Translate this page into:
A 4-year multicentric experience of intravenous cannula-based intralesional radiofrequency ablation as an effective and safe office procedure for common cutaneous nodules
Corresponding author: Dr. Saurabh Singh, Associate Professor, Department of Dermatology, Venereology and Leprology, All India Institute of Medical Sciences, Basni Phase 2nd, Jodhpur - 342 005, Rajasthan, India. saurabhdoc@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Singh S, Passi S. A 4-year multicentric experience of intravenous cannula-based intralesional radiofrequency ablation as an effective and safe office procedure for common cutaneous nodules. Indian J Dermatol Venereol Leprol 2021;87:433-5.
Sir,
Radiofrequency surgery generates heat which may cause collateral damage responsible for side effects. A solution to this problem has been the availability of insulated radiofrequency probes which have been primarily utilized outside the domain of dermatology. Innovation in this regard has been intralesional radiofrequency utilizing the conventional radiofrequency probes and intravenous cannula,1-3 but we feel it has not been examined well in literature.
A retrospective file review was performed for patients with predominantly deep dermal lesions of non-infective, cystic or vascular nature, operated at 2 centres (Primarily operated by SS. SP helped intraoperatively and collected follow up data at ESIC center) between August 2014 and September 2018 who had consented for the minimally invasive method as an alternative over conventional surgical excision. Only those patients who completed at least 1 post-operative follow-up visit were included. All intralesional radiofrequency procedures were performed under local anaesthesia. The procedure of intralesional radiofrequency was basically performed as per the previously published report,1 with some improvisations. Using a 15-number surgical blade, a small window was created in the plastic sheath of an intravenous cannula. This cannula, intact with the metallic trocar, was then inserted inside the lesion until appropriate depth so that the window remained outside the tissue. The cannula was initially inserted to its maximum insulated length, radiofrequency energy coagulation mode was delivered by touching the probe to the exposed window and then cannula was withdrawn gradually [Video 1]. A fine crackling sound and bubbles with tissue fluid inside the cannula indicated coagulation of dermal tissue by radiofrequency energy which occurred throughout the procedure.
Overall, 24 patients (male : female = 1.4) with a mean age of 29.6 ± 15.3 years and with various diagnoses underwent the procedure. The relevant median values of the studied patients are mentioned in Table 1. A pre-operative radiological evaluation was done in the form of sonography for lesions deeper than 1–2 centimeters (1 sebaceous cyst and 1 ganglion), doppler ultrasound scan for swellings of vascular nature (2 lymphatico-venous malformations) and a magnetic resonance imaging (1 lymphangioma circumscriptum). The cannula insertion techniques to cover the lesion in entirety included multiple pass ‘fanning’ and ‘cross-hatching’, each pass lasting 5 to 10 seconds followed by a brief thaw period of 1-2 seconds. Endpoint of intralesional radiofrequency was either complete coverage with a palpable rise in surface temperature or blanching of superficial skin with peau d’orange appearance which indicated that cannula had reached the dermoepidermal junction. Using an 18 gauge needle-stab puncture, the contents of ganglions and sebaceous cysts were expressed out gently, as far as possible, before intralesional radiofrequency. For pyogenic granulomas, the intralesional radiofrequency was performed through adjoining normal skin directed to the base of the lesion, following which lesion was shaved off using cutting mode.
| Diagnosis | Site | Total patients | Median disease duration (Months) |
IQR | Median radiofrequency sittings |
IQR | Median follow up (Months) |
IQR | Median PGA |
IQR | Median IGA |
IQR |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ganglion | Foot, wrist, ankle | 5 | 5 | 101.5 | 1 | 0 | 4 | 2.5 | 10 | 2.5 | 10 | 3.5 |
| Sebaceous cyst | Back, cheek, forehead, eyebrow | 5 | 12 | 75 | 2 | 0.5 | 7 | 11 | 9 | 3 | 9 | 3.5 |
| Pyogenic granuloma | Scalp, nail bed, cheek | 5 | 2 | 3.25 | 1 | 0 | 7 | 16.5 | 10 | 0 | 10 | 0 |
| Lymphatic malformation | Buttock, groin, pubis, thigh | 4 | 180 | 342 | 2 | 2 | 18 | 11 | 9 | 2 | 9 | 2.5 |
| Acne cyst | Cheek | 3 | 6 | 9 | 1 | 0 | 18 | 3 | 10 | 0 | 10 | 0 |
| Hypertrophic/Keloidal Scar | Temple, presternal | 2 | 34 | 53 | 1.5 | 1 | 10 | 10 | 8 | 4 | 7.5 | 5 |
Mean number of intralesional radiofrequency sessions was 1.25 ± 0.6 (1 to 3). The improvement was recorded on a scale of 0 to 10 (latter meaning complete remission) by both patients and physicians. The patients reported significant relief and reported mean improvement to be 9.1 ± 1.3 and that by physicians was reported was 8.9 ± 1.7 [Figures 1-3]. Patients were followed up for a mean period of 9.1 ± 5.8 months and 4 patients showed recurrence (2 ganglions and 2 sebaceous cysts) after 3 to 5 months of intralesional radiofrequency. Overall, the vascular lesions and acne cysts benefitted the most. On the whole, the therapy was well tolerated with minor side effects like mild atrophic scarring in 3 patients and hyperpigmentation in 2. None of the patients developed hypopigmentation or depigmentation.

- Pyogenic granuloma on scalp

- After being subjected to intralesional radiofrequency, appearing shrunken and blanched

- At 14 months follow-up after intralesional radiofrequency and superficial shave radiofrequency
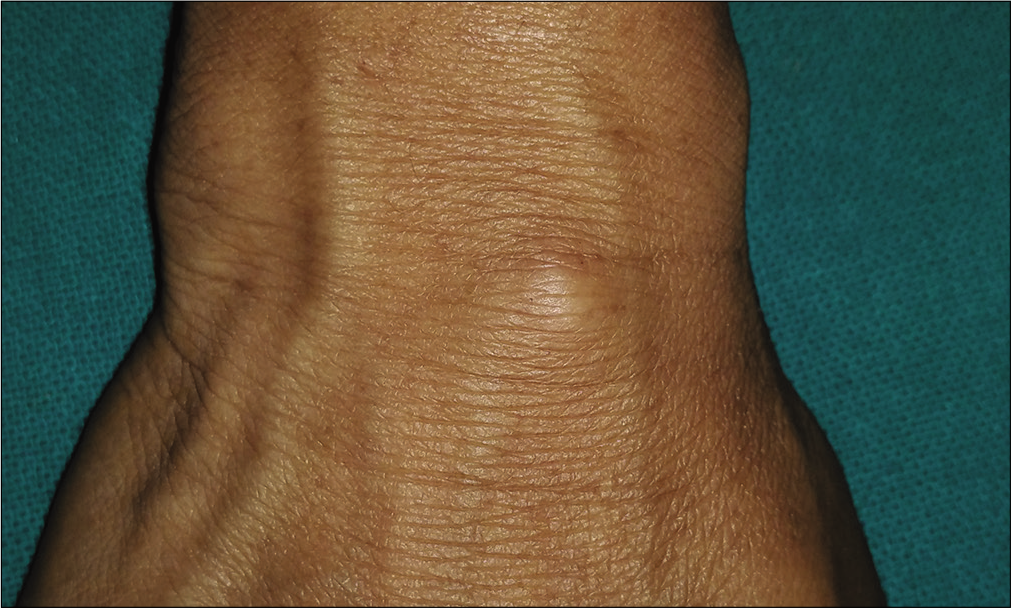
- Ganglion on right wrist
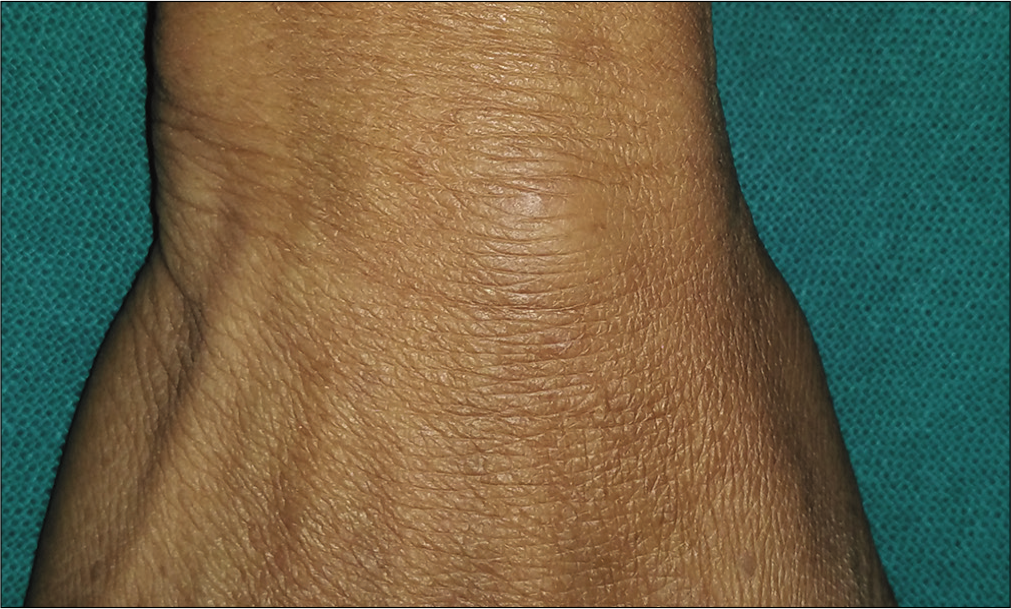
- At 6 months follow-up after a single sitting of intralesional radiofrequency, lesion subsided by >90%

- Lymphangiectasias on the pubic area

- At 14 months follow-up after 2 sittings of intralesional radiofrequency, lesions resolved significantly without scarring or recurrence
Intralesional radiofrequency is still evolving and various studies have used different methods ranging from a surface application for venous malformations, inserting insulated probes in keloids to inserting uninsulated hypodermic needles in angiolymphoid hyperplasia.4-6 This particular technique is inexpensive and minimizes operative scars in the management of innocuous swellings of aesthetic concern and previous reports highlight the same.1-3
The only prior literature on intralesional radiofrequency using similar technique differs from our study with lower mean patient and physician scores (7.6 ± 2.22 and 7.3 ± 2.42), the higher number of radiofrequency sessions used (2.26 ± 1.61), with a longer follow-up (11.4 ± 11.6 months) and lower recurrence (1 case). We used a palpable rise in temperature or blanching of skin as an endpoint whereas Subhadarshani et al. used the induration of lesion as the endpoint for stopping radiofrequency.3 We, in addition, ensured complete coverage of lesions using techniques like fanning and cross-hatching.
Even though intralesional radiofrequency technique has an inherent disadvantage as it is a blind procedure and simultaneously occupies both hands to hold the intravenous cannula and radiofrequency probe, it is mastered easily with practice. A small number of cases was another limitation of our study. Radiological guidance like pre-operative or intra-operative ultrasound may enhance the results with this technique.
Acknowledgement
We would like to thank the faculty colleagues and residents of department of dermatology at All India Institute of Medical Sciences, Jodhpur, for rendering help with patient care.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Intralesional radiofrequency ablation for nodular angiolymphoid hyperplasia on forehead: A minimally invasive approach. Indian J Dermatol Venereol Leprol. 2014;80:419-21.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and safety of a novel method of insulated intralesional radiofrequency ablation for deep dermal and subcutaneous lesions: A 3 year institutional experience. Dermatol Surg. 2018;44:714-20.
- [CrossRef] [PubMed] [Google Scholar]
- Angiolymphoid hyperplasia of external ear treated with intralesional radiofrequency ablation. BMJ Case Rep. 2018;2018:bcr2017223447.
- [CrossRef] [PubMed] [Google Scholar]
- Intralesional radiofrequency in venous malformations. Br J Oral Maxillofac Surg. 2015;53:213-6.
- [CrossRef] [PubMed] [Google Scholar]
- Radiofrequency tissue volume reduction for treatment of auricle keloids. Laryngoscope. 2011;121:1233-6.
- [CrossRef] [PubMed] [Google Scholar]
- Angiolymphoid hyperplasia with eosinophilia showing promising result with intralesional radio frequency ablation therapy: A new cost effective and hassle free modality of treatment. J Cutan Aesthet Surg. 2016;9:281-3.
- [CrossRef] [PubMed] [Google Scholar]





