Translate this page into:
A case of Heck's disease with primary intestinal lymphangiectasia treated with imiquimod
2 Department of Pathology, School of Medicine, Akdeniz University, Antalya, Turkey
Correspondence Address:
Erkan Alpsoy
Department of Dermatology and Venerology, School of Medicine, Akdeniz University, Konyaalti, Antalya 07070
Turkey
| How to cite this article: Bozca BC, Ozbudak IH, Alpsoy E. A case of Heck's disease with primary intestinal lymphangiectasia treated with imiquimod. Indian J Dermatol Venereol Leprol 2020;86:724-725 |
Sir,
Heck's disease, also known as focal or multifocal epithelial hyperplasia, is a rare benign lesion of the oral mucosa caused by human papilloma virus (HPV).1 The disease is characterized by the occurrence of multiple mucosal-colored, soft, flattened papules in the oral cavity, especially on the labial and buccal mucosa, lower lip and tongue, and less often on the upper lip, gingiva and palate.2 Intestinal lymphangiectasia is a rare disease characterized by abnormal and dilated intestinal lymphatic vessels, which causes a loss of protein and lymphocytes from the gut. Consequently, serum gammaglobulin levels, particularly IgG and IgA, and peripheral blood lymphocytes, particularly CD4+ T cells, decrease, resulting in prolonged functional immunodeficiency of the patient.3 Although the relationship of primary intestinal lymphangiectasia with the factors that may affect immunity, such as poverty, dietary insufficiency and close living conditions, has been previously implicated, its relationship with Heck's disease has not been reported before. Herein, we present a case of Heck's disease associated with primary intestinal lymphangiectasia successfully treated with imiquimod.
A 16-year-old female patient came with asymptomatic raised lesions in the mouth which was present since the age of 7, but increased after dental treatment in recent months. Clinical and routine laboratory findings (bilateral lower limb oedema, weight loss, lymphopenia, hypoalbuminemia), endoscopic examination and histopathology (ectasia of lymphatic vessels in the villi of the lamina propria) of the patient were consistent with the diagnosis of primary intestinal lymphangiectasia after the exclusion of other diseases that cause intestinal lymphangiectasia. The patient was under follow-up in pediatric gastroenterology. Family history revealed no similar oral lesions. Examination of oral mucosa revealed widespread papular lesions with cobblestone appearance localized in the buccal mucosa, dorsal aspect of the tongue and lips [Figure - 1]. Histopathological examination showed mild-severe dysplasia, koilocytotic atypia and viral cytopathic effect (koilocytosis, binucleation, parakeratosis and keratohyalin granules) [Figure - 2]. Polymerase chain reaction (PCR) analysis was performed, and HPV-16 and HPV-66 were identified. Based on these findings, the patient was diagnosed with Heck's disease. The patient was recommended the application of topical imiquimod 5% cream for 3 consecutive days/week. With this treatment, in the lips and buccal mucosa, an absolute improvement was achieved within 2 months [Figure - 3]. At the end of 5-month imiquimod treatment, there were only a few lesions limited to the dorsal aspect of the tongue. For these remaining lesions, imiquimod treatment was recommended 5 days/week for 1 month. With a total of 6 months of treatment, almost all lesions disappeared, and imiquimod treatment was discontinued. However, 18 months after discontinuation of treatment, new lesions started appearing on the anterior and lateral parts of the tongue, and imiquimod treatment was restarted. Lesions were controlled with the reintroduction of imiquimod treatment 5 days/week within 1 month. The patient is now in remission without treatment for mor than 1 year.
 |
| Figure 1: Lesions with cobblestone appearance in the inner labial mucosa |
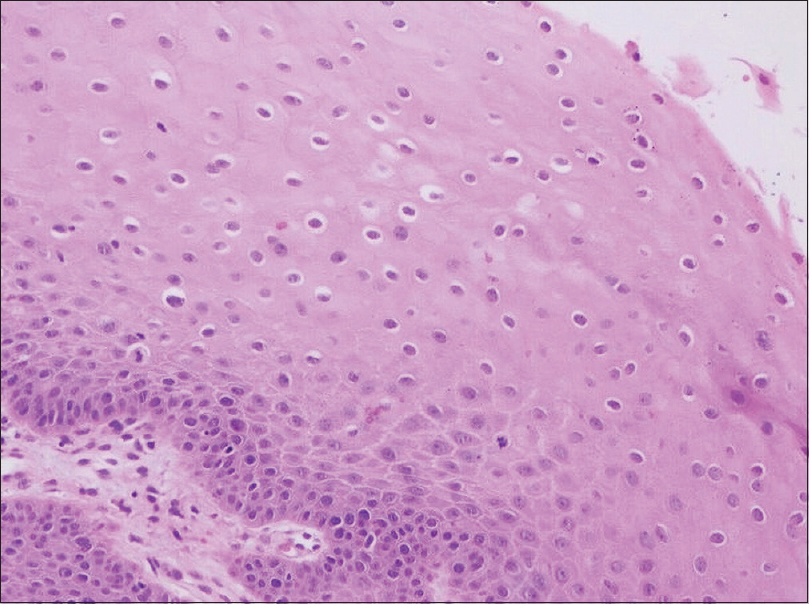 |
| Figure 2: Koilocytotic atypia (H and E, ×200) |
 |
| Figure 3: Improvement in lesions after 2 months of imiquimod application |
Naive CD4+ T cells (CD4+ CD45RA+), which play a central role in controlling HPV infections, decrease considerably in primary intestinal lymphangiectasia,[4] and this may explain the occurrence of extensive HPV-related Heck's disease. Primary intestinal lymphangectasia can suppress CD4+ T cell-mediated immunity, as in HIV infection, leading to the emergence of high-risk HPV subtypes, such as HPV 16 and 66. IgA plays an essential role in the immunity of mucosal surfaces. It can be speculated that the decrease in IgA levels due to loss from the gastrointestinal tract in intestinal lymphangiectasia may facilitate the development of HPV infection. However, the IgA level was within normal limits in our case, which supports, at least in this case, the critical role of CD4+ T cells. We were unable to find any previous reports of the association of primary intestinal lymphangiectasia and Heck's disease. This may be due to the extremely rare occurrence of both diseases. Another important reason may be the poor recognition of Heck's disease by nondermatologists. We believe that the case presented here may raise awareness on this issue and lead to similar observations in the future.
Imiquimod 5% cream has already proven its efficacy in the treatment of HPV infections by stimulation of both the innate immune response and the cell-mediated immune system.[5] There is no recommendation on the optimal frequency and duration of imiquimod treatment for Heck's disease. In a case reported by Barikbin et al.,[6] with the application of imiquimod for at least 8 h and to wash the area with water at the end of this period, once every other night, improvement started 4 weeks after beginning treatment. Based on the recommended regimen for the treatment of external genital warts and similar to the application of Barikbin et al.,[6] the patient was instructed to apply the cream on the oral lesions 3 days/week. During treatment, there were no local or systemic side effects other than mild irritation. Although there is no data related to the risk of systemic absorption due to the administration of imiquimod to the oral mucosa, we did not observe any systemic side effects in our case.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Ozden B, Gunduz K, Gunhan O, Ozden FO. A case report of focal epithelial hyperplasia (heck's disease) with pcr detection of human papillomavirus. J Maxillofac Oral Surg 2011;10:357-60.
[Google Scholar]
|
| 2. |
Said AK, Leao JC, Fedele S, Porter SR. Focal epithelial hyperplasia An update. J Oral Pathol Med 2013;42:435-42.
[Google Scholar]
|
| 3. |
Gumà J, Rubió J, Masip C, Alvaro T, Borràs JL. Aggressive bowel lymphoma in a patient with intestinal lymphangiectasia and widespread viral warts. Ann Oncol 1998;9:1355-6.
[Google Scholar]
|
| 4. |
Fuss IJ, Strober W, Cuccherini BA, Pearlstein GR, Bossuyt X, Brown M, et al. Intestinal lymphangiectasia, a disease characterized by selective loss of naive CD45RA+ lymphocytes into the gastrointestinal tract. Eur J Immunol 1998;28:4275-85.
[Google Scholar]
|
| 5. |
Ponte P, Serrão V, Fiadeiro T. Focal epithelial hyperplasia (Heck's Disease) in two siblings: Response to treatment with imiquimod 5% cream. Eur J Dermatol 2010;20:248-9.
[Google Scholar]
|
| 6. |
Barikbin B, Tehranchinia Z, Mozafari N. Treatment of multifocal epithelial hyperplasia with imiquimod. Indian J Dermatol Venereol Leprol. 2014;80(2):175-177.
[Google Scholar]
|
Fulltext Views
5,078
PDF downloads
2,117





