Translate this page into:
A case of a reddish umbilical tumor: An uncommon presentation of a viral wart
2 Department of Pathology, Licenciado Adolfo López Mateos Regional Hospital, ISSSTE, Mexico City, Mexico
3 Department of Dermatology, Licenciado Adolfo López Mateos Regional Hospital, ISSSTE, Mexico City, Mexico
Correspondence Address:
Uriel Villela-Segura
Esquina, Eje Vial 3 Sur, Dr José María Vertiz 464, Buenos Aires, Cuauhtémoc, BO: 06780, Ciudad de México, CDMX
Mexico
| How to cite this article: Villela-Segura U, De La Torre-Rend�n F, Ram�rez-S�enz S, Barr�n-Tapia MT. A case of a reddish umbilical tumor: An uncommon presentation of a viral wart. Indian J Dermatol Venereol Leprol 2020;86:709-711 |
Sir,
Condyloma acuminatum or genital warts are sexually transmitted disease caused by human papillomavirus. Low-risk human papillomavirus 6 and human papillomavirus 11 types are responsible for 90% of the cases; however, high-risk types like 16 and 18 can also be causative agents. The genital area is the most commonly affected site although there are several cases reported involving other anatomical sites.[1]
A 23-year-old healthy man, judo wrestler, attended the dermatology department of the Hospital Regional Lic. Adolfo López Mateos, Mexico City with a 1-month history of malodorous umbilical discharge, followed by a growing umbilical mass. There was no history of prior surgical procedures. Cutaneous examination revealed a red-violaceous, tender, exophytic tumor measuring 2 × 2.5 cm, with serous discharge and periumbilical erythema. [Figure - 1]. The rest of the physical examination was normal. The patient was single and denied any sexual contact in the last year, although he had a previous history of sexual contact with four healthy partners.
 |
| Figure 1: Umbilical warty red-violaceous tumor with periumbilical erythema |
Considering the history, evolution and the site of presentation, the possible diagnosis was a viral wart versus a patent urachus, the latter was ruled out with a normal computed tomography scan. Skin biopsy from the umbilical warty lesion revealed parakeratosis, acanthosis with papillomatosis and koilocytes in the upper epidermis [Figure - 2]. Anyplex™ II multiplex real-time polymerase chain reaction detected the presence of human papillomavirus 11. Serological tests for HIV, hepatitis B virus, hepatitis C virus and Venereal Disease Research Laboratory test were normal. The patient denied having any personal history of genital warts or any unusual sexual practices. Contact tracing of his former sexual partners and current wrestling partners was unsuccessful.
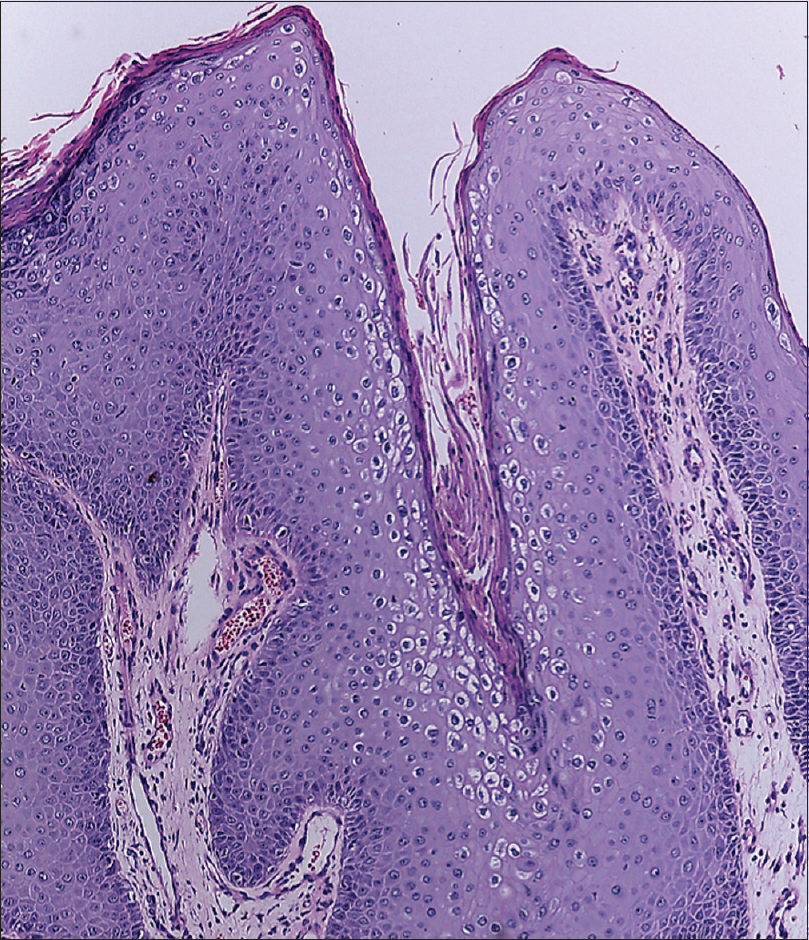 |
| Figure 2: Epidermis with parakeratosis, acanthosis, papillomatosis and presence of koilocytes (H and E, ×200) |
The patient underwent surgical excision followed by topical imiquimod 5% cream three times weekly for 16 weeks [Figure - 3]. The condition resolved without any recurrence or appearance of new lesion during his follow-up 1 year later.
 |
| Figure 3: Clinical appearance after excisional biopsy |
The mode of transmission of human papillomavirus is through skin-to-skin contact, autoinoculation and less commonly vertical transmission.[1] In our case, he could have acquired the infection through previous close skin contact with one of his previous sexual partners or an infected wrestling partner with an unnoticed lesion.
The incubation period ranges from 3 weeks to 8 months. Sexually transmitted viral warts are usually seen on genitalia, perineum and adjacent areas. The extragenital presentation is uncommon with reported cases located on breast or axilla, and this could be associated with nonconventional sexual practices. Umbilical manifestation is exceptional with two reported cases in the medical literature (none of them confirmed with polymerase chain reaction).[2] This entity has been described as a sessile, skin-colored, whitish or brown papilloma, with an exophytic surface. Most cases are asymptomatic; however, discomfort, irritation and bleeding may occur on contact with clothing. Some patients can complain of malodorous discharge. Histologically, there is the presence of acanthosis, papillomatosis, and hyperkeratosis with parakeratosis along with the presence of koilocytes which is a distinctive feature.[3]
Differential diagnoses for umbilical tumors include patent urachus, hypertrophic scar, pyogenic granuloma, endometriosis in women and umbilical metastasis, referred to as “Sister Mary Joseph's nodule,” which is most commonly associated with malignancy of an ovarian origin and less commonly in cases of malignancy affecting pancreas, gastrointestinal tract and lymphoma.[4]
Based on the size of the wart and its rapid evolution surgical excision was chosen as the first therapeutic option in our patient. To avoid recurrence, additional treatment with imiquimod 5% cream was prescribed.
We were unable to find similar cases in medical literature reporting umbilical localization of a viral wart, confirmed by polymerase chain reaction.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Hawkins MG, Winder DM, Ball SL, Vaughan K, Sonnex C, Stanley MA, et al. Detection of specific HPV subtypes responsible for the pathogenesis of condylomata acuminata. Virol J 2013;10:137.
[Google Scholar]
|
| 2. |
Vijayabhaskar R, Sadasivam OL, Kirushnakumar KS. Papilloma of the umbilicus. Indian J Surg 2014;76:329-30.
[Google Scholar]
|
| 3. |
Vyas NS, Campbell CM, Mathew R, Abrahamsen M, van der Kooi K, Jukic DM, et al. Role of histological findings and pathologic diagnosis for detection of human papillomavirus infection in men. J Med Virol 2015;87:1777-87.
[Google Scholar]
|
| 4. |
Psarras K, Symeonidis N, Baltatzis M, Notopoulos A, Nikolaidou C. Umbilical metastasis as primary manifestation of cancer: A small series and review of the literature. J Clin Diagn Res 2014;8:ND17-9.
[Google Scholar]
|
Fulltext Views
4,347
PDF downloads
1,887





