Translate this page into:
A case of disseminated histoplasmosis presenting with facial and laryngeal involvement
2 Department of Pathology, All India Institute of Medical Sciences, New Delhi, India
Correspondence Address:
Sujay Khandpur
4th Floor, Teaching Block, Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi - 110 029
India
| How to cite this article: Sondhi P, Singh S, Khandpur S, Agarwal S. A case of disseminated histoplasmosis presenting with facial and laryngeal involvement. Indian J Dermatol Venereol Leprol 2020;86:470 |
Sir,
Histoplasmosis is an infectious systemic mycosis caused by Histoplasma capsulatum in Americas and tropics and Histoplasma duboisii in Africa. Although, the disease occurs more commonly in immunocompromised cases, it has also been well-documented in immunocompetent individuals. Herein, we report a case of disseminated histoplasmosis with involvement of the face and larynx in a 69-year-old man. The case is interesting in view of the atypical morphology of cutaneous lesions that clinically mimicked other dermatoses. The recent development of facial lesions in this patient which were confirmed to be of histoplasmosis was an important clue and guided the otorhinolaryngologists in considering the diagnosis of concomitant laryngeal histoplasmosis.
A 69-year-old man presented to us in the dermatology outpatient department with asymptomatic skin lesions over both cheeks and forehead of 3 months duration. They started as erythematous papules and plaques, with some plaques developing superficial ulcers with a purulent discharge. He also had hoarseness of voice and dysphagia for the same duration. His medical history revealed persistent cough, hoarseness of voice, pain in throat, and dysphagia 14 years back which was diagnosed as laryngeal tuberculosis based on a laryngeal biopsy that revealed epithelioid cell granulomas with caseous necrosis. He was adequately treated with antitubercular therapy that led to resolution of all his symptoms in 6 months and he was asymptomatic for the next 13 years. He was also diagnosed with adrenal tuberculosis 16 years back based on history of significant weight loss, generalized weakness, and anorexia and an adrenal mass detected on abdominal computed tomography (CT) scan, for which he was treated adequately with antitubercular therapy. The symptoms resolved; however, he developed adrenal insufficiency for which he is on maintenance dose of 5 mg prednisolone once daily. He is a known case of diabetes mellitus for the past 30 years which is well-controlled with oral hypoglycemic drugs and dietary modifications. There was no history of significant weight loss, anorexia, or night sweats during current illness.
Dermatological examination revealed erythematous papules and plaques on the forehead, upper eyelids, both cheeks, and chin, with superficial ulceration in few plaques [Figure - 1]. We kept a differential diagnosis of sarcoidosis, tumid lupus erythematosus, granulomatous rosacea, Jessner's lymphocytic infiltrate, and granuloma faciale.
 |
| Figure 1: Multiple, well-defined, erythematous papules and plaques over the face with superficial ulcerations in few |
A skin biopsy from a facial plaque revealed pan-dermal dense inflammatory infiltrate composed of epithelioid cell granulomas with many Langhans and foreign body giant cells, lymphocytes, histiocytes, and few neutrophils [Figure - 2]a. Numerous fungal spores with a typical halo suggestive of Histoplasma capsulatum were identified within histiocytes and giant cells, which were highlighted on PAS stain [Figure - 2]b.
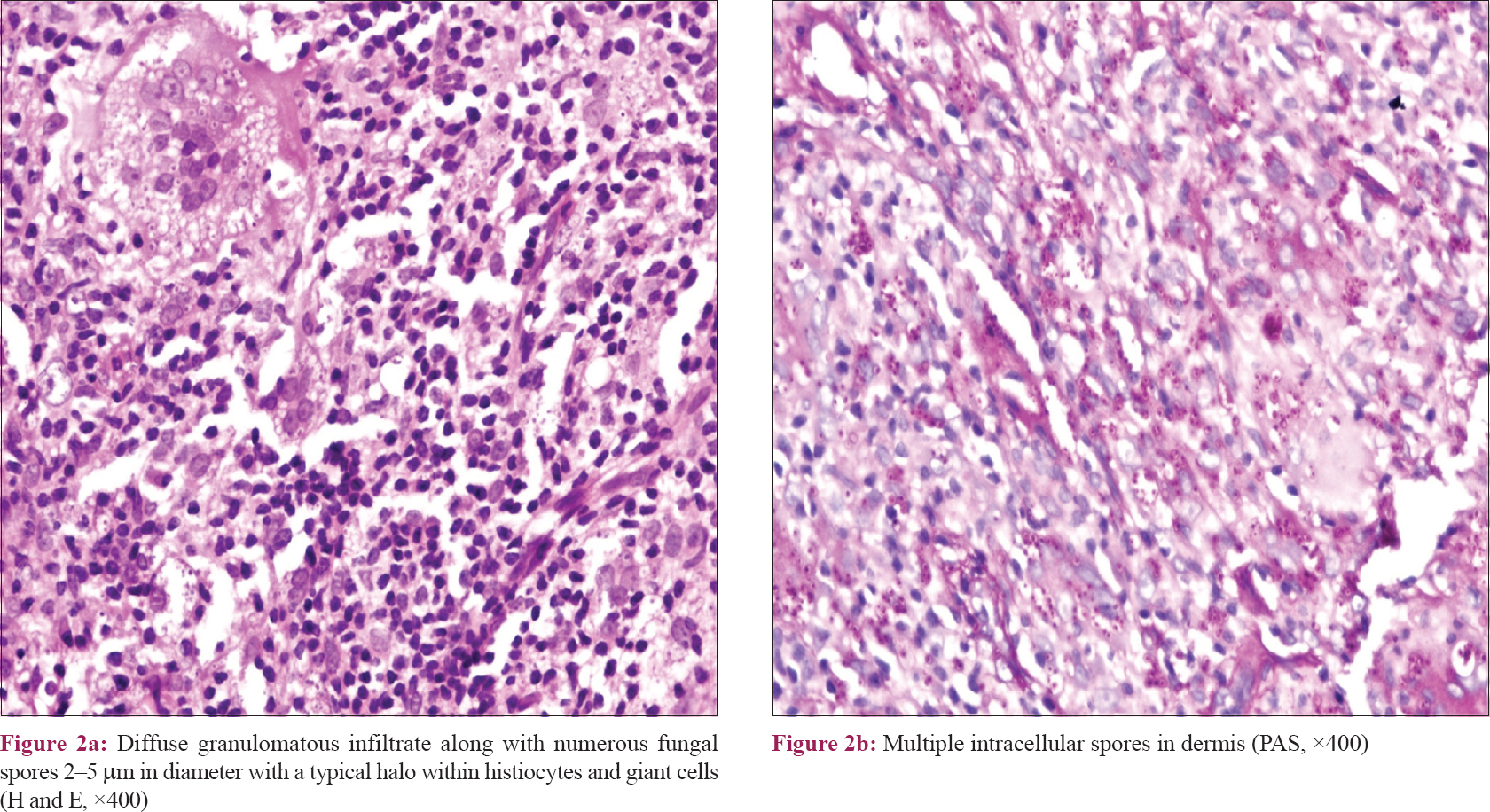 |
| Figure 2: |
The laryngoscopic evaluation showed congestion of left endolarynx and edema of false and true vocal cords and arytenoids. The proliferative lesion was observed to be in the left false vocal cord/arytenoid cartilage region.
Laryngeal biopsy was deferred since the otolaryngologist opined that the procedure involves significant risk, and the skin and laryngeal disease processes might be similar. A CT scan of the neck, chest, abdomen, and pelvis revealed diffuse edema in true and false vocal cords, emphysematous changes in both lungs with fibrotic opacities, and bilateral bulky adrenal glands with foci of coarse calcifications [Figure - 3]a and [Figure - 3]b. On further probing, the patient revealed history of significant exposure to bird droppings since the last 10 years. Serological testing for human immunodeficiency virus (HIV) was negative.
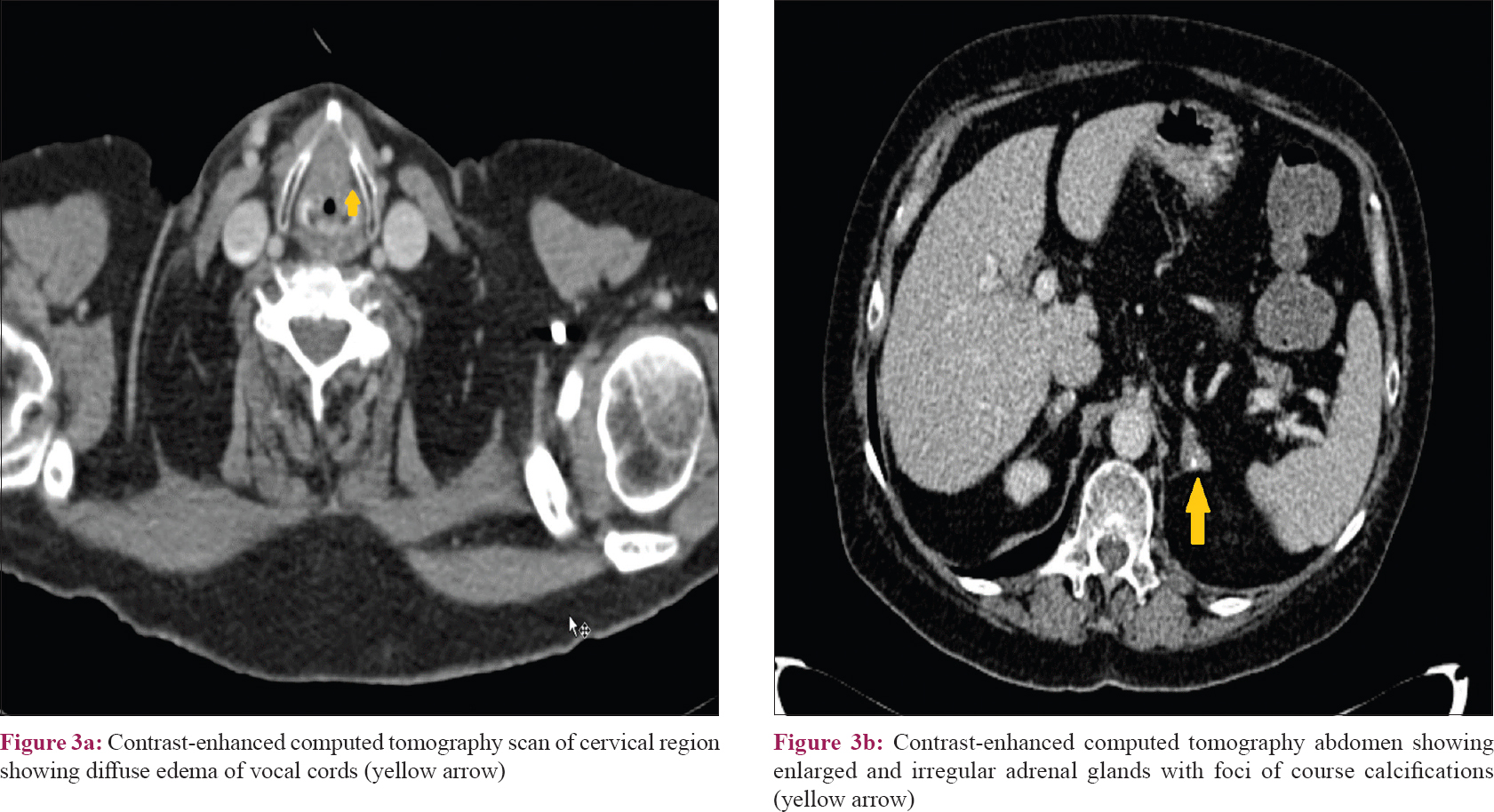 |
| Figure 3: |
A diagnosis of cutaneous and laryngeal histoplasmosis was made. The patient was administered capsule itraconazole 200 mg twice daily that led to resolution of all facial lesions in 4 months with atrophy. There was also complete improvement in hoarseness of voice and dysphagia. The patient received total 12 months of itraconazole, 200 mg twice daily, and is symptom-free at further 1 year of follow-up [Figure - 4].
 |
| Figure 4: Subsidence of erythematous papules and plaques with atrophy after 6 months of oral itraconazole therapy |
Histoplasmosis is acquired by inhalation of fungal spores (conidia). The true prevalence of this mycosis is still underappreciated as the condition goes unrecognized for long periods due to low awareness among physicians and misdiagnosed as tuberculosis or leishmaniasis.[1],[2]
A majority (99%) of the patients have a self-limiting infection of the lungs, while remaining 1% progress to either disseminated or chronic disease involving the lungs, liver, spleen, lymph nodes, bone marrow, and sometimes the skin and mucous membranes.[3] Occurrence of disseminated form of histoplasmosis especially cutaneous involvement in disseminated cases is rare in immunocompetent patients. In HIV-positive patients, 95% of histoplasmosis appears as disseminated infection.[4] The estimated incidence of cutaneous involvement varies widely, ranging from 3.2% in the United States to as high as 85% in Latin America.[5],[6] The dermatological manifestations reported in patients with disseminated histoplasmosis are extremely diverse and include papules and plaques with or without crusts, pustules and nodules, mucosal ulcers and erosions, molluscum contagiosum-like lesions, acneiform eruptions, keratotic plaques, peri-anal ulcers, erythema multiforme, and so on.[5],[6]
Isolated laryngeal histoplasmosis is also very rare, and there are only few case reports especially in immunocompromised patients.[7] It may present with dysphonia, odynophagia, dysphagia, dyspnea, fatigue, weight loss, and generalized unrest. Rathod et al. have described cutaneous lesions similar to ours in a post-renal transplant recipient patient. The patient had multiple tender erythematous papules and nodules on the face which were spontaneously ulcerating. There was no internal organ involvement.[8]
Sacoor has described a case of cutaneous histoplasmosis in the centrofacial region who later on developed laryngeal histoplasmosis; however, the patient was HIV-positive.[9] Besides this, there was involvement of liveras well.
Our patient had an unusual morphology in the form of erythematous edematous nontender plaques localized to the face that posed a diagnostic dilemma with other symmetrically distributed facial dermatoses. The presence of a mixed cell granuloma with the identification of characteristic histoplasma spores within macrophages and giant cells completely ruled out the other clinical differentials.
Infectious Disease Society of America has recommended itraconazole (200 mg three times for 3 days and then twice daily for at least 12 months) for mild-to-moderate disseminated histoplasmosis.
The case is being reported for its unusual cutaneous morphology along with probable laryngeal involvement.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Goswami RP, Pramanik N, Banerjee D, Raza MM, Guha SK, Maiti PK, et al. Histoplasmosis in Eastern India: The tip of the iceberg? Trans R Soc Trop Med Hyg 1999;93:540-2.
[Google Scholar]
|
| 2. |
Gopalakrishnan R, Nambi PS, Ramasubramanian V, Abdul Ghafur K, Parameswaran A. Histoplasmosis in India: Truly uncommon or uncommonly recognised? J Assoc Physicians India 2012;60:25-8.
[Google Scholar]
|
| 3. |
Raina RK, Mahajan V, Sood A, Saurabh S. Primary cutaneous histoplasmosis in an immunocompetent host from a nonendemic area. Indian J Dermatol 2016;61:467.
[Google Scholar]
|
| 4. |
Vidyanath S, Shameena P, Sudha S, Nair RG. Disseminated histoplasmosis with oral and cutaneous manifestations. J Oral Maxillofac Pathol 2013;17:139-42.
[Google Scholar]
|
| 5. |
Hong JH, Stetsenko GY, Pottinger PS, George E. Cutaneous presentation of disseminated histoplasmosis as a solitary peri-anal ulcer. Case report and discussion. J Cutan Pathol 2016;43:438-43.
[Google Scholar]
|
| 6. |
Cunha VS, Zampese MS, Aquino VR, Cestari TF, Goldani LZ. Mucocutaneous manifestations of disseminated histoplasmosis in patients with acquired immunodeficiency syndrome: Particular aspects in a Latin-American population. Clin Exp Dermatol 2007;32:250-5.
[Google Scholar]
|
| 7. |
Ferrari TC, Soares JM, Salles JM, Handam JS, Azevedo RC, Xavier MA, et al. Laryngeal histoplasmosis in an immunocompetent patient from a non-endemic region: Case report. Mycoses 2009;52:539-40.
[Google Scholar]
|
| 8. |
Rathod G, Goyal R, Bhimani RK, Aggarwal S, Patel R. Primary cutaneous histoplasmosis in 56 years old male. A rare case report. Int J Curr Microbiol Appl Sci 2014;3:420-6.
[Google Scholar]
|
| 9. |
Sacoor MF. Disseminated cutaneous histoplasmosis with laryngeal involvement in a setting of immune reconstitution inflammatory syndrome. South Afr J HIV Med 2017;18:693.
[Google Scholar]
|
Fulltext Views
2,956
PDF downloads
1,829





