Translate this page into:
Bullous lesions in leprosy: A rare phenomenon
2 Department of Dermatology, RNT Medical College, Rajasthan, India
3 Department of Dermatology, Jyani clinic, Sriganganagar, India
4 Department of Dermatology, Mahatma Gandhi Institute of Medical Sciences, Jaipur, Rajasthan, India
Correspondence Address:
Uma Shankar Agarwal
397, Shankar Niwas, Sri Gopal Nagar, Gujjar ki Thadi, Jaipur- 302 019
India
| How to cite this article: Agarwal US, Mehta S, Kumar R, Besarwal RK, Agarwal P. Bullous lesions in leprosy: A rare phenomenon. Indian J Dermatol Venereol Leprol 2013;79:107-109 |
Sir,
Bullous lesions in leprosy are rare and may occur during reactions, due to sensory neuropathy or as bullous drug reaction.
During last six months we have come across four cases of leprosy who presented with recurrent bullous and ulcerative lesions along with sensory loss, fever, joint pain with a duration ranging from two weeks to eight years. Clinical data is summarized in [Table - 1].
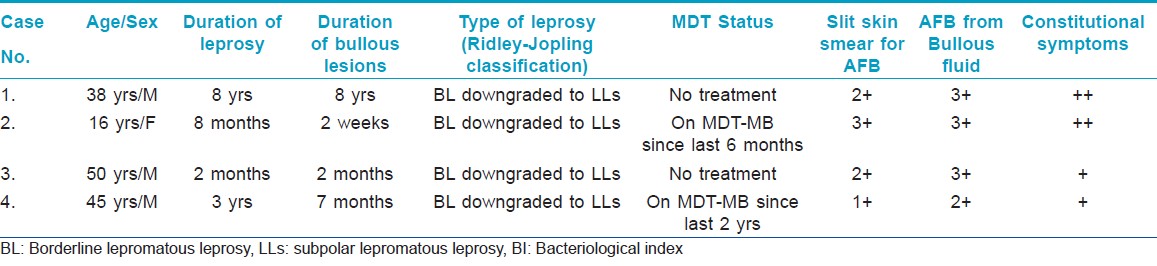
On examination, all patients showed hypoaesthetic, hypopigmented plaques ranging in size from 2 × 3 cm to 10 × 8 cm over the extremities and trunk with variable degree of infiltration over face and back. The ulnar, lateral popliteal and posterior tibial nerves were thickened and tender in all patients. All patients were febrile, and had multiple ulcerative and bullous lesions over the extremities and trunk [Figure - 1] and [Figure - 2]. Bullous lesions ranging from 0.5-2 cm in diameter were present over normal looking skin as well as on erythematous plaques. Most of the lesions were flaccid blisters with areas of erosions after rupture of few such lesions. Tender erythematous papulonodular lesions over extremities were also evident in all patients. There was no sign and symptom suggestive of orchitis, iritis or glomerulonephritis.
 |
| Figure 1: Bullous lesion over left arm (Case one) |
 |
| Figure 2: Multiple bullous and erythematous papulonodular lesions over back (Case three) |
In addition, case one had bilateral, tender cervical lymphadenitis (which may be because of type 2 reaction). Slit skin smear and smear from bullous fluid showed acid fast bacilli (AFB) positivity (Bacteriological index or BI = 2+ and 3+ respectively). Direct immunoflurescence (DIF) for autoimmune blistering diseases was negative. Biopsy from bullous lesion showed suprabasal cleavage [Figure - 3], diffuse and periappendageal lymphohistiocytic infiltrate in dermis with few neutrophils, features of vasculitis like vessel wall damage, extravasation of erythrocytes and leucocytoclasia along with tendency of macrophage granuloma formation (BI = 3+). Considering the histopathological features possibility of borderline lerpromatous leprosy (BL) with erythema nodosum leprosum (ENL) was kept. The patient also had chest X-ray findings suggestive of bilateral pulmonary tuberculosis.
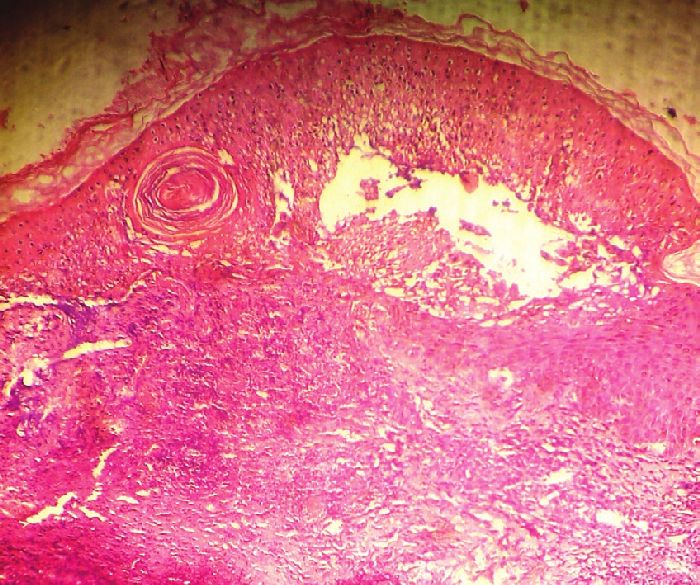 |
| Figure 3: Suprabasal cleavage, neutrophilic and lymphohistiocytic infiltrates in dermis along with vessel wall damage (Case one, H and E Stain, 40×) |
Case two also had a single oral ulcer over the hard palate, which was erythematous 0.5 × 1 cm in size, oval with well-defined border and granulomatous floor. Atrophic scars were also present all over body at sites of previous necrotic ulcers. Slit skin smear and smear from bullous fluid were AFB positive (BI = 3+ in both). Biopsy [Table - 2] showed subcorneal split and lymphohistiocytic infiltrate in dermis along with features of vasculitis.
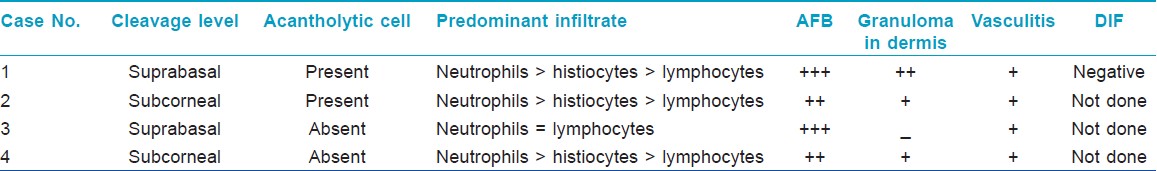
In case three, slit skin smear and smear from bullous fluid were AFB positive (BI = 2+ and 3+ respectively). Biopsy [Table - 2] showed suprabasal split, features of ENL (Vasculitis) and BL (BI = 3+).
Case four also had atrophic scars at multiple body sites. Slit skin smear and smear from bullous fluid [Table - 1] were AFB positive (BI = 1+ and 2+ respectively). Biopsy [Table - 2] showed subcorneal split, features of ENL (Vasculitis) and BL (BI = 2+).
Routine investigation showed leukocytosis (15,000-22,000 cells/mm 3 ) and raised ESR (25-35 mm in first hour) in all patients. Nikolsky′s sign was negative in all patients. Tzanck smear didn′t show acantholytic cells in any of these patients. Other investigations such as urine examination, blood sugar, liver function test, renal function test, ELISA for HIV were normal in all the patients.
Case one and three were given antibiotics and NSAIDs along with MDT-MB and oral steroid (Prednisolone 40 mg/day initial dose). Antitubercular therapy (DOTS Category I) was also started in case one. MDT-MB was stopped in case two and four to rule out drug induced bullous lesions but fresh bullous and papulo-nodular lesions continued to appear. After 15 days, MDT-MB was restarted with antibiotic, NSAIDS and oral steroids (prednisolone 40 mg/day). All the patients showed marked improvement within two month and steroids were gradually tapered in next three month. Ulcer over hard palate healed in one month of starting treatment (Case two).
Bullous lesions are rarely observed in leprosy. In leprosy they may occur in lucio phenomenon, lazarine leprosy, necrotic ENL or as presentation of sensory neuropathy. Other causes may be heat exposure, associated autoimmune bullous disorder; drug induced bullous reactions and other causes of necrotizing vasculitis.
Lucio phenomenon occurs in diffuse, non-nodular form of lepromatous leprosy, chiefly encountered in Mexicans and is seen in untreated patients. Bullae may appear in the center of purpuric, painful, red patches as lucio phenomenon which was ruled out in our patients by presence of fever, nodular lesions, and by absence of purpuric lesions. Lazarine leprosy was described as a type of leprosy in either pole presenting predominantly as bullous and necrotic lesions with generalized infiltrates, loss of eyebrows, fever, gangrene and scarring. Histopathology shows infiltration of neutrophils with marked dilatation, necrosis and thrombosis of capillaries. Our patients didn′t show this kind of clinical and his to pathological features. Bullous lesions may appear on distal extremities in leprosy patients when exposed to heat because of impaired reflex dilatation of skin capillaries due to damaged dermal nerves. Clinical features, nerve involvement, AFB positivity and histopathological features in our patients suggested the final diagnosis of necrotic ENL (with bullous lesions). In severe type of ENL reaction, ulceration may occur because of necrotizing vasculitis. Vesiculobullous, ulcerated, pustular, hemorrhagic and erythema multiforme like lesions have been reported in ENL. [1],[2],[3]
Thappa et al reported co-existence of bullous pemphigoid with lepromatous leprosy. [4] Acantholytic cells [Table - 2] in our cases may be due to secondary acantholysis. Bullous and necrotizing lesions due to rifampicin and dapsone were also reported from India [5],[6]
Though the bullous lesions in leprosy have been reported from different countries including from India but recently we have seen four such cases within a short period of 6 months. Clinicians and dermatologists should be aware of this rare presentation of leprosy which may also be an indicator of the patient having reaction.
| 1. |
Verma KK, Pandhi RK. Necrotic erythema nodosum leprosum: A presenting manifestation of lepromatous leprosy. Int J Lepr Other Mycobact Dis 1993;61:293-4.
[Google Scholar]
|
| 2. |
Dogra S, Kaur I, Kumar B. Bullous reaction in leprosy; A rare phenomenon. Int J Lepr Other Mycobact Dis 2002;70:206-7.
[Google Scholar]
|
| 3. |
Rai VM, Balachandran C. Necrotic erythema nodosum leprosum. Dermatol Online J 2006;12:12.
[Google Scholar]
|
| 4. |
Thappa DM, Rao MV, Garg BR, Ratnakar C. Bullous pemphigoid in lepromatous leprosy. Indian J Lepr 1996;68:251-4.
[Google Scholar]
|
| 5. |
Goel A, Balachandran C. Bullous necrotizing fixed drug eruption with hepatitis due to rifampicin. Indian J Lepr 2001;73:159-62.
[Google Scholar]
|
| 6. |
Dutta RK. Erythema multiforme bullosum due to dapsone. Lepr India 1980;52:306-9.
[Google Scholar]
|
Fulltext Views
4,851
PDF downloads
2,572





