Translate this page into:
A case of malignant syphilis complicated with myiasis in Northeast China
2 Department of Dermatology, FAW General Hospital, Changchun, China
Correspondence Address:
Yong-Zhi Ji
Department of Dermatology, Second Hospital of Jilin University, 218 Ziqiang Street, Changchun 130041
China
| How to cite this article: Ji YZ, Jia LL, Li Y. A case of malignant syphilis complicated with myiasis in Northeast China. Indian J Dermatol Venereol Leprol 2020;86:470 |
Sir,
Malignant syphilis is a rare form of secondary syphilis, which is most commonly associated with HIV infection. We report a 55-year-old man who presented with a 2-week history of cutaneous ulcers and thick crusts accompanied by low-grade fever (37.5°C–38.7°C). He worked in unhygienic surroundings and the standard of living was low. He had divorced his wife 10 years ago and gave history of unprotected sexual contact 2 months back with a partner who could not be traced. He was also consuming alcohol heavily since 10 years. Physical examination revealed multiple ulcers covered with rupioid crusts (maximum diameter of 6 cm) on the face, scalp, trunk and extremities, including the soles [Figure - 1]a and [Figure - 1]b. The mucosa was clear and there was no superficial lymph node enlargement. During surgical debridement, several white maggots (about 1 cm in length) were identified from the necrotic tissue on the left lower leg [Figure - 1]c. Laboratory examination revealed leucocytosis (13.0 × 109/L) with neutrophilia (10.23 × 109/L) and slightly increased C-reactive protein (10.4 mg/dL). Liver function tests were normal with alanine aminotransferase level of 36 U/L (normal value <40 U/L) and aspartate aminotransferase level of 37 U/L (normal value <40 U/L). Serum treponema pallidum particle agglutination assay was positive and rapid plasma reagin (RPR) titer was 1:128. HIV serological test was negative. The tissue was from the region of cutaneous ulcers. Tissue cultures for fungi, Mycobacterium tuberculosis and Neisseria gonorrhoeae were negative. Dark ground microscopic examination for Treponema pallidum w as negative. Histological examination of a skin biopsy specimen from the lesions on the back revealed epidermal hyperplasia and extensive inflammatory infiltration with plasma cells and lymphocytes in the dermis [Figure - 2]. The maggots were identified as the second instar larvae of hypoderma lineatum by the Department of Parasitology of Jilin University. Based on the above findings, the patient was diagnosed with malignant syphilis and myiasis after ruling out fungal infections, Mycobacterium tuberculosis or Neisseria gonorrhoeae disseminated infections and vasculitis. Treatment was started with intramuscular penicillin G benzathine (2.4 million units per week for 3 weeks) preceded by 20 mg oral prednisone to prevent Jarisch–Herxheimer reaction. One month later, the ulcers healed completely, although atrophic scars remained [Figure - 1]d and [Figure - 1]e; the RPR titer dropped to 1:32. At 3-month follow-up, there was no relapse and the RPR titer had further dropped to 1:4; anti-HIV antibody was still negative.
 |
| Figure 1: |
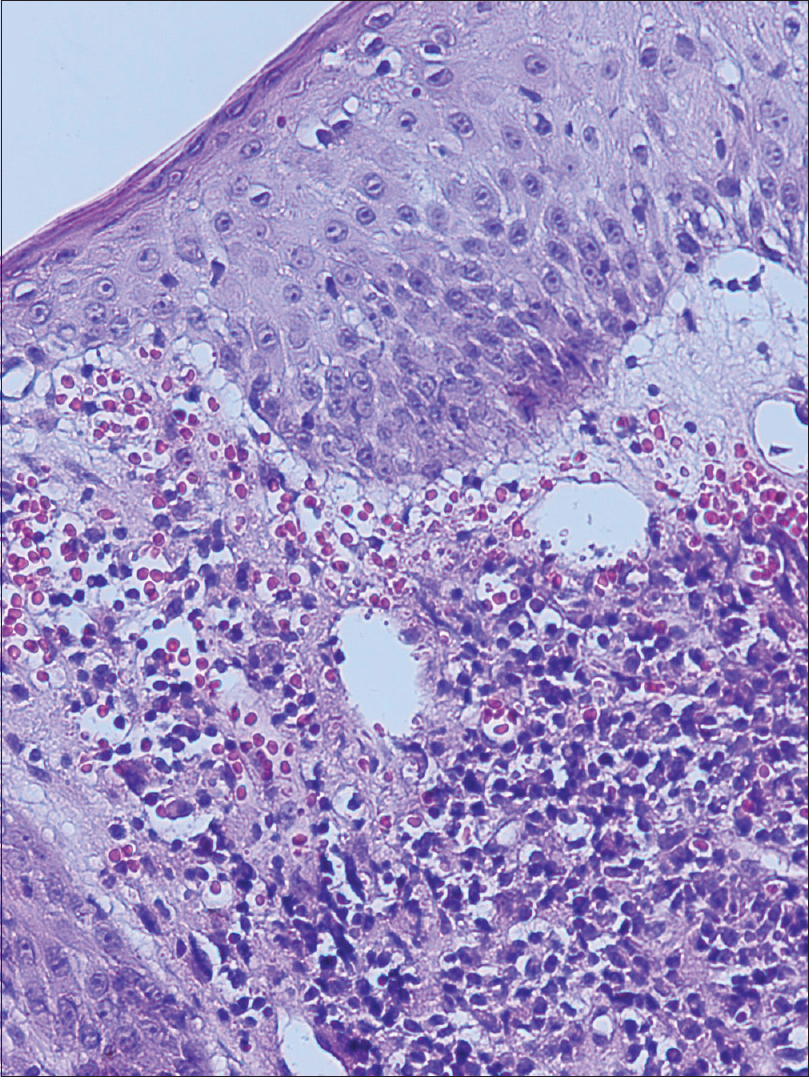 |
| Figure 2: Histopathological examination showing epidermal hyperplasia and dense inflammatory infiltration of plasma cells and lymphocytes in the dermis (H and E, ×200) |
Malignant syphilis is clinically characterized by generalized necrotic ulcers covered with dark, rupioid crusts which are preceded by prodromal symptoms of fever, headache and myalgia. The development of malignant syphilis has been linked to the weakening of the host immune status. It is believed that HIV-induced immunodeficiency favors the predominance of the agent in the agent-host contest which may alter the classical clinical course of syphilis and produce unusual syphilitic manifestations.[1] However, malignant syphilis is not exclusive to HIV-positive patients and is also associated with chronic alcoholism, malnutrition, hepatitis, pregnancy, diabetes, repeated infections and fatal blow.[2] In our case, the probable triggers were excessive alcohol consumption and malnutrition. Poor personal hygiene and impaired skin barrier caused by malignant syphilis also led to myiasis, which is a rare parasitic disease in the non-pastoral areas, especially in North-east China. The diagnosis of malignant syphilis is based on the clinical manifestations, serological findings and histopathological findings of lymphocytic infiltrates among plasma cells in the dermis. It is worth mentioning that syphilis serology can be negative in HIV-positive patients,[3] or due to the so-called syphilis prozone phenomenon.[4] Furthermore, the titer of non-treponemal test antigen is not directly related to the severity and duration of the disease.[5] Neurosyphilis can be seen in malignant syphilis; however, in our patient, there were no symptoms or signs suggestive of neurological involvement and the treatment resulted in satisfactory reduction in RPR titer. Hence, cerebrospinal fluid assessment was not performed. The treatment schedule for malignant syphilis is the same as for late latent syphilis.[2] Ceftriaxone or tetracyclines can be used in patients who are allergic to penicillin. Usually, malignant syphilis rapidly responds to appropriate therapy; however, in the absence of treatment, the infection can progress to late stages with poorer prognosis. Thus, awareness regarding the clinicopathological manifestations is necessary for the diagnosis of this rare disease and its presence should alert the health care provider to consider HIV co-infection and other potential causes for immune dysfunction.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Corti M, Solari R, De Carolis L, Figueiras O, Vittar N, Maronna E, et al. Malignant syphilis in a patient infected by human immunodeficiency virus. Case report and literature review. Rev Chilena Infectol 2012;29:678-81.
[Google Scholar]
|
| 2. |
García-Martínez FJ, Fernandez-Redondo V, Sanchez-Aguilar D, Toribio J. Malignant syphilis in an immunocompetent patient. Actas Dermosifiliogr 2012;103:437-9.
[Google Scholar]
|
| 3. |
Farhi D, Benhaddou N, Grange P, Zizi N, Deleuze J, Morini JP, et al. Clinical and serologic baseline and follow-up features of syphilis according to HIV status in the post-HAART era. Medicine (Baltimore) 2009;88:331-40.
[Google Scholar]
|
| 4. |
Watson KM, White JM, Salisbury JR, Creamer D. Lues maligna. Clin Exp Dermatol 2004;29:625-7.
[Google Scholar]
|
| 5. |
Yamashita M, Fujii Y, Ozaki K, Urano Y, Iwasa M, Nakamura S, et al. Human immunodeficiency virus-positive secondary syphilis mimicking cutaneous T-cell lymphoma. Diagn Pathol 2015;10:185.
[Google Scholar]
|
Fulltext Views
4,840
PDF downloads
3,213





