Translate this page into:
Primary cryoglobulinemia with cutaneous features
2 Department of Pathology, Theni Medical College, Theni, India
Correspondence Address:
A S Krishnaram
Department of Dermatology, Madurai Medical college, Madurai 625 001
India
| How to cite this article: Krishnaram A S, Geetha T, P, Saigal A. Primary cryoglobulinemia with cutaneous features. Indian J Dermatol Venereol Leprol 2013;79:427-430 |
Sir,
A 45-year-old agricultural worker presented with pain and discoloration of fingers and toes since 15 days. Symptoms commenced with swelling of both feet associated with pain which lasted for 3 days, followed by discoloration of great toe and inner aspect of both feet. Subsequently, he developed pain and discoloration of fingers of both hands. Patient did not experience any episode of Raynaud′s phenomenon or cold intolerance. No apparent history of insect sting or drug intake could be elicited. He was neither a smoker nor suffered from any long-term systemic illness. General, physical, and systemic examinations were normal with normal blood pressure and peripheral pulses.
Dermatological examination showed dry gangrene of distal half of all fingers [Figure - 1]a and b and patchy tender areas of gangrene with ulceration involving dorsum of foot and toes.
 |
| Figure 1: (a) Gangrene-dorsum of the fingers. (b) Gangrene- ventral aspect of the fingers |
The patient was thoroughly investigated with routine blood and urine investigations being within normal limits. Specific investigations such as viral markers for hepatitis C virus (HCV), hepatitis B virus, and human immunodeficiency virus; serological test for syphilis, rheumatoid factor (RF), antinuclear antibody, antineutrophilic cytoplasmic antibodies, antiphospholipid antibodies, and serum complement levels of C3 and C4 did not reveal any abnormality. Serum protein electrophoresis [Figure - 2] and serum immunological assay showed hypergammaglobulinemia with immunoglobulin M (IgM) level measuring 670 mg/dl (normal: 40-230 mg/dl). Urine examination for paraproteins was negative. Bone marrow study was devoid of any evidence of hematological malignancy. Doppler study of all peripheral vessels, visceral angiogram, and abdominal ultrasonogram was normal. Biopsy from the gangrenous tissue showed necrosis of superficial layers of epidermis, intraluminal amorphous eosinophilic thrombi occluding small vessels of mid-dermis, and sparse inflammatory cell collections [Figure - 3]a and b. Hence, a provisional diagnosis of non-inflammatory vasculopathy due to cryoglobulinemia was considered and thereafter confirmed with the cryoprecipitate test, which was found to be positive [Figure - 4]a and b. Special stain with periodic acid Schiff was considered as an alternative.
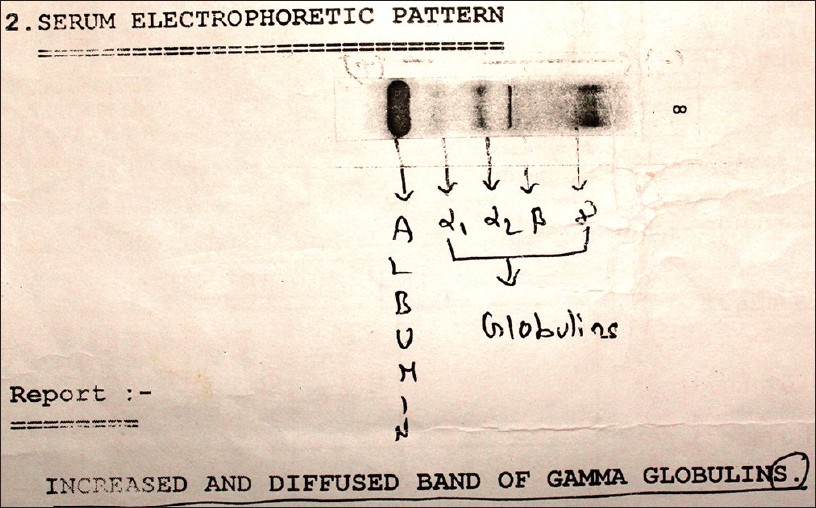 |
| Figure 2: Serum protein electrophoresis showing increased gammaglobulins |
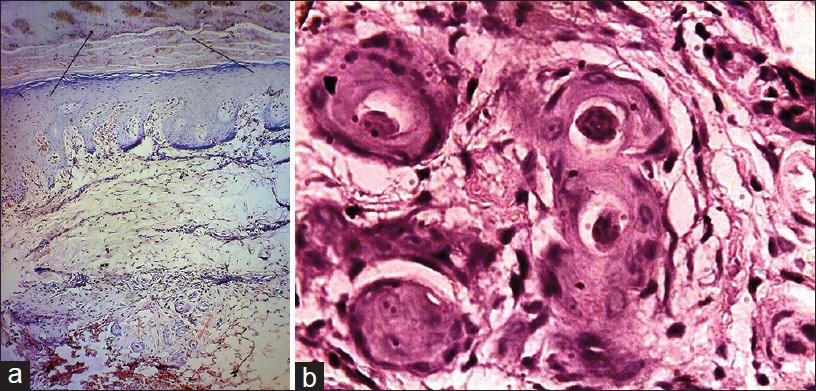 |
| Figure 3: (a) Histopathology showing necrosis of superficial layers of the skin (black arrow) and intraluminal amorphous eosinophilic thrombi (red arrow)-low power (H and E, 4 × 10); (b) Histopathology showing intraluminal amorphous eosinophilic thrombi-high power (H and E, 40 × 10) |
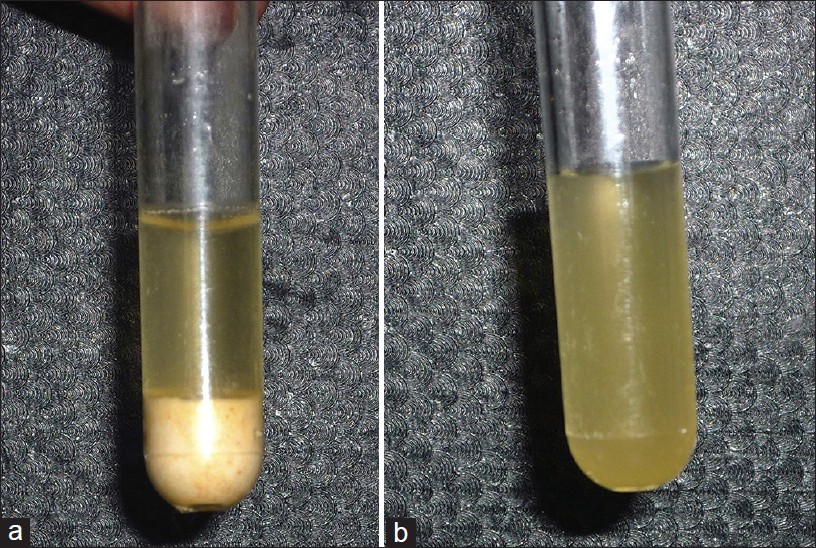 |
| Figure 4: (a) Cryoprecipitate at cold temperature. (b) Disappearance of cryoprecipitate on rewarming |
Parenteral dexamethasone for 2 weeks showed dramatic response with peeling of entire gangrenous tissue. Serum IgM levels came back to normal and steroid was tapered and stopped in 6 weeks. Patient was followed up for 3 years and did not have any recurrence.
Cryoglobulins are single or mixed immunoglobulins that undergo reversible precipitation at temperature below 37°C and dissolve on rewarming. [1] Brouet, et al. [2] classified cryoglobulinemia into three distinct groups: Type I cryoglobulinemia comprises of single immunoglobulin mainly IgM. It is invariably associated with lymphoproliferative malignancies or hematological disorders and rarely occurs without an underlying cause. [3] Type II and type III are mixed cryoglobulins with monoclonal RF (Type II) or polyclonal RF (Type III) complexing with polyclonal IgG mainly. They usually have underlying connective tissue disease, infection, or hepatic disease. Intermediate variant comprising features of types II and III have been described in one study. [4] Ten percent of cryoglobulinemic patients do not have underlying cause and are classified as essential and considered to be resistant to treatment. [5]
The clinical manifestations of type II and type III are essentially due to immune complex cryoglobulinemic vasculitis (leukocytoclastic vasculitis) with various cutaneous lesions and multisystem involvement. Type I cryoglobulinemia is essentially due to self-aggregation through Fc fragment of monoclonal immunoglobulin, with resulting hyperviscosity, thrombosis, ischemia, and vasculopathy, involving skin and kidney. The clinical presentation is usually that of the underlying hematological or lymphoproliferative malignancy.
Cutaneous involvement is seen in 25% of the cases. Palpable purpura is the commonest skin manifestation occurring in 15% followed by Raynaud′s phenomenon, ulcers, skin rash, livedo reticularis, and acrocyanosis in that order of frequency. Digital ischemia and gangrene comprise only 2% of cases with skin involvement. [4] Renal, neurological, and articular involvements occur in 21-38% of the patients. [4]
Essential cryoglobulinemia usually manifests as mixed cryoglobulinemia type II or III.
However, the discovery of a close association between HCV and mixed cryoglobulinemia has practically reduced it to a minority of cases and creates a doubt on the existence of essential cryoglobulinemia. [6] Essential or primary form of Type I cryoglobulinemia has very little reference in the literature. [7] We report a rare case of primary cutaneous cryoglobulinemia, successfully treated and followed up for 3 years.
Digital or acral gangrene is not an uncommon presentation in many clinical specialties. The present case was found interesting, as initial detailed evaluation in the department of medicine did not reveal any underlying cause. Biopsy from the gangrenous area as suggested by the dermatologist showed occlusive vasculopathy giving the first clue toward a diagnosis of cryoglobulinemia. Cryoprecipitate test clinched the diagnosis, which was substantiated by abnormal immunoglobulin assay and serum protein electrophoretic pattern. The characterization of cyroglobulins is technically demanding and was not done. Cryocrit value above 5% is indicative of symptomatic cryoglobulinemia with patients showing palpable purpura, glomerulonephritis, and/or peripheral neuropathy. [4]
Follow-up of the patient for nearly 3 years without any recurrence of skin lesions, normal renal parameters, and immunoglobulin assay establish this case as primary or essential form of type I cryoglobulinemia. The elevated IgM levels in the absence of underlying hematological or lymphoproliferative malignancies can best be considered a part of monoclonal gammopathy of undetermined significance, as mentioned earlier in the literature. [7] Dramatic improvement with parenteral steroids showed the benign nature of the disease.
Interestingly tick bites mimic cryoglobulinemia histologically by showing occlusive vasculopathy. [8] However, absence of history of tick bite, absence of mouthparts, lack of wedge-shaped necrosis, and inflammatory changes excluded its possibility.
To conclude, we report this case of primary cutaneous cryoglobulinemia for its rarity. The importance of performing biopsy and cryoprecipitate test in all cases of digital gangrene where an underlying cause could not be detected has been highlighted.
| 1. |
Cohen SJ, Pittelkow MR, Su WP. Cutaneous manifestations of cryoglobulinemia: Clinical and histopathologic study of seventy-two patients. J Am Acad Dermatol 1991;25:21-7.
[Google Scholar]
|
| 2. |
Brouet JC, Clauvel JP, Danon F, Klein M, Seligmann M. Biologic and clinical significance of cryoglobulins. A report of 86 cases. Am J Med 1974;57:775-88.
[Google Scholar]
|
| 3. |
Barnhill RL, Nousari CH, Xu X, Arksdale SK. Vascular diseases. In: Elder DE, editor. Histopathology of the skin. 10 th ed. Philadelphia: Lippincott Williams and Wilkins; 2009. p. 219-20.
[Google Scholar]
|
| 4. |
Trejo O, Ramos-Casals M, García-Carrasco M, Yagüe J, Jiménez S, de la Red G, et al. Cryoglobulinemia: Study of etiologic factors and clinical and immunologic features in 443 patients from a single center. Medicine (Baltimore) 2001;80:252-62.
[Google Scholar]
|
| 5. |
Ramírez Huaranga MA, Ramos Rodríguez CC, Bellido Pastrana D. Cryoglobulinemia with acronecrosis not associated with hepatitis C infection: A case report. Rheumatol Clin 2012;8:84-6.
[Google Scholar]
|
| 6. |
Trendelenburg M, Schifferli JA. Cryoglobulins are not essential. Ann Rheum Dis 1998;57:3-5.
[Google Scholar]
|
| 7. |
Kagaya M, Takahashi H. A case of type I cryoglobulinemia associated with a monoclonal gammopathy of undetermined significance (MGUS). J Dermatol 2005;32:128-31.
[Google Scholar]
|
| 8. |
Stefanato CM, Phelps RG, Goldberg LJ, Perry AE, Bhawan J. Type-I cryoglobulinemia-like histopathologic changes in tick bites: A useful clue for tissue diagnosis in the absence of tick parts. J Cutan Pathol 2002;29:101-6.
[Google Scholar]
|
Fulltext Views
5,506
PDF downloads
1,378





