Translate this page into:
A case of linear immunoglobulin A disease with dapsone hypersensitivity and its management strategies
Correspondence Address:
Biju Vasudevan
Department of Dermatology, Command Hospital (Southern Command), Wanowrie, Pune - 411 040, Maharashtra
India
| How to cite this article: Verma R, Vasudevan B, Sagar A, Pragasam V, Deb P, Choden G. A case of linear immunoglobulin A disease with dapsone hypersensitivity and its management strategies. Indian J Dermatol Venereol Leprol 2013;79:833-835 |
Sir,
Linear immunoglobulin A (IgA) disease is a rare acquired autoimmune subepidermal vesiculobullous disorder with an estimated prevalence of 0.5 per 1,000,000 adults. [1] Drugs and infections have been reported to be associated. [2] We herein report a patient of severe linear IgA disease with unusual therapeutic challenges.
A 27-year-old lady presented with fever of 7 days duration, followed 2 days later by multiple painful fluid-filled lesions over body. Dermatological examination revealed multiple polysized, discrete to confluent crusted plaques with vesicles along margins in generalized distribution (cluster of jewel appearance) [Figure - 1]. Multiple hypopigmented macules and pustules were also present. Bulla spread and Nikolsky′s signs were negative. There was no mucosal involvement. Clinical differential diagnosis of subcorneal pustular dermatosis, linear IgA disease, and bullous pemphigoid was offered.
 |
| Figure 1: Annular skin lesions with vesicles on margins giving a cluster of jewels appearance |
Initial skin biopsy revealed subepidermal bulla with a neutrophilic infiltrate in the dermis [Figure - 2]. Direct immunofluorescence showed deposition of IgA linearly along basement membrane. Patient was diagnosed as a case of linear IgA disease and was started on oral dapsone 100 mg once daily. The lesions showed gradual resolution over 4 weeks.
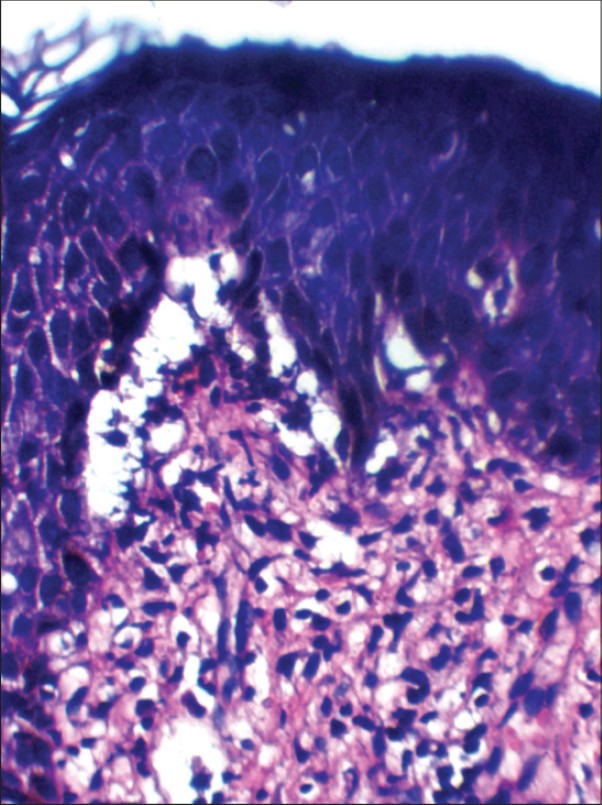 |
| Figure 2: Histopathology revealing classical subepidermal bulla with neutrophilic infiltrate. ×40 (H and E, ×40) |
However after 4 weeks, patient reported back with fever and extensive redness and scaling over body. On examination, patient was febrile, had icterus, and an extensive erythematous maculopapular rash. Investigations revealed serum bilirubin of 3.3 mg/dL, alanine aminotransferase levels of 162 IU/L, and aspartate aminotransferase levels of 92 IU/L with absolute eosinophil count of 1383 cells/cm. Ultrasound abdomen revealed hepatosplenomegaly. Patient was diagnosed to have dapsone-induced hypersensitivity syndrome and dapsone was stopped. Patient was started on oral prednisolone 60 mg and colchicine 0.5 mg thrice daily.
In spite of this therapy, after 7 days, the bullous lesions relapsed and serum bilirubin levels began to rise. With two different problems of linear IgA dermatosis and dapsone hypersensitivity syndrome, intravenous pulse methylprednisolone 1 g for 3 consecutive days was administered. The patient started improving on the 2 nd day of pulse therapy. She was restarted on oral prednisolone 60 mg after completion of the pulse therapy and colchicine was continued.
Two weeks later, patient developed multiple furuncles over the extremities. There was no evidence of any immunosuppression in the form of diabetes, human immunodeficiency virus infection, or any other associated disorders. The patient was started on oral linezolid 600 mg twice daily, prednisolone was tapered by 10 mg every 2 weeks, and colchicine was continued. The furuncles regressed in duration of one week. When tapering of oral prednisolone had reached 20 mg after 4 weeks, patient again started developing multiple fluid-filled lesions over extremities similar to the initial episode. Repeat skin biopsy and direct immunofluorescence showed typical features of linear IgA dermatoses and patient was restarted on full dose of prednisolone 60 mg and colchicine was stopped. The skin lesions gradually started resolving and liver function tests also became normal after 8 weeks. The steroids were continued with progressively tapering doses for a total duration of further 12 weeks after which all the skin lesions resolved, not leaving any trace of pigmentation or scars. The patient has presently been followed-up for 6 months during which she has had no recurrence.
The clinical presentation of linear IgA disease can be heterogeneous and can mimic other blistering diseases such as dermatitis herpetiformis, bullous pemphigoid, pemphigus vulgaris, epidermolysis bullosa acquisita, and also other groups of disorders like erythema multiforme, toxic epidermal necrolysis, systemic lupus erythematosus, and erythema annulare centrifugum. [3] Linear IgA disease is a chronic relapsing condition with mild cutaneous manifestations usually. Our patient had very severe cutaneous involvement without mucosal involvement which is not seen very commonly.
Dapsone is the most effective drug in managing this condition with excellent initial responses and long-term remissions being reported. [4] Colchicine, thalidomide, cyclosporine, niacinamide, antibiotics like sulfonamides and amoxicillin are also reported to be effective. [5] Oral steroids have been combined with dapsone for better results in recalcitrant cases. However, use of pulsed steroids in heavy intravenous doses has not been described previously. Dapsone hypersensitivity syndrome being concomitantly managed with severe linear IgA disease is another therapeutic challenge not faced very often.
Herein, we had a patient of severe cutaneous linear IgA disease who had various therapeutic challenges in the form of dapsone hypersensitivity syndrome and nonresponse to colchicine. She was in the reproductive age group and hence thalidomide was contraindicated. Corticosteroids seemed to be the only panacea whenever she got into trouble and even pulsed steroids had to be given. Such unusual therapeutic requirements in a case of linear IgA disease have rarely been mentioned in literature.
| 1. |
Zillikens D, Wever S, Roth A, Weidenthaler-Barth B, Hashimoto T, Brocker EB. Incidence of autoimmune subepidermal blistering dermatoses in a region of central Germany. Arch Dermatol 1995;131:957-8.
[Google Scholar]
|
| 2. |
Jheng-Wei L, Yi-Chin S, Wen-Hung C. Vancomycin-induced linear IgA bullous dermatosis mimicking toxic epidermal necrolysis. Indian J Dermatol Venereol Leprol 2011;77:537.
[Google Scholar]
|
| 3. |
Dippel E, Orfanos CE, Zouboulis C. Linear IgA dermatosis presenting with erythema annulare centrifugum lesions: Report of three cases in adults. J Eur Acad Dermatol Venereol 2001;15:167-70.
[Google Scholar]
|
| 4. |
Alajlan A, Al-Khawajah M, Al-Sheikh O, Al-Saif F, Al-Rasheed S, Al-Hoqail I, et al. Treatment of linear IgA bullous dermatosis of childhood with flucloxacillin. J Am Acad Dermatol 2006;54:652-6.
[Google Scholar]
|
| 5. |
Madnani NA, Khan KJ. Linear IgA bullous dermatosis of childhood: Response to thalidomide. Indian J Dermatol Venereol Leprol 2010;76:427-9.
[Google Scholar]
|
Fulltext Views
2,807
PDF downloads
1,788





