Translate this page into:
A case of multidrug-resistant tuberculosis presenting as erythema elevatum diutinum: A rare association
Corresponding author: Dr. Preema Sinha, Department of Dermatology, Base Hospital, Lucknow 226002, Uttar Pradesh, India. sinhapreema@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sinha P, Sharma J, Tiwari S, Bhattacharjee S, Sinha A. A case of multidrug-resistant tuberculosis presenting as erythema elevatum diutinum: A rare association. Indian J Dermatol Venereol Leprol 2022;88:548-50.
Sir,
Erythema elevatum diutinum was described by Hutchinson in 1888 and Bury in 1889 and was named by Crocker and Williams in 1894.1,2 It is classified amongst the cutaneous vasculitides and is often associated with underlying infectious, autoimmune or neoplastic conditions. There are occasional reports of lung involvement in the form of pulmonary infiltrates, tuberculosis and Wegener’s granulomatosis.1-4 It is characterized histologically by leucocytoclastic vasculitis with fibrosis and a predominately neutrophilic dermal infiltrate. We report a case of erythema elevatum diutinum as the presenting feature in a patient with multidrug-resistant tuberculosis.
A 39-year-old woman presented with multiple erythematous tender plaques over the extensor surfaces of both upper and lower limbs since ten days. She also complained of arthralgia of the wrists and knees. There was a family history of multidrug-resistant pulmonary tuberculosis.
The general and systemic examination were normal. There was no joint deformity, tenderness or swelling. Multiple well-defined, erythematous papules and plaques were seen over the extensor surface of wrists and dorsae of hands and knees [Figures 1 and 2]. There was no mucosal involvement.

- Multiple well-defined, erythematous papules and plaques present over the extensor surface of forearms and dorsae of both hands

- Multiple well-defined, bilaterally symmetrical erythematous papules and plaques present over the knees
Laboratory investigations showed a normal hemogram and serum biochemistry but erythrocyte sedimentation rate was 50 mm at the end of one hour and the C-reactive protein was positive. Anti-nuclear antibodies and rheumatoid factor were not detected and complement levels (C3 and C4) were normal. Serological tests for human immunodeficiency virus and syphilis were non-reactive. Histopathological examination of the plaque revealed exocytosis of inflammatory cells in the epidermis and an intense perivascular neutrophilic infiltrate with leukocytoclasia in the dermis [Figures 3 and 4].
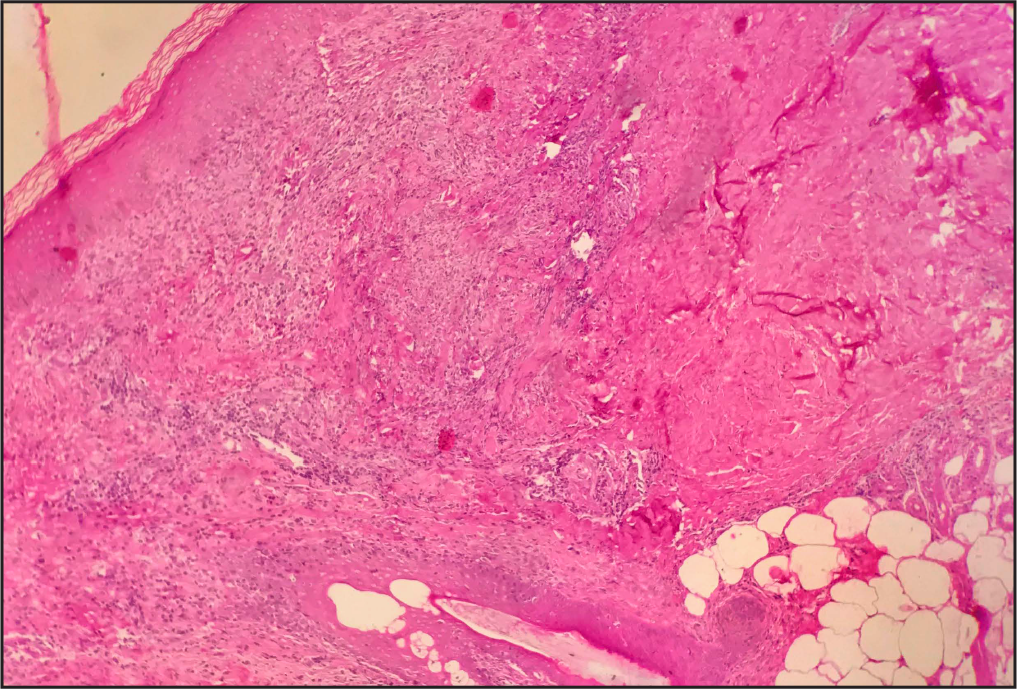
- (H & E ×100) Dermis shows dense perivascular neutrophilic infiltrate with leukocytoclasis not extending to the subcutaneous fat
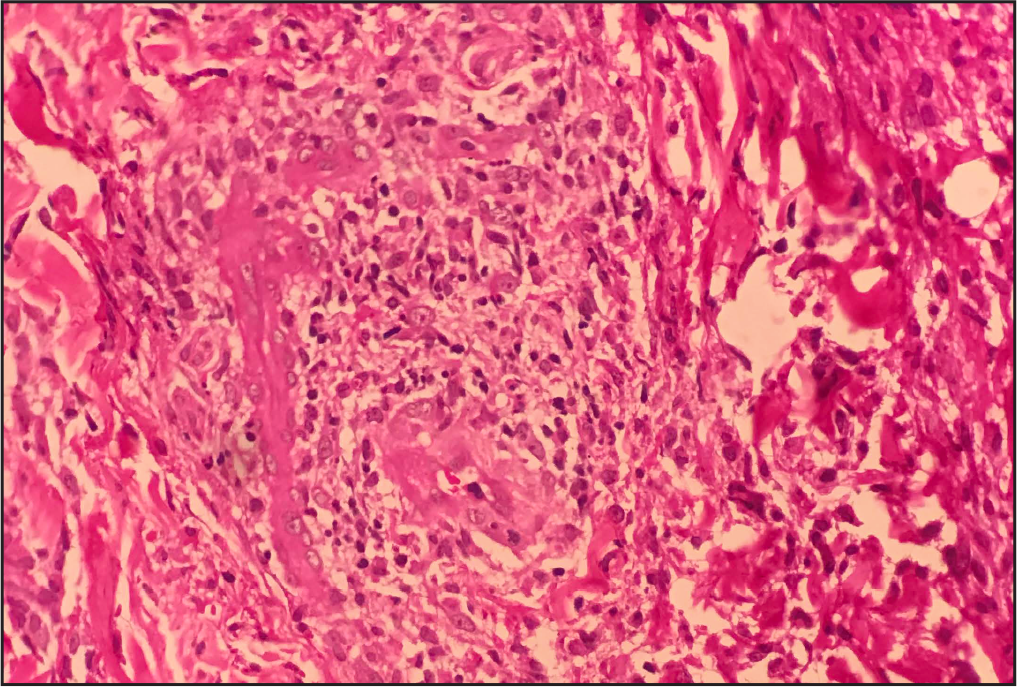
- (H & E ×400) Dense perivascular neutrophilic infiltrate with leukocytoclasis
An evaluation for tuberculosis was performed. The quantiferon gold test was positive and a computed tomography scan of the chest showed active bronchiolitis in left lower lobe with hilar and mediastinal lymphadenopathy [Figure 5]. The XpertMTB/ Rif assay done on mediastinal lymph node aspirate obtained through endobronchial ultrasound transbronchial needle aspirate identified Mycobacterium tuberculosis resistant to rifampicin. A cytological study of bronchoalveolar lavage fluid did not reveal malignant cells.
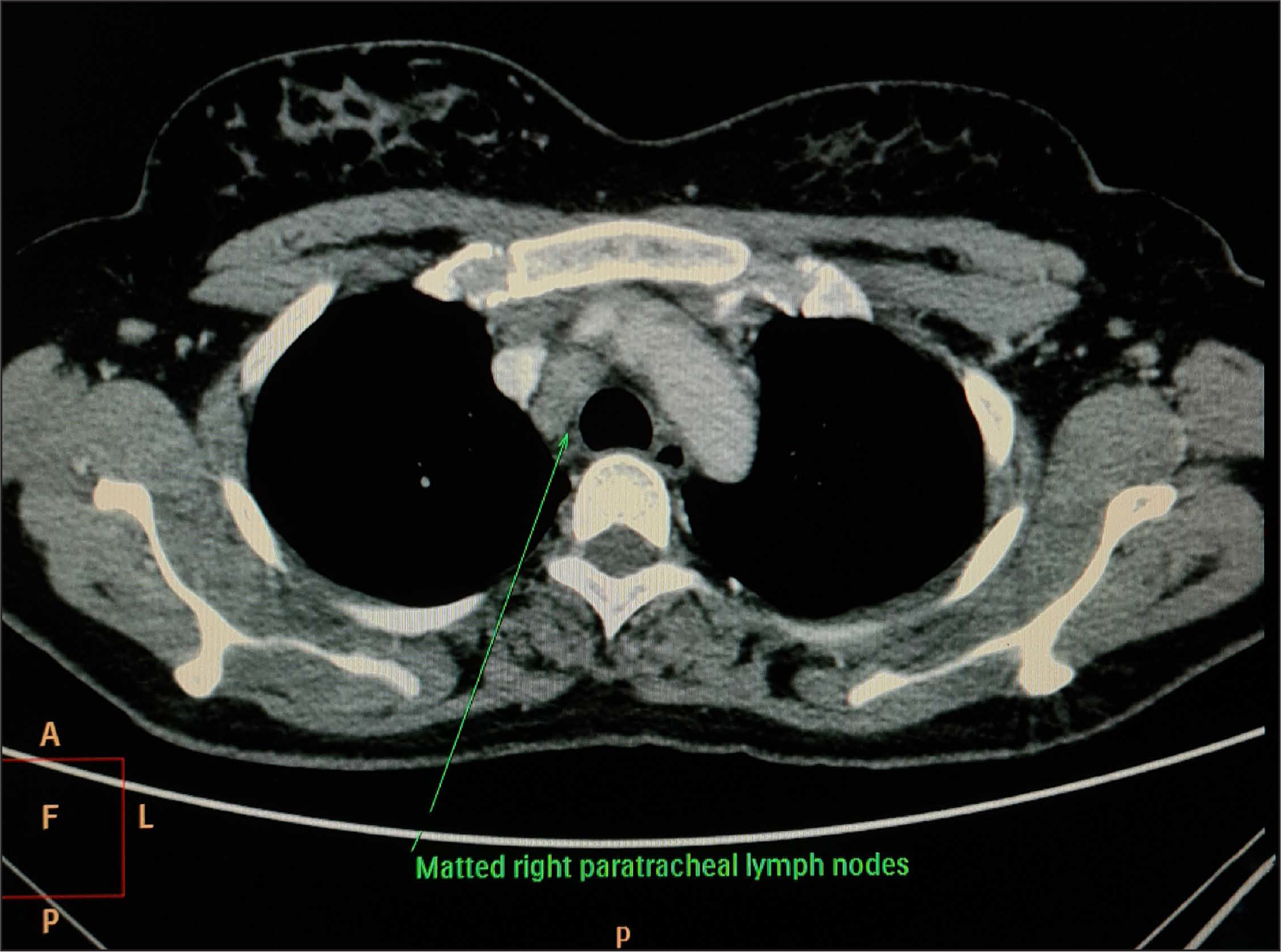
- Computed tomography scan of the chest showing mediastinal lymphadenopathy
In view of these findings, a diagnosis of multidrug-resistant tuberculosis with erythema elevatum diutinum was made. Treatment for drug-resistant pulmonary tuberculosis was instituted by a pulmonologist and the erythema elevatum diutinum was treated with dapsone 100 mg daily resulting in complete regression of skin lesions in just seven days. Dapsone was however continued for a total of eight weeks as the patient had one episode of recurrence of skin lesions.
Erythema elevatum diutinum is a chronic cutaneous small-vessel vasculitis presenting as reddish-brown papules, plaques or nodules with a predilection for the extensor surfaces of the extremities, especially the joints. Occasionally, vesicles, haemorrhagic lesions and ulcerations have also been described.5 Lesions may be tender and arthralgia and systemic symptoms are sometimes present.
Erythema elevatum diutinum is an immune complex-mediated type III hypersensitivity reaction. The leukocytoclastic vasculitis may be initiated by immune complex deposition in the post-capillary venules activating the complement cascade and neutrophilic chemotaxis.6,7 This has been proposed to be due to an Arthus type reaction to viral or bacterial antigens.
In conclusion, we report a case of erythema elevatum diutinum in a patient with multidrug-resistant tuberculosis. Our case underscores the importance of working up all patients with erythema elevatum diutinum exhaustively for underlying disease.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- A case of erythema with remarkable nodular thickening and induration of skin associated with intermittent albuminuria. Illus Med News. 1889;3:145.:9.
- [CrossRef] [PubMed] [Google Scholar]
- Erythema elevatum diutinum associated with pulmonary infiltrates. Br J Dermatol. 1997;137:652.:3.
- [CrossRef] [PubMed] [Google Scholar]
- Erythema elevatum diutinum associated with Wegener’s granulomatosis and IgA paraproteinemia. J Am Acad Dermatol. 1993;28:846.:9.
- [CrossRef] [PubMed] [Google Scholar]
- Erythematous nodules in a patient infected with the human immunodeficiency virus: erythema elevatum diutinum. Arch Dermatol. 1998;134:231.:6.
- [CrossRef] [PubMed] [Google Scholar]
- Erythema elevatum diutinum: a case report and review of literature. Int J Dermatol. 2019;58:408.:15.
- [CrossRef] [PubMed] [Google Scholar]





