Translate this page into:
A case of the novel mutation p.L311P in KRT5 causing localised epidermolysis bullosa simplex in East Asian population
Corresponding author: Prof. Chul Hwan Bang, Department of Dermatology, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea. mrbangga@catholic.ac.kr
-
Received: ,
Accepted: ,
How to cite this article: Yun SY, Kim YH, Han JH, Kim M, Lee JH, Park YM, et al. A case of the novel mutation p.L311P in KRT5 causing localised epidermolysis bullosa simplex in East Asian population. Indian J Dermatol Venereol Leprol. 2024;90:798-800. doi: 10.25259/IJDVL_241_2023
Dear Editor,
Epidermolysis bullosa (EB) is an inherited condition distinguished by the development of blisters upon minor trauma. The classification of EB into four main types is based on the extent of ultramicroscopic separation occurring within the skin.1 Among these, EB simplex (EBS) is typified by blister formation within the basal epidermis, largely following an autosomal dominant inheritance pattern.1 Localised EBS is the most common type of EBS. Although mutations in several genes, including PKP1, TGM5, PLEC, JUP, DST, KRT5, KRT14, DSP, and EXPH5, are associated with the EBS phenotype, more than 75% of EBS patients have shown mutations in the KRT5 or KRT14 gene.2 Herein, we report a case of localised EBS with vesicles and bullae restricted to the soles of the feet with a novel mutation in the KRT5 gene.
A 19-year-old man, presented with multiple, painful, variably-sized bullae on the soles of both feet since childhood [Figures 1a and 1b]. He gave a history of trauma-induced bullae on the soles due to the constant rubbing of his shoes during movement. Mucosae and nails were not affected. In addition, his maternal grandmother, mother, and older sister showed similar clinical manifestations. Consanguinity history was not available. Skin biopsy revealed subepidermal vesiculation without inflammation of the dermal portion. Immunofluorescence antigen mapping for K5 could not be performed. Direct immunofluorescence was negative for C3, C1q, IgG, IgM, IgA, and fibrinogen. After informed consent, genomic DNA was extracted from the patient’s blood sample and subjected to next-generation sequencing. Clinical exome sequencing revealed a heterozygous missense mutation of KRT5, NM_000424.3:c.932T>C p.Leu311Pro, subsequently validated through Sanger sequencing [Figure 2]. This variant was not common in the general population, and multiple computational analyses predicted to have a deleterious effect on the gene (PolyPhen2, probably damaging; Mutation Taster, deleterious; SIFT, not tolerated; I-Mutant 2.0, decreased stability). The genetic variant identified in this study is associated with epidermolysis bullosa simplex, listed in the Online Mendelian Inheritance in Man (OMIM #148040). The pathogenicity of the identified variant was determined using previous reports and disease databases, including ClinVar, the Human Gene Mutation Database (HGMD ver 2020.1), and gnomAD. This variation has not been recorded in ClinVar. The observed variant has a minor allele frequency of 0.000004% in the genome AD database (rs59864957) and is absent in the East-Asian population. A mutation in the KRT5 gene with the HGMD accession number CM031234 was identified in a study by Ciubotaru et al. (2003) (PubMed ID: 12707098). The mutation involves a substitution of thymine with cytosine at position 932 (c.932T>C). Therefore, the variant was classified as a likely pathogenic mutation according to American College of Medical Genetics and Genomics (ACMG) guideline.3 Based on clinical manifestations, family history, histopathological findings, and molecular testing, he was diagnosed with localised EBS due to KRT5 mutation.

- Multiple, painful bullae on the soles of both feet (a, b)
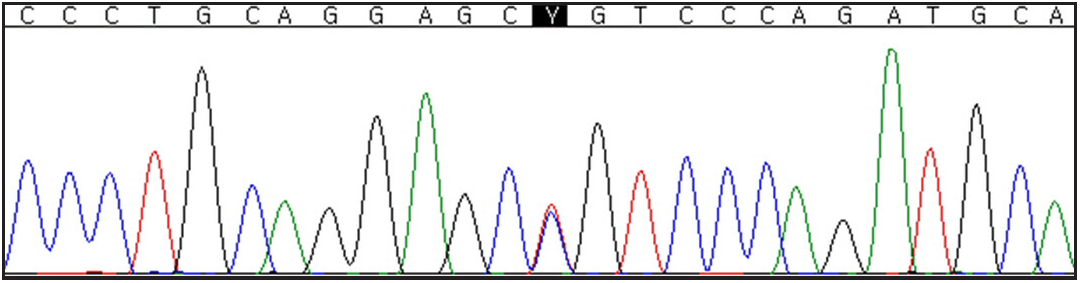
- Chromatogram of Sanger sequencing showing a KRT5 heterozygous mutation c.932T>C that led to p.(Leu311Pro) missense variant
Mutations in KRT5 and KRT14 genes encoding the intermediate filament proteins in basal keratinocytes can cause the collapse of keratin networks, producing intracellular vacuoles due to mechanical stress.4 Sawant et al. found that phosphorylation of threonine 150 (T150) KRT5 is crucial for forming the keratin intermediate filament network, contributing to the pathogenesis of EBS.5 However, the mechanisms by which individual mutations cause cell fragility remain unclear. Further studies should be conducted to identify the molecular pathogenesis of the mutations related to EBS.
At present, the primary treatment of EBS is conservative care. Prevention of friction and avoidance of heat and humidity can decrease the occurrence of bullae.
We searched for gene mutation-related papers on PubMed databases. Detecting this previously unreported mutation (p.L311P) in KRT5 contributes to an enhanced comprehension of the underlying mechanisms involved in localised EBS. Moreover, it offers valuable insights into the relationship between the observed phenotype and the genotype in EBS, further expanding our knowledge in this field. In addition, clinicians should be aware that mutational analysis of family members and genetic counseling is important.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Consensus reclassification of inherited epidermolysis bullosa and other disorders with skin fragility. Br J Dermatol. 2020;183:614-27.
- [CrossRef] [PubMed] [Google Scholar]
- Inherited epidermolysis bullosa: updated recommendations on diagnosis and classification. J Am Acad Dermatol. 2014;70:1103-26.
- [CrossRef] [PubMed] [Google Scholar]
- Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405-24.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The two-chain coiled-coil molecule of native epidermal keratin intermediate filaments is a type I-type II heterodimer. J Biol Chem. 1990;265:8766-74.
- [PubMed] [Google Scholar]
- Threonine 150 phosphorylation of keratin 5 is linked to epidermolysis bullosa simplex and regulates filament assembly and cell viability. J Invest Dermatol. 2018;138:627-36.
- [CrossRef] [PubMed] [Google Scholar]





