Translate this page into:
A case of neutrophilic dermatosis of the hands associated with chronic myelomonocytic leukemia presenting as annular papules and plaques
Corresponding author: Prof. Jun Young Kim, Department of Dermatology, Kyungpook National University Hospital, South Korea. 198kjy@hanmail.net
-
Received: ,
Accepted: ,
How to cite this article: Ha NG, Han MH, Park TI, Lee SJ, Kim JY. A case of neutrophilic dermatosis of the hands associated with chronic myelomonocytic leukemia presenting as annular papules and plaques. Indian J Dermatol Venereol Leprol. 2024;90:640-2. doi: 10.25259/IJDVL_75_2022
Dear Editor,
A 72-year-old female presented with several, relatively hard, asymptomatic papules and annular plaques on both hands, which had been present since the past two months [Figure 1]. Some lesions showed vesiculobullous changes and crusts at the center [Figure 1]. The patient had taken oral steroids prescribed by a local medical center for three weeks, but the medication had no effect on these lesions. Additionally, the patient had a liver abscess and was taking medication for hypothyroidism. She also complained of experiencing shortness of breath recently while walking. With clinical differential diagnoses of granuloma annulare, erythema annulare centrifugum, neutrophilic dermatosis of the dorsal hands (NDDH), and erythema elevatum diutinum, a punch biopsy was obtained from the lesion on her right index finger [Figure 1, yellow arrow]. Histopathological examination revealed heavy infiltration of neutrophils, histiocytes, extravasated red blood cells, and nuclear fragments, without vasculitis in the dermis [Figures 2a and 2b]. Immunohistochemical staining for acid-fast bacilli and Grocott’s methenamine silver to rule out cutaneous infections was negative. Finally, the patient was diagnosed with NDDH because the cutaneous lesions were mainly distributed on the dorsal hands, and pathologic findings showed a dense infiltration of neutrophils without palisading granuloma or leukocytoclastic vasculitis. Since this is a type of Sweet syndrome, laboratory investigations were conducted to determine the association with systemic diseases, revealing a white blood cell count of 30,000/µL with 74.6% neutrophils and 12.9% monocytes, a platelet count of 63,000/µL, and a hemoglobin level of 6.3 g/dL. Due to leukocytosis and anemia, the patient was referred to a hematologist, and a bone marrow biopsy confirmed chronic myelomonocytic leukemia (CMML). The patient received azacitidine chemotherapy for the underlying CMML, and her skin lesions were treated with topical antibiotic and betamethasone dipropionate 0.064% cream. The lesions improved under chemotherapy and deteriorated between treatments, showing a waxing and waning pattern. After undergoing chemotherapy, the skin lesions remained in remission for seven months.
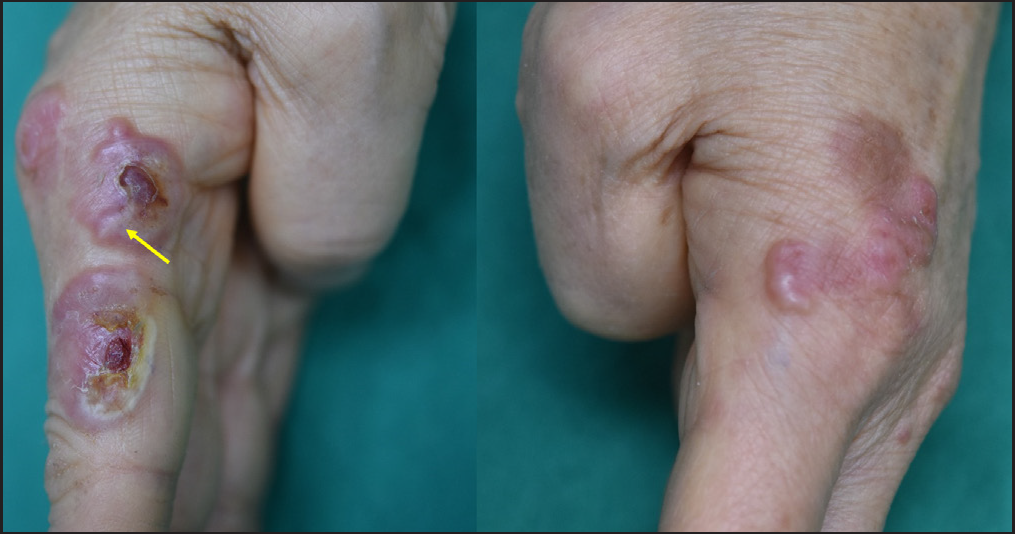
- Erythematous annular papules and plaques with a symmetrical distribution on both hands. Some lesions show vesiculobullous change and crusts at the center. A punch biopsy was taken from the lesion on her right index finger (yellow arrow).
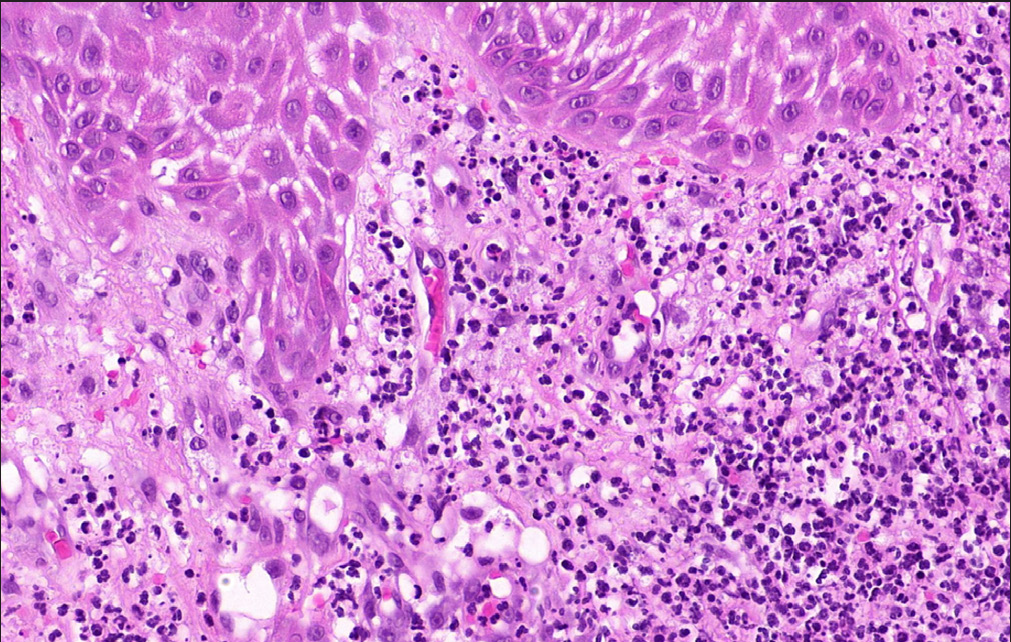
- The infiltrated cells in the dermis are mainly composed of neutrophils. In the upper dermis, extravasated red blood cells and nuclear dust can be observed (H&E, ×200).
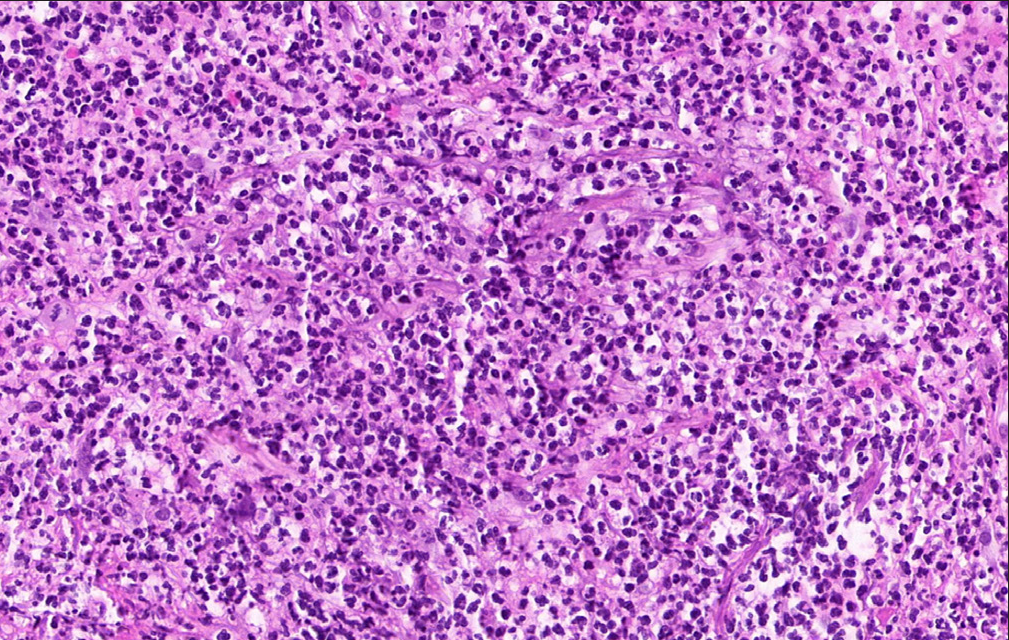
- Heavy infiltration of neutrophils in the mid-dermis (H&E, ×200).
NDDH is a rare localized variant of Sweet syndrome, characterized by painful erythematous violaceous papules, plaques, and nodules with bullae, pustules, and ulcers. 1 The majority of NDDH cases involve the dorsal aspect of the hand, but some also involve the lateral and palmar aspects of the hand. 2 Weenig et al. 1 reported four cases of neutrophilic dermatosis affecting the hands with ulceration, pustules, and/or edematous changes. Walling et al. 3 reported a series of nine patients with NDDH, mainly presenting with ulcerated plaques. Micallef et al. 4 reported four cases of NDDH with violaceous plaques, ulcerations, pustules, and/or bullae. The cutaneous manifestation of NDDH is similar to that of atypical pyoderma gangrenosum and bullous Sweet syndrome. 4 Although, Duquia et al. 5 reported a case of NDDH with an annular configuration, it had an edematous border with vesiculobullous changes. In this case, the patient presented with atypical indurated papules and annular plaques with vesiculobullous changes that mainly involved the dorsal hands, which clinically suggested granuloma annulare or erythema elevatum diutinum as a differential diagnosis. However, histopathologic features of dense neutrophil infiltration without palisading granulomatous inflammation or leukocytoclastic vasculitis allowed us to distinguish it from them. Table 1 lists the clinicopathologic features of 18 cases of NDDH in the recent literature, including the present case.
| Case | Age (years) | Sex | Related illness | Clinical description | Histologic description or diagnosis | Reference |
|---|---|---|---|---|---|---|
| 1 | 68 | M | Pulmonary squamous cell carcinoma | Red to violaceous, edematous plaques | Diffuse dermal neutrophilia | Weenig et al., 1 cases 1–4 |
| 2 | 77 | M | Laryngeal squamous cell carcinoma, IgA monoclonal gammopathy | 6 × 8 cm ulcer with an erythematous, edematous borderand a yellow adherent exudate at the base | Papillary dermal edema and diffuse dermal neutrophilia | |
| 3 | 62 | F | Preleukemia | Erythematous, edematous plaques with centralnecrosis and a violaceous border | Papillary dermal edema and diffuse dermal neutrophilia | |
| 4 | 75 | M | None identified | Several pustules superimposed on erythematousplaques | Papillary dermal edema and diffuse dermal neutrophilia | |
| 5 | 61 | F | Moderate leukocytosis, neutrophilia, anemia, elevated inflammatory indices | 6 × 4 cm violaceous plaque with central nonundermining superficial ulceration | Pseudoepitheliomatous hyperplasia, vasculitis, dense polymorphonuclear infiltrate epidermis to subcutis | Walling et al., 3 cases 5–13 |
| 6 | 44 | F | None identified | Recurrent ulcerations | Ulceration, no vasculitis, dense dermal neutrophilic infiltrate with lymphocytes | |
| 7 | 48 | F | Leukocytosis, neutrophilia | Small, edematous, pink papules evolving into pustules with subsequent ulceration | Ulceration, edema, sheets of polymorphonuclear cell in dermis, no vasculitis | |
| 8 | 71 | M | Metastatic lung cancer | Superficial ulcerations with raised violaceous nonundermined borders | Spongiosis, compact parakeratosis, and a dense upper dermal neutrophilic infiltrate | |
| 9 | 30 | F | Elevated inflammatory indices, leukocytosis | 4 × 4 cm violaceous, firm, centrally necrotic plaque | Ulceration, sheets of polymorphonuclear cell in dermis,no vasculitis | |
| 10 | 69 | F | B cell lymphoma | 2 cm ulceration with a violaceous border | Ulceration, sheets of polymorphonuclear cell in dermis, no vasculitis | |
| 11 | 71 | F | None identified | Violaceous 3 to 4 cm plaques | Subepidermal edema and microabscess, dense interstitial and perivascular neutrophilic infiltrate, no vasculitis | |
| 12 | 31 | M | Leukocytosis, neutrophilic, elevated liver enzymes | Spontaneously arising bullae expanded into tender ulcers | Florid, fibrinoid necrosis, folliculocentric neutrophilic infiltrate in papillary/reticular dermis | |
| 13 | 51 | F | Elevated C-reactive protein, leukocytosis, neutrophilia, anemia | Superficially ulcerated plaque with violaceous undermined borders | Dense neutrophilic infiltrate subepidermal to subcutis, no vasculitis | |
| 14 | 60 | F | None detected | Tender violaceous plaque | Focally ulcerated, markedly acanthotic epidermis, dense neutrophilic infiltrate in the upper dermis, polymorphonuclear infiltrate in the epidermis | Micallef et al., 4 cases 14–17 |
| 15 | 82 | F | None detected | Violaceous plaques with a pustular border | Dense neutrophilic infiltrate from the epidermis into the deep reticular dermis. Microabscess formation in the epidermis. | |
| 16 | 73 | F | None detected | Violaceous plaques with an ulcerated center | Neutrophilic infiltration of the epidermis with multiple epidermal microabscesses | |
| 17 | 78 | M | Respiratory tract infection | Violaceous bullae with ulceration | Dense neutrophilic infiltrate from the epidermis to the subcutaneous tissue with abscess formation | |
| 18 | 72 | F | Chronic myelomonocytic leukemia | Annular indurated papules and plaques with vesicular change and crust on the center | Dense infiltration of neutrophils and histiocytes, extravasated red blood cells, nuclear fragments, no vasculitis | Current case |
M: male, F: female
NDDH is associated with various conditions, including malignancies, inflammatory bowel diseases, and rheumatologic diseases. 2 In particular, hematologic disorders, such as myelodysplastic syndrome, plasma cell dyscrasias, and acute myeloid leukemia, account for 14.3% of cases. 4 This case is rare because NDDH is accompanied by CMML, a type of myelodysplastic/myeloproliferative neoplasm overlap syndrome. In this case, due to the diagnosis of NDDH and shortness of breath, the patient underwent a blood test including a complete blood count, which led to the detection of the underlying haematologic malignancy, CMML. In cases of NDDH, it is important to note that cutaneous findings may precede the identification of an underlying malignancy. 1 Once NDDH is diagnosed, an appropriate workup to exclude associated diseases should be performed. A complete blood count with cytopenia may suggest haematologic disorders. Gastrointestinal symptoms raise the suspicion of inflammatory bowel disease. Here, we report a case of NDDH accompanied by CMML with an atypical cutaneous presentation in the form of indurated papules and annular plaques. This case may help to better understand NDDH and further expand the clinical spectrum of skin lesion morphologies in NDDH.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Neutrophilic dermatosis of the hands: Four new cases and review of the literature. Int J Dermatology. 2004;43:95-102.
- [Google Scholar]
- Acral manifestations of Sweet syndrome (neutrophilic dermatosis of the hands) Clin Dermatol. 2017;35:81-4.
- [CrossRef] [PubMed] [Google Scholar]
- The relationship between neutrophilic dermatosis of the dorsal hands and sweet syndrome: Report of 9 cases and comparison to atypical pyoderma gangrenosum. Arch Dermatol. 2006;142:57-63.
- [CrossRef] [PubMed] [Google Scholar]
- Neutrophilic dermatosis of the dorsal hands: A review of 123 cases. J Am Acad Dermatol 2019 S0190-9622(19)32678-7
- [Google Scholar]
- Neutrophilic dermatosis of the dorsal of the hands: Acral sweet syndrome? Int J Dermatol. 2006;45:51-2.
- [CrossRef] [PubMed] [Google Scholar]






