The median and median percent reduction (%) of inflammatory lesion counts decreased from 52 to 5 (91.3%), 4 (94%) and 0.5 (99.3%) at week 2, 4 and 10, respectively [Figure - 1]. The median and median percent reduction (%) of non-inflammatory lesion counts decreased from 33 to 30 (12.8%), 21.5 (39.4%) and 13.5 (64.5%) at week 2, 4, and 10, respectively [Figure - 2]. At week 10, 100% of the patients achieved grade 0-I [Figure - 3].
 |
| Figure 1: Variation of the number of inflammatory lessions at baseline and follow-up visits after each treatment |
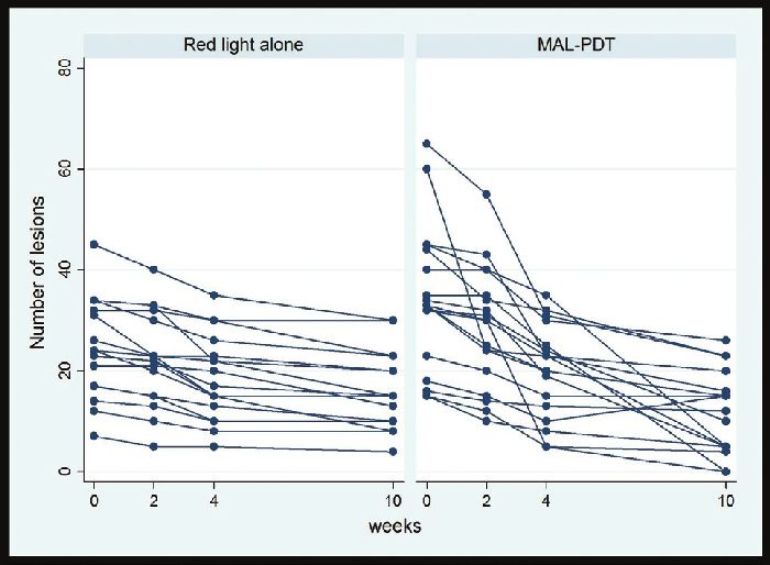 |
| Figure 2: Variation of the number of non-inflammatory lessions at baseline and follow-up visits after each treatment |
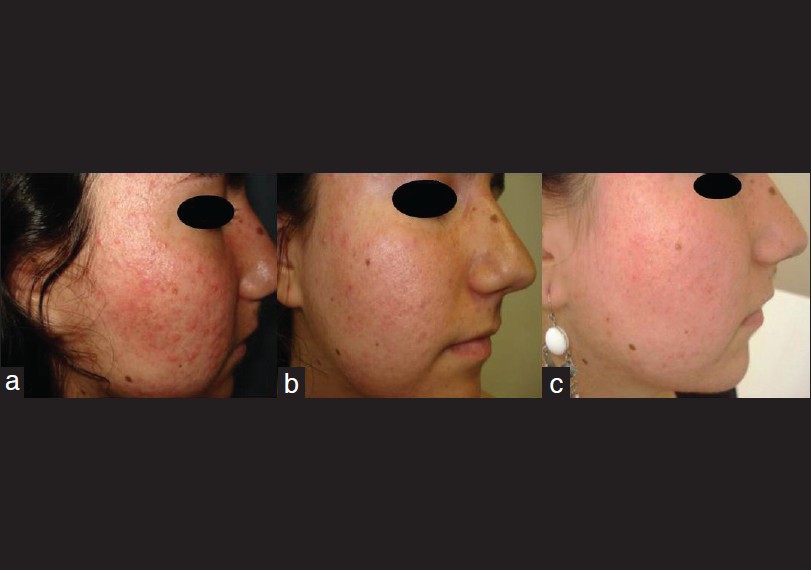 |
| Figure 3: Clinical photographs of a patient with acne grade III, treated with methyl-aminolevulinate-photodynamic therapy at (a) baseline, (b) week 4 and (c) week 10 |
In the red light alone group, 14.2% of the patients who had grade II-IV achieved grade 0-I at week 2. The median and median percent reduction (%) of inflammatory lesion counts decreased from 15 to 11.5 (0%), 5.5 (21.4%) and 5.0 (64.1%) at week 2, 4 and 10, respectively [Figure - 1]. The median and median percent reduction (%) of non-inflammatory lesions decreased from 24 to 22.5 (11.3%), 18.5 (25.9%) and 15 (35.1%) at week 2, 4, and 10, respectively [Figure - 2]. At week 10, 77.7% of the patients achieved grade 0-I [Figure - 4].
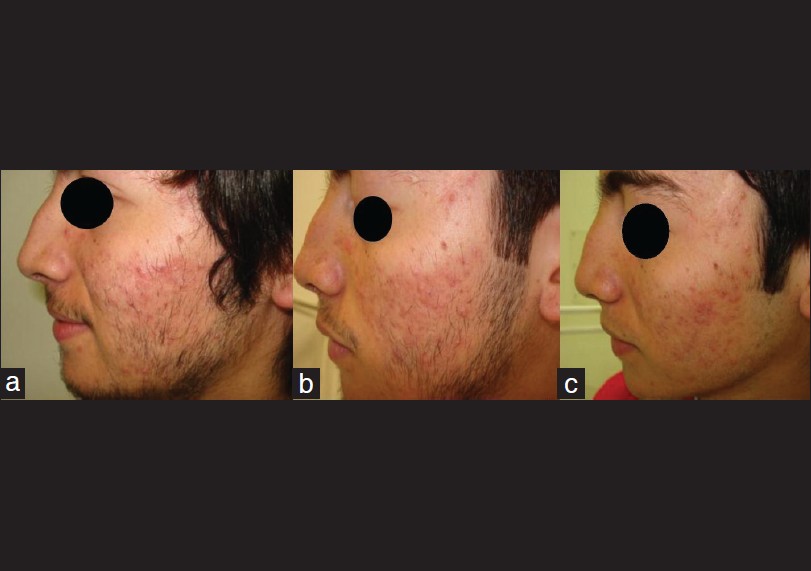 |
| Figure 4: Clinical photographs of a patient with multiple acne scars and inflammatory lesions corresponding to acne grade III, treated with red light alone at (a) baseline, (b) week 4 and (c) week 10 |
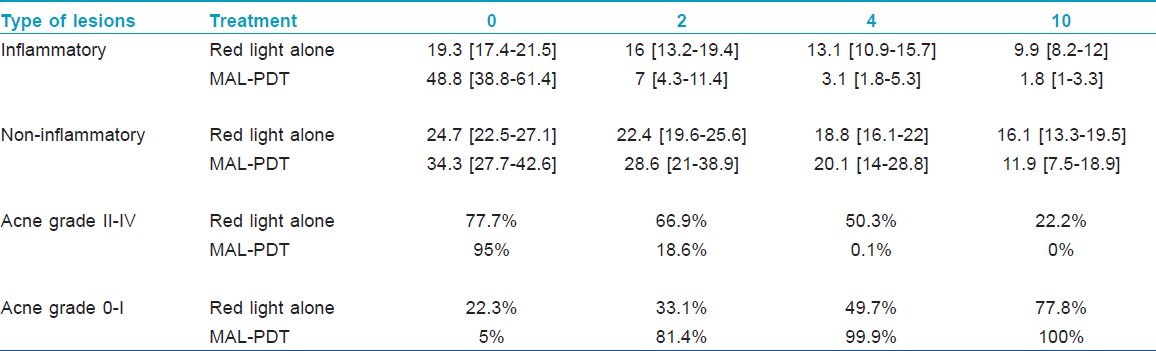
Inference analysis
According to GEE analysis, both treatments showed a significant response by reducing the number of inflammatory and non-inflammatory lesions at every follow-up visit from baseline. However, MAL-PDT group had a greater response than the red light alone group (P < 0.001; GEE model). For each treatment, the expected probability to achieve acne grade 0 or I, and the number of expected inflammatory and non-inflammatory lesions (SD) at week 2, 4 and 10 are shown in [Table - 2].
Adverse effects
Side effects were pain, erythema and epithelial exfoliation. After the first treatment, the median pain score was 2 (inter-quartile range 1-3) and 3 (IQR 2-7) for red light alone and MAL-PDT group, respectively (P = 0.0002). After the second treatment, the median pain score was 1 (IQR 1-3) and 5 (IQR 0-7) for red light alone and MAL-PDT group, respectively (P < 0.001). There were no statistical differences in erythema after the first treatment in both groups, however; MAL-PDT patient group had more moderate and severe erythema after the second treatment (P = 0.012).
A skin biopsy was performed on one patient with moderate inflammatory acne treated with MAL-PDT. In order to analyze morphologic changes of the sebaceous glands, the skin biopsy was taken at baseline (0 day) and seven days after the last MAL-PDT treatment. Both biopsies were taken from her right cheek. At baseline, the sebaceous gland morphology had a conserved structural pattern and its sebum concentration was normal [Figure - 5]a. After MAL-PDT treatment, histopathological findings revealed decreased amounts of sebocytes, reduced amounts of lipids (green color), and atrophic sebaceous glands [Figure - 5]b.
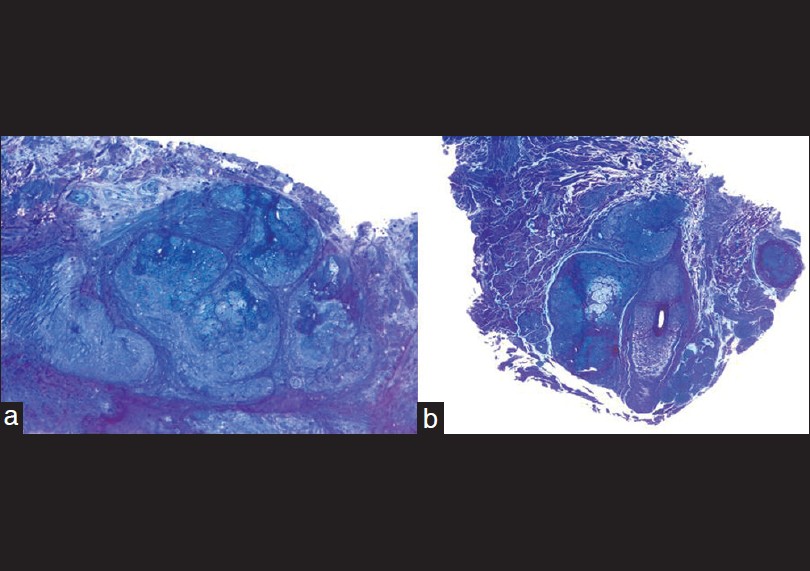 |
| Figure 5: Evaluation of sebaceous gland morphology and its sebum concentration before and after MAL-PDT treatment. (a) Normal architectural pattern of sebaceous glands and follicles with a normal amount of lipids (green color) (toluidine blue staining, original magnification ×200). (b) A smaller size of the sebaceous glands with a reduced number of sebocytes in their central area along with a reduced amount of lipids (green color) (toluidine blue staining, ×200) |
Discussion
This study shows that red light MAL-PDT treatment has a rapid onset of action. At week 2, 82.3% of the patients with grade II-IV achieved grade 0-I. Also, the median of inflammatory lesions decreased from 52 to 5 with a median percent reduction of 91.3%. In contrast, only 14.2% of the patients with grade II-IV achieved grade 0-I in the red light alone group. However, both treatments were significantly effective for improving inflammatory and non-inflammatory lesions. Interestingly, patients from the red light alone group had a gradual clinical improvement over time. In contrast, patients from MAL-PDT group had a rapid clinical improvement with total response at week 10.
This study shows that both treatments significantly reduce acne severity at 10 weeks of follow-up visits, but MAL-PDT has a quicker onset of action with a higher response than red light alone. Hence, red light plus topical porphyrin precursors enhance the phototherapeutic effects with an earlier clinical improvement.
Also of interest, the red light alone group showed a significant reduction in inflammatory and non-inflammatory lesions. Interestingly, Na et al. assessed the efficacy of red light phototherapy using a portable device in facial acne. [12] Eight weeks after treatment, the percent reduction of total lesions was significantly higher in the treated side (55% reduction) compared to the control side (19% increase). This study also showed the beneficial effect of red light on inflammatory acne, which has been attributed to greater skin penetration and greater sensitivity of P. acnes and sebaceous glands to photodestruction. [13] This mechanism may explain the significant clinical response of the red light alone group of our study.
Even though the MAL-PDT group had more patients with severe acne, it showed a better response than the red light alone group. This better response is supported by other studies. As such, a study of MAL-PDT and placebo-PDT using red light (37 J/cm 2 ) showed a median percent reduction in inflammatory lesions of 54% and 20% at 12 weeks after treatment, respectively. [11] Other reports from red light MAL-PDT studies have been shown to reduce 59% to 68% of inflammatory lesions at 12 weeks after treatment. [10],[11],[12],[13],[14] In addition, Riddle et al. showed an analysis of 8 trials and 13 case series related to PDT and acne. All reported reduction in inflammatory lesions of 25-88%, with consistent superiority of PDT over light alone. [15] However, these studies used different light dosimetry and irradiance, skin preparation and drug incubation time. To date, non-uniform parameters are being used for wavelength, light dosimetry, skin preparation, type of precursor and concentration and time of incubation. Therefore, there is no consensus on how to perform PDT for acne treatment. Surely, the modification of these variables may affect the efficacy and side effects. Thus, guidelines for PDT in acne therapy are warranted.
Histological changes such as reduced numbers of sebocytes, reduced amounts of lipids (green color) and a smaller size of sebaceous glands were found in a patient with moderate acne treated with MAL-PDT. For PDT activation, high intensity red light sources have a deeper penetration than blue light sources (Tyndall effect), and are more likely to reach and activate porphyrins in sebaceous glands. [13] This mechanism can produce sebaceous gland destruction and probably a longer remission of acne. Also, red light PDT can induce a reduction in the size and/or function of the sebaceous glands. Theoretically, this effect can be reversible or more permanent depending on the number of treatment sessions. As such, Hongcharu et al. conducted a study of acne patients treated with red light ALA-PDT. [9] The authors reported that sebum excretion was eliminated clinically, and this effect lasted for at least 20 weeks after multiple treatment sessions and 10 weeks after a single treatment. Also, histological findings such as vacuolization of sebocytes and sustained atrophic glands were observed. However, due to the fact that our histopathological findings are based on only one biopsy taken from one patient, we cannot generalize this information to the other patients.
It seems that red light sources in repeated treatment sessions may produce a higher and longer efficacy along with suppression of sebaceous gland functions. As such, this approach would be as efficient as oral retinoids in targeting the sebaceous glands. This theory will be unraveled when PDT is optimized with long-term clinical trials.
In addition, side effects such as pain, erythema and epithelial exfoliation were reported in our study. MAL-PDT treatment was associated with more pain and erythema than red light alone treatment. Intra-group analyses showed that MAL-PDT patients had more severe pain after the second treatment. This situation may be explained by the fact that after illumination there is a superficial burn on the skin surface. Inflammation and epidermal turnover are presented in the damaged skin, so when the second treatment is applied, the skin is thinner and signs of inflammation and epidermal exfoliation can be seen. As such, the skin is more sensitive to illumination, which increases pain and erythema. These side effects have also been reported in other studies. [16],[17] On the other hand, sterile pustular eruption was not seen in any patients.
Taking into account that non-uniform parameters are being used for PDT treatment, there is a need to optimize the treatment protocol to ensure a better result with a long-term acne remission. The results from our study indicate that red light MAL-PDT and red light alone are significantly effective for improving inflammatory and non-inflammatory lesions. Nevertheless, red light MAL-PDT has a quicker onset of action and a higher response than red light alone.
| 1. |
Webster GF. Acne vulgaris. BMJ 2002;325:475-9.
[Google Scholar]
|
| 2. |
Williams HC, Dellavalle RP, Garner S. Acne vulgaris. Lancet 2012;379:361-72.
[Google Scholar]
|
| 3. |
Issa MC, Manela-Azulay M. Photodynamic therapy: A review of the literature and image documentation. An Bras Dermatol 2010;85:501-11.
[Google Scholar]
|
| 4. |
Lee Y, Baron ED. Photodynamic Therapy: Current Evidence and Applications in Dermatology. Semin Cutan Med Surg 2011;30:199-209.
[Google Scholar]
|
| 5. |
Kawada A, Aragane Y, Kameyama H, Sangen Y, Tezuka T. Acne phototherapy with a high-intensity, enhanced, narrow-band, blue light source: An open study and in vitro investigation. J Dermatol Sci 2002;30:129-35.
[Google Scholar]
|
| 6. |
Elman M, Slatkine M, Harth Y. The effective treatment of acne vulgaris by a high-intensity, narrow band 405-420 nm light source. J Cosmet Laser Ther 2003;5:111-7.
[Google Scholar]
|
| 7. |
Smith EV, Grindlay DJ, Williams HC. What's new in acne? An analysis of systematic reviews published in 2009-2010. Clin Exp Dermatol 2010;36:119-23.
[Google Scholar]
|
| 8. |
Sakamoto FH, Lopes JD, Anderson RR. Photodynamic therapy for acne vulgaris: A critical review from basics to clinical practice. Part I. Acne vulgaris: When and why consider photodynamic therapy? J Am Acad Dermatol 2010;63:183-93.
[Google Scholar]
|
| 9. |
Hongcharu W, Taylor CR, Chang Y, Aghassi D, Suthamjariya K, Anderson RR. Topical ALA-photodynamic therapy for the treatment of acne vulgaris. J Invest Dermatol 2000;115:183-92.
[Google Scholar]
|
| 10. |
Wiegell SR, Wulf HC. Photodynamic therapy of acne vulgaris using methyl aminolaevulinate: A blinded, randomized, controlled trial. Br J Dermatol 2006;154:969-76.
[Google Scholar]
|
| 11. |
Hörfelt C, Funk J, Frohm-Nilsson M, Wiegleb Edström D, Wennberg AM. Topical methyl aminolaevulinate photodynamic therapy for treatment of facial acne vulgaris: Results of a randomized controlled study. Br J Dermatol 2006;155:608-13.
[Google Scholar]
|
| 12. |
Na JI, Suh DH. Red light phototherapy alone is effective for acne vulgaris: randomized, single-blinded clinical trial. Dermatol Surg 2007;33:1228-33.
[Google Scholar]
|
| 13. |
Sakamoto FH, Torezan L, Anderson RR. Photodynamic therapy for acne vulgaris: A critical review from basics to clinical practice. Part II. Understanding parameters for acne treatment with photodynamic therapy. J Am Acad Dermatol 2010;63:195-211.
[Google Scholar]
|
| 14. |
Wiegell SR, Wulf HC. Photodynamic therapy of acne vulgaris using 5-aminolevulinic acid versus methyl aminolevulinate. J Am Acad Dermatol 2006;54:647-51.
[Google Scholar]
|
| 15. |
Riddle CC, Terrell SN, Menser MB, Aires DJ, Schweiger ES. A review of photodynamic therapy (PDT) for the treatment of acne vulgaris. J Drugs Dermatol 2009;8:1010-19.
[Google Scholar]
|
| 16. |
Pollock B, Turner D, Stringer MR, Bojar RA, Goulden V, Stables GI, et al. Topical aminolaevulinic acid photodynamic therapy for the treatment of acne vulgaris: A study of clinical efficacy and mechanism of action. Br J Dermatol 2004;151:616-22.
[Google Scholar]
|
| 17. |
Itoh Y, Ninomiya Y, Tajima S, Ishibashi A. Photodynamic therapy of acne vulgaris with topical delta-aminolaevulinic acid and incoherent light in Japanese patients. Br J Dermatol 2001;144:575-9.
[Google Scholar]
|
Fulltext Views
3,535
PDF downloads
1,324





