Translate this page into:
A case of ulcerative cutaneous sarcoidosis
Corresponding author: Dr. Amal Chamli, Department of Dermatology, Habib Thameur Hospital, Tunis, Tunisia. amal.fmt@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Zaouak A, Chamli A, Ben Samir A, Hlel I, Ben Brahim E, Fenniche S, et al. A case of ulcerative cutaneous sarcoidosis. Indian J Dermatol Venereol Leprol 2023;89:582–4.
Dear Editor,
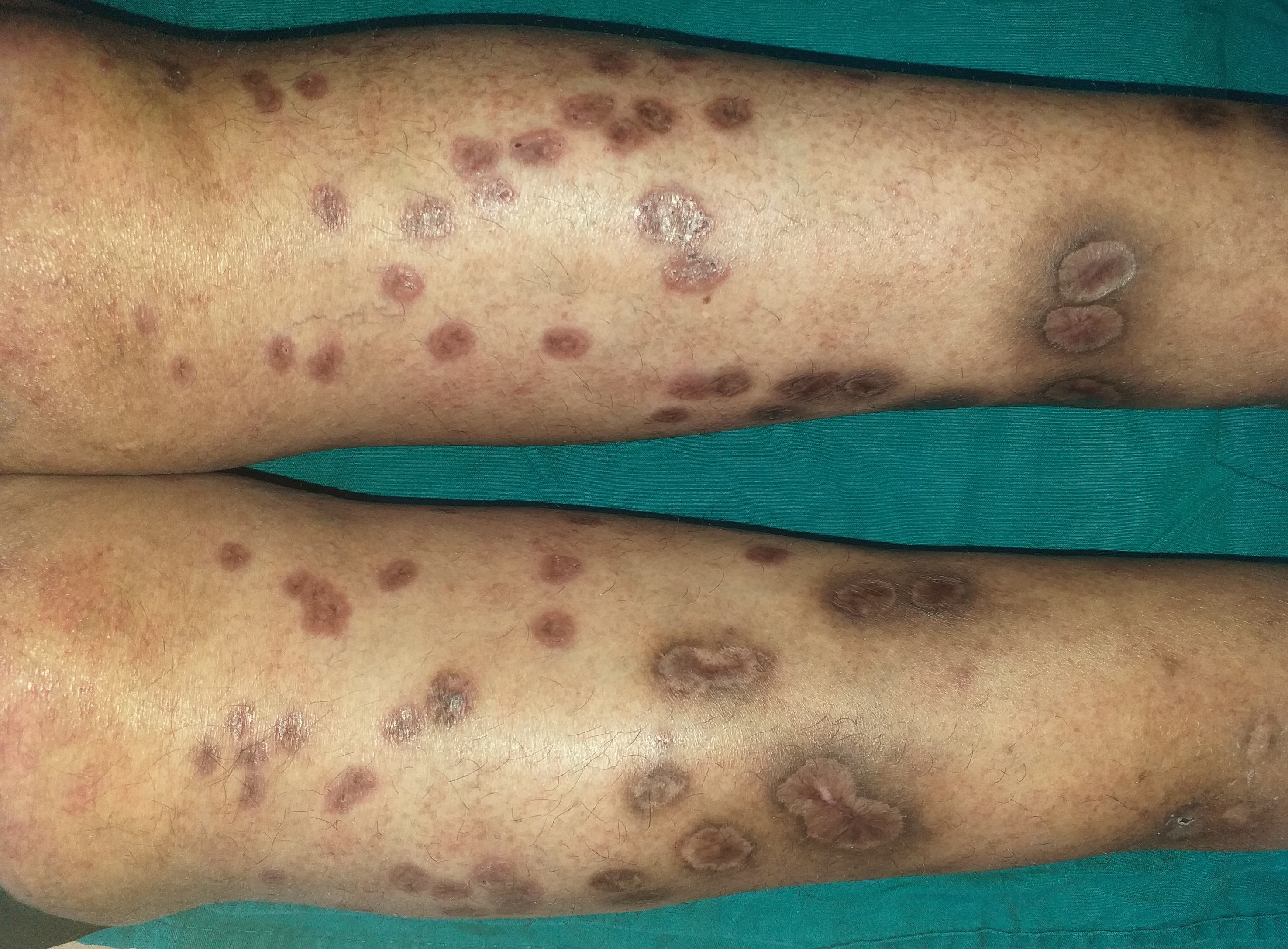
A 54-year-old woman presented to our department with a 2-month history of progressive painful non-healing ulcero-necrotic plaques and nodules on her legs. Cutaneous examination revealed numerous red-brown nodules and plaques of varying sizes measuring 0.5–2 cm in diameter, with punched-out ulcers covered by necrotic brownish crust and infiltrated rolled borders, localised on the bilateral pretibial areas [Figure 1a]. Dermoscopy of the lesions revealed multiple linear and branching vessels overlying translucent orange-yellowish background [Figure 1b]. The patient was afebrile and the remaining physical examination, including lymph nodes, was normal. There was no clinical evidence of arterial or venous insufficiency. The patient denied any pruritus, respiratory symptoms, ocular symptoms, unexplained weight loss or arthralgias. Histopathological examination of the skin specimens revealed non-caseating epithelioid granulomas in the superficial dermis [Figures 2a and b]. There were no polarizable foreign materials within the granulomas. Periodic acid Schiff, acid-fast and gram stains for fungi and bacteria failed to show micro-organisms. Laboratory evaluations revealed neutropenia, lymphopenia, hypochromic microcytic anaemia, low serum ferritin level and elevated erythrocyte sedimentation rate. Serum angiotensin-converting enzyme level was elevated at 91.78 U/L (normal range: 20–70 U/L). Hepatitis B and C, human immunodeficiency virus, syphilis serologies, and QuantiFERON-TB Gold were negative. The antineutrophil cytoplasmic antibody and antiphospholipid antibodies were unremarkable. Cultures for fungi, bacteria and mycobacteria were negative. The computed tomography scan of chest, abdomen and pelvis revealed bilateral hilar and mediastinal lymphadenopathies and peri lymphatic micronodules. Pulmonary function tests, electrocardiogram and ophthalmological examination were unremarkable. Based on these findings the diagnosis of ulcerative cutaneous sarcoidosis was made. The patient was started on hydroxychloroquine 200 mg twice daily along with daily cleaning with povidone iodine, debridement and topical betamethasone. The clinical course was marked by non-healing of the skin ulcers but without the development of new cutaneous lesions. Topical treatment was continued with an anti-ulcer cream, Mebo (moist exposed burn therapy), an oil-based herbal paste and beta-sitosterol. The ulcers healed within three months leaving flat scars [Figure 3]. The patient was referred to the internal medicine department for the management of systemic component of sarcoidosis.
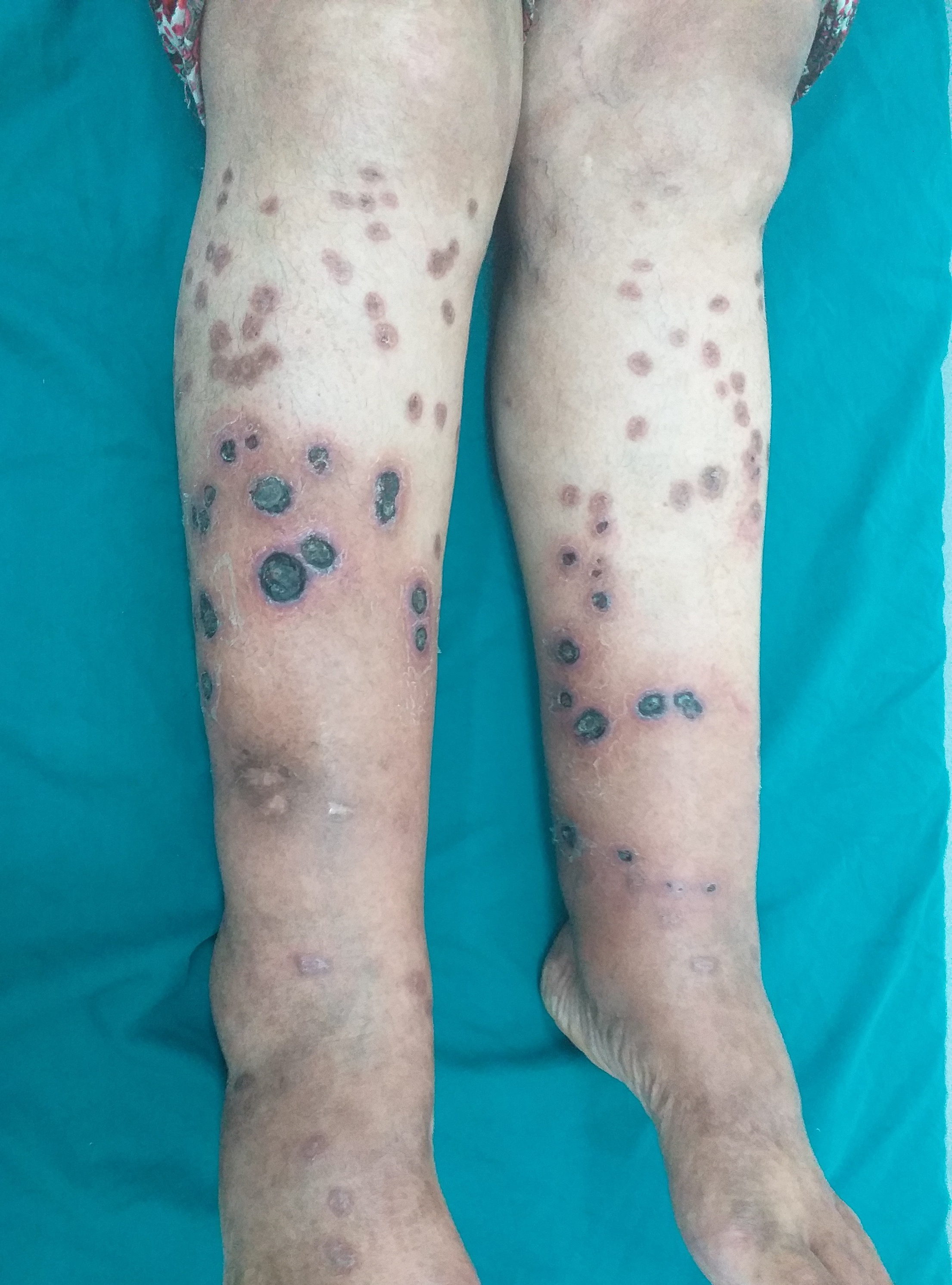
- Multiple ulcers covered by necrotic brownish crust with infiltrated erythematous borders on the lower extremities
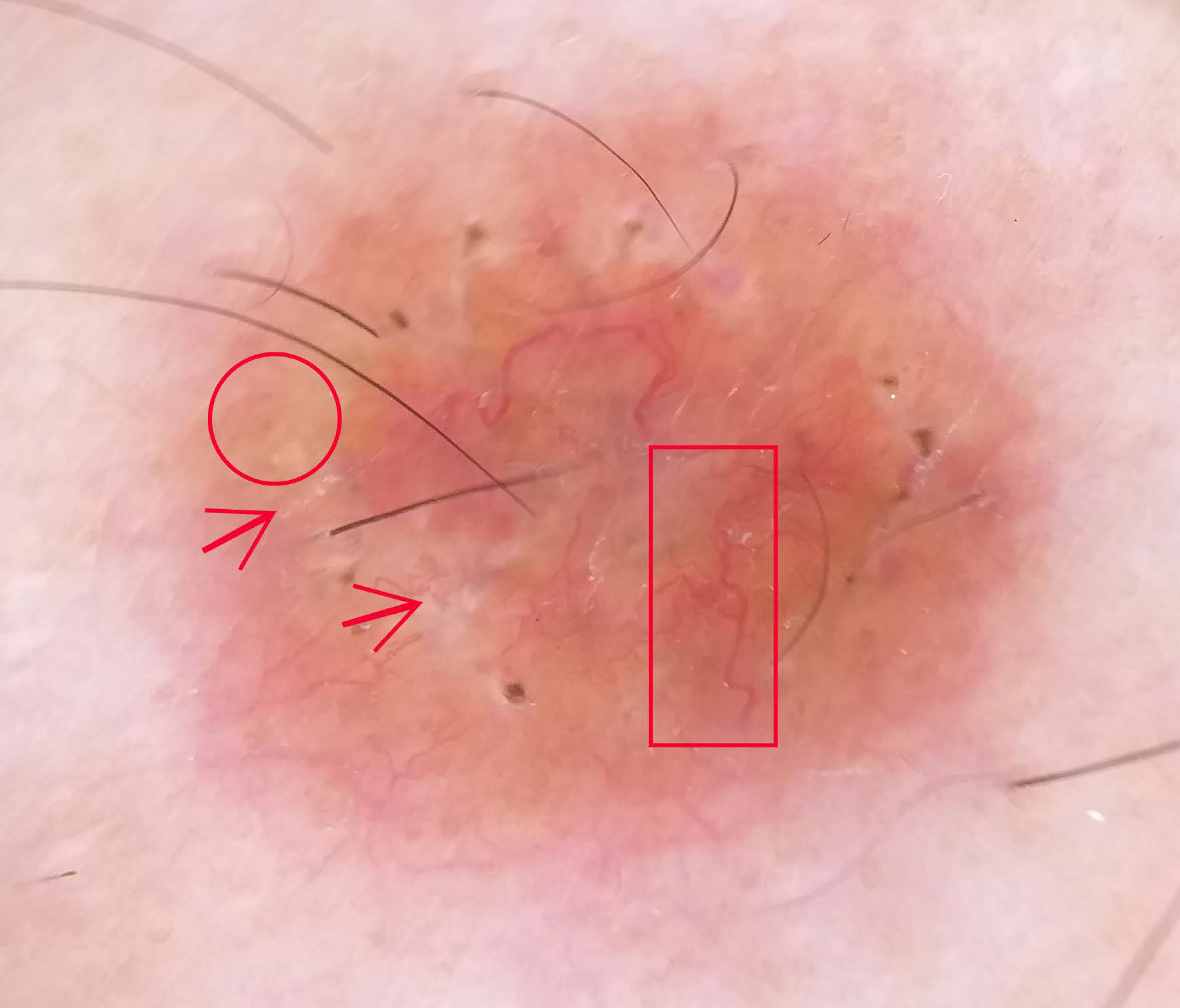
- Dermoscopic examination revealed multiple linear and branching vessels (red rectangle) overlying translucent orange-yellowish background (red circle) with scar-like depigmentation areas, white scales (red arrow) and central serous crust (Dermlite DL4)
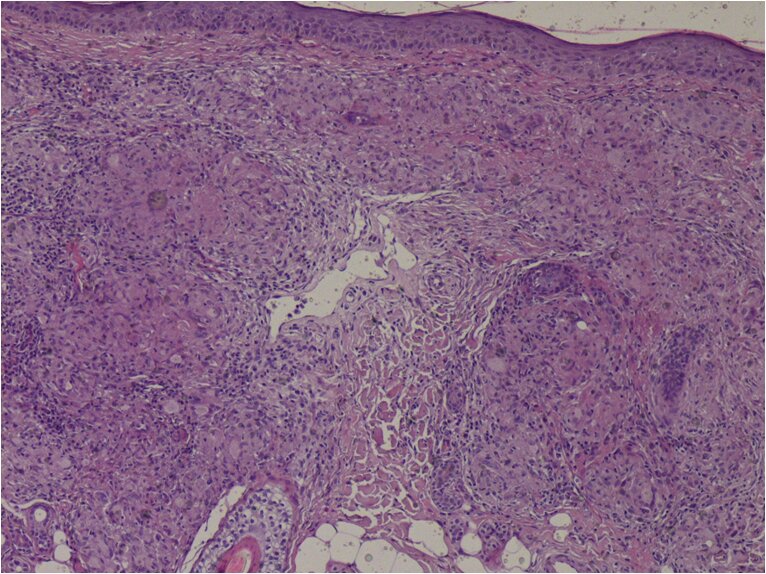
- Non-caseating epithelioid granulomas in the dermis (HE ×200)
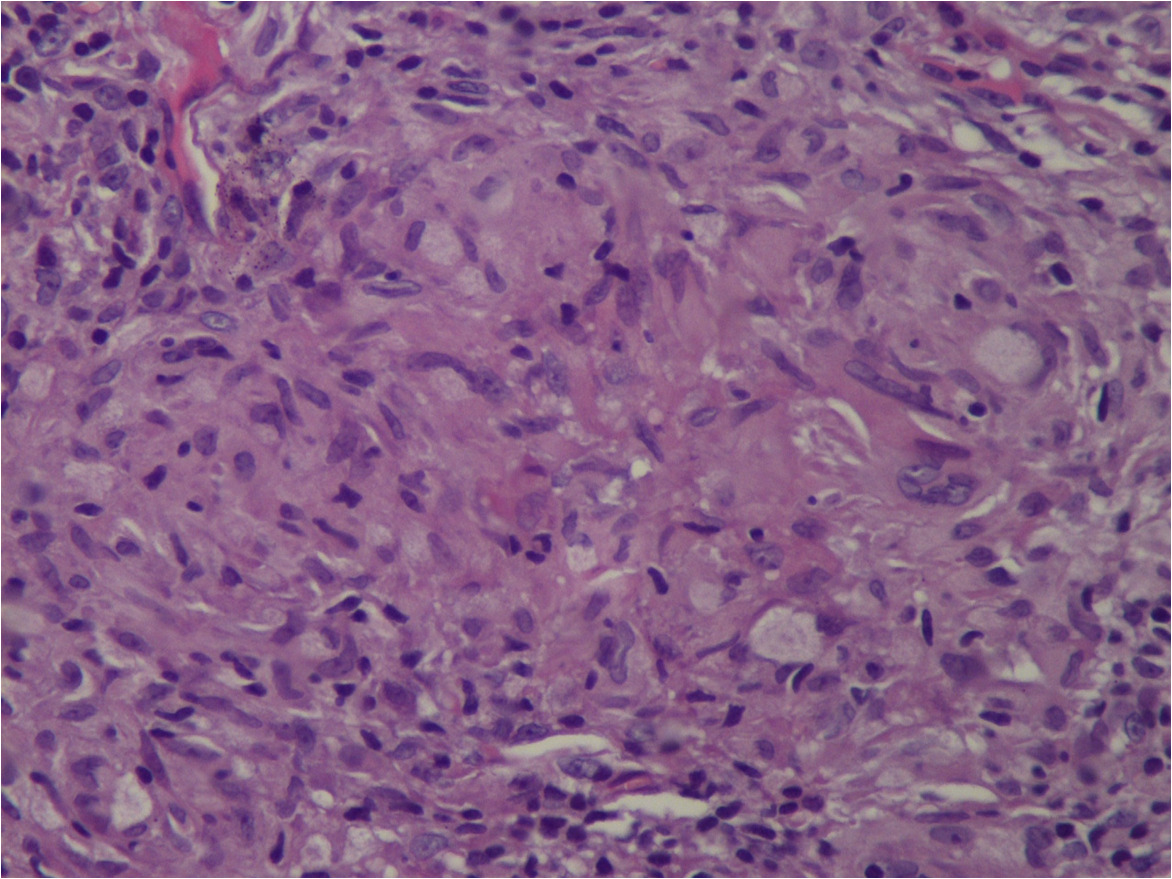
- Sarcoid granuloma composed of epithelioid histiocytes and multi-nucleated giant cells (He ×400)
- Healing ulcers of the legs after 3 months of topical treatment
Discussion
Herein, we describe a rare case of cutaneous sarcoidosis, presenting as punched-out ulcers over the legs of a 54-year-old woman. Cutaneous sarcoidosis is known as the “great imitator” due to variability in manifestations. Indeed, ulcerative cutaneous sarcoidosis is a distinctly unusual manifestation of cutaneous sarcoidosis, affecting 5% of worldwide populations. Blacks and women are more likely to have ulcerative cutaneous sarcoidosis.1 The mechanism of ulceration remains unclear but trauma on atrophic or papulonodular lesions has been reported to be the principal cause of ulceration in sarcoidosis. Granulomatous vasculitis, hyaline degeneration, as well as necrotising granulomas may contribute to other possible mechanisms2. Furthermore, this entity is commonly associated with systemic involvement, as shown in our patient who presented with haematological and mild lung involvement. Ulcers tend to arise within existing papulo-nodules on the lower limbs or de novo. The most frequent location is the pretibial area. In addition, ulcerative cutaneous sarcoidosis may present as ulcerations with purpuric borders, an atrophic base or also necrotic ulcers. Few cases have been described as punched-out ulcers, as in our patient2. In these cases, infectious causes such as syphilis, cryptococcosis, leprosy, cutaneous leishmaniasis, and tuberculosis should be considered in the differential diagnosis. Furthermore, ulcerative cutaneous sarcoidosis of the lower limbs could mimic eschar, superficial pyoderma gangrenosum, necrobiosis lipoidica, perforating diseases, granulomatosis lymphomatoid of Liebow, vascular insufficiency and necrotising vasculitis.3
The presence of non-caseating epithelioid granulomas in histopathology is highly suggestive of ulcerative cutaneous sarcoidosis but is not specific. Therefore, appropriate stains, cultures and polymerase chain reaction (PCR) are crucial to differentiate ulcerative cutaneous sarcoidosis from skin infections such as syphilis, leishmaniasis and tuberculosis.2
In addition, our case may mimic perforating sarcoidosis as well as perforating granuloma annulare or Kyrle disease since the similar presentation. However, in our patient, transepidermal elimination of sarcoid granuloma or collagen was not observed in histopathology.4
Cutaneous manifestations of lymphomatoid granulomatosis of Liebow present with violaceous and hyperpigmented ulcerated nodules of the trunk and extremities and are usually associated with lung involvement. Histology shows characteristically an inflammatory angiocentric infiltrate, composed of polymorphous mononucleated cells often associated with necrosis, unlike our case. Vascular insufficiency could be excluded by arterial and venous Doppler ultrasound and necrotising vasculitis is eliminated by the negativity of antineutrophil cytoplasmic antibodies (ANCAs) and the absence of vasculitis on histology. In addition, as in granulomatous diseases, dermoscopy can be of important diagnostic tool, showing yellow-orange background, and white areas associated with linear vessels. Hence, there is no diagnostic test for sarcoidosis and the diagnosis is made by combining clinic, dermoscopic, histopathological, biological and radiological findings, as in the current case.
In ulcerative cutaneous sarcoidosis, patients are commonly refractory to many types of treatment. Systemic corticosteroids have been reported as standard therapy in ulcerative cutaneous sarcoidosis. Topical treatments alone have been reported to fail.2 Interestingly, our patient was treated successfully with hydroxychloroquine and topical ulcer treatment. We started conventional topical treatment but since there was no improvement, we decided on a trial with Mebo. In fact, Mebo (moist exposed burn ointment) or moist exposed burn treatment/therapy is traditional Chinese medicine. Its main ingredient is beta-sitosterol, a plant-derived steroid with anti-inflammatory and anti-pyretic properties.5 In summary, practitioners should suspect ulcerative cutaneous sarcoidosis in front of ulcero-necrotic plaques of the lower extremities. Furthermore, this case is being reported to draw the attention of practitioners to the importance of local measures in the treatment of ulcerative cutaneous sarcoidosis.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- Atypical ulcers: Atypical ulcers. Dermatol Ther. 2013;26:222-35.
- [CrossRef] [PubMed] [Google Scholar]
- Clinicopathologic features of ulcerative-atrophic sarcoidosis. Int J Dermatol. 2004;43:108-12.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous sarcoidosis: Differential diagnosis. Clin Dermatol. 2007;25:276-87.
- [CrossRef] [PubMed] [Google Scholar]
- Generalized perforating granuloma annulare. J Am Acad Dermatol. 1992;27:319-22.
- [CrossRef] [PubMed] [Google Scholar]
- Analgesic and anti-inflammatory activity of β-sitosterol isolated from Nyctanthes arbortristis leaves. Inflammopharmacology. 2012;20:219-24.
- [CrossRef] [PubMed] [Google Scholar]





