Translate this page into:
Eosinophilic panniculitis after subcutaneous administration of sodium heparin
Correspondence Address:
Ana Batalla
Department of Dermatology, Xesti�n Integrada Pontevedra - Saln�s, Hospital Provincial, C/ Dr. Loureiro Crespo, n2. CP 36002, Pontevedra
Spain
| How to cite this article: Batalla A, Ros�n E, Posada C, Fl�rez �. Eosinophilic panniculitis after subcutaneous administration of sodium heparin. Indian J Dermatol Venereol Leprol 2013;79:849 |
Sir,
Cutaneous side-effects of heparins are well-known. Among them, nodule development is uncommon. Usually, these nodules reveal calcinosis cutis on histological examination.
A 66-year-old woman presented with pruriginous lesions on her abdomen, 25 days after initiating oral acenocoumarol and subcutaneous enoxaparin for a pulmonary thromboembolism. On physical examination, multiple tender, poorly delimited, subcutaneous nodules at enoxaparin injection area were evident [Figure - 1]. A biopsy and several complementary studies were performed. Hemogram, erythrocyte sedimentation rate, serum chemistry including alpha-1-antitrypsin, lipase, tryptase, angiotensin I-converting enzyme, rheumatoid factor, thyroid hormone function, autoimmunity studies, urinalysis, chest X-ray and purified protein derivative test were all normal, except for slight eosinophilia with normal white cell count. Cutaneous biopsy showed a mainly septal panniculitis [Figure - 2]. The inflammatory infiltrate was predominantly composed of eosinophils, together with few lymphocytes and histiocytes, within the thickened septa and lobules [Figure - 3]. In the dermis, scant perivascular and interstitial inflammatory cell infiltrate composed predominantly of eosinophils was evident. Mild overlying spongiosis was also identified. A diagnosis of cutaneous drug reaction with eosinophilic panniculitis induced by heparin was made. Enoxaparin injections were discontinued, which resulted in cutaneous improvement. A positive patch test to enoxaparin confirmed this diagnosis.
 |
| Figure 1: Subcutaneous nodules in areas of heparin injection (abdomen) |
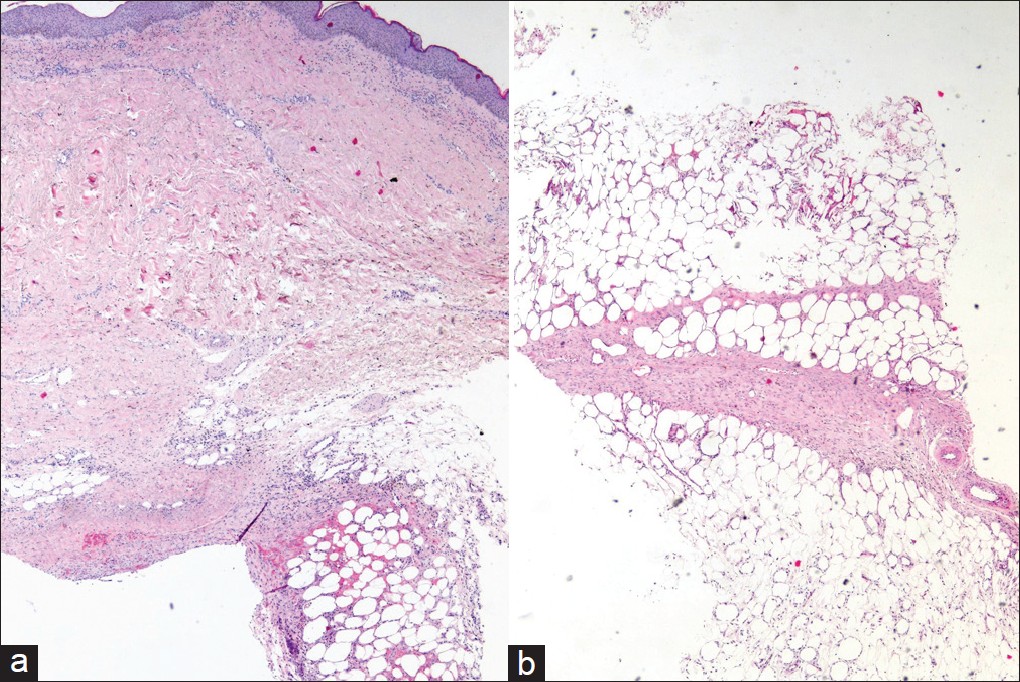 |
| Figure 2: (a and b) Cutaneous drug reaction with eosinophilic panniculitis induced by heparin. Low power view showing inflammatory infiltrate in the upper dermis, thickened septa and lobules (H and E, ×40) |
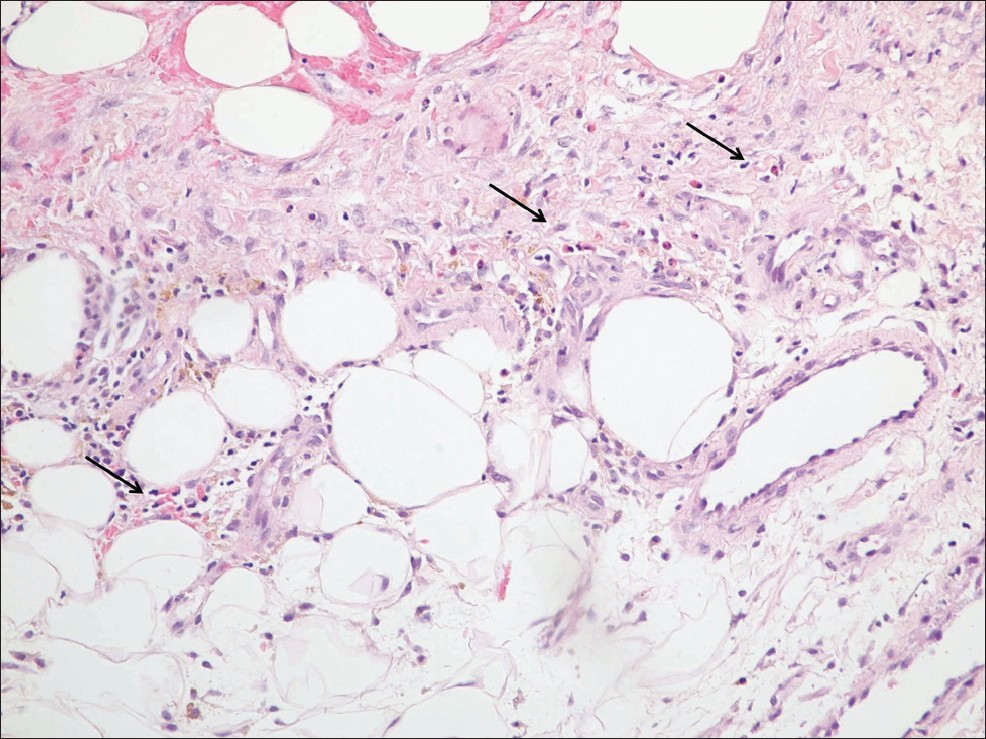 |
| Figure 3: Detail of numerous eosinophils (arrows) in the inflammatory infiltrate in the septum (H and E, ×200) |
The incidence of skin lesions induced by subcutaneous heparin is unknown. Urticaria, angioedema, ecchymosis, cutaneous necrosis, cutaneous induration and eczema-like lesions have been reported secondary to heparin administration. Delayed-type hypersensitivity reactions appear to be the most common mechanism to develop these cutaneous lesions. The presence of nodules or panniculitis caused by heparin has rarely been described. [1] The majority of these patients presented with calcinosis cutis or subcutis on histological examination and only one case of eosinophilic panniculitis was reported. Most patients with nodules were receiving treatment with calcium non-fractionated heparins or low molecular weight heparins (LMWH) containing calcium salts. On the other hand, patients with calcinosis cutis following subcutaneous heparin injection usually suffered from vitamin D, parathyroid hormone or calcium-phosphate disturbances. [2] Nodules induced by sodium LMWH have also been found. Funt et al. observed nodules in 14 of 426 cancer patients following dalteparin (heparin with sodium salts) injection. These authors described the radiological characteristics of these nodules, but histological studies were not performed. [3]
Regarding to acenocoumarol, the absence of reported cases of panniculitis caused by this drug as well as the involution of cutaneous lesions despite continuing with this treatment, helped us to exclude acenocoumarol as a possible cause of the lesions of our patient.
Eosinophilic panniculitis is a rare form of panniculitis characterized by septal and lobular involvement with eosinophilic infiltration. It is believed to be a reactive process that has been associated with a variety of systemic conditions such as gnathostomiasis, leukocytoclastic vasculitis and erythema nodosum. [4] In rare instances, eosinophilic panniculitis has been observed as a local phenomenon induced by subcutaneous or intramuscular drug injections including apomorphine, specific immunotherapy, benzathine penicillin and calcium heparin. [1],[5] Delayed-type hypersensitivity reactions have also been considered as the cause of these reactions. [5]
Conclusion
To the best of our knowledge, this is the first case of eosinophilic panniculitis induced by administration of LMWH containing sodium salts.
| 1. |
Yasuda M, Abe M, Yamanaka M, Amano H, Tamura A, Ishikawa O. Eosinophilic panniculitis and hypereosinophilia caused by hypersensitivity to calcium heparin. Eur J Dermatol 2010;20:401-2.
[Google Scholar]
|
| 2. |
Campanelli A, Kaya G, Masouyé I, Borradori L. Calcifying panniculitis following subcutaneous injections of nadroparin-calcium in a patient with osteomalacia. Br J Dermatol 2005;153:657-60.
[Google Scholar]
|
| 3. |
Funt SA, Hidalgo A, Panicek DM. Subcutaneous nodules at the injection site of low-molecular-weight heparin: A mimic of metastatic disease at CT. J Comput Assist Tomogr 2002;26:520-3.
[Google Scholar]
|
| 4. |
Adame J, Cohen PR. Eosinophilic panniculitis: Diagnostic considerations and evaluation. J Am Acad Dermatol 1996;34:229-34.
[Google Scholar]
|
| 5. |
Masferrer E, Martin-Ezquerra G, Martínez-Escala E, Pujol RM, Giménez-Arnau A. Eosinophilic panniculitis triggered by intramuscular penicillin and occupational setting. Allergy 2011;66:436-7.
[Google Scholar]
|
Fulltext Views
3,898
PDF downloads
3,166





