Translate this page into:
A challenging case of Kikuchi-Fujimoto disease with systemic lupus erythematosus complicated with hemophagocytic lymphohistiocytosis in a young man
Corresponding author: Dr. Chandra Sekhar Sirka, Department of Dermatology, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India. csirka2006@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Pradhan S, Sirka CS, Dash G, Sahu K, Rout AN. A challenging case of Kikuchi-Fujimoto disease with systemic lupus erythematosus complicated with hemophagocytic lymphohistiocytosis in a young man. Indian J Dermatol Venereol Leprol 2021;87:78-82.
Sir,
Kikuchi-Fujimoto disease or histiocytic necrotizing lymphadenitis is an extremely rare, self-limiting disorder that presents with fever and painful, unilateral cervical lymphadenopathy in previously healthy individual.1
Skin manifestations are found in 16–40% of patients and often simulates systemic lupus erythematosus.2,3Although self-limiting, it can be sometimes complicated with secondary hemophagocytic lymphohistiocytosis thereby posing challenges in both diagnosis and treatment.
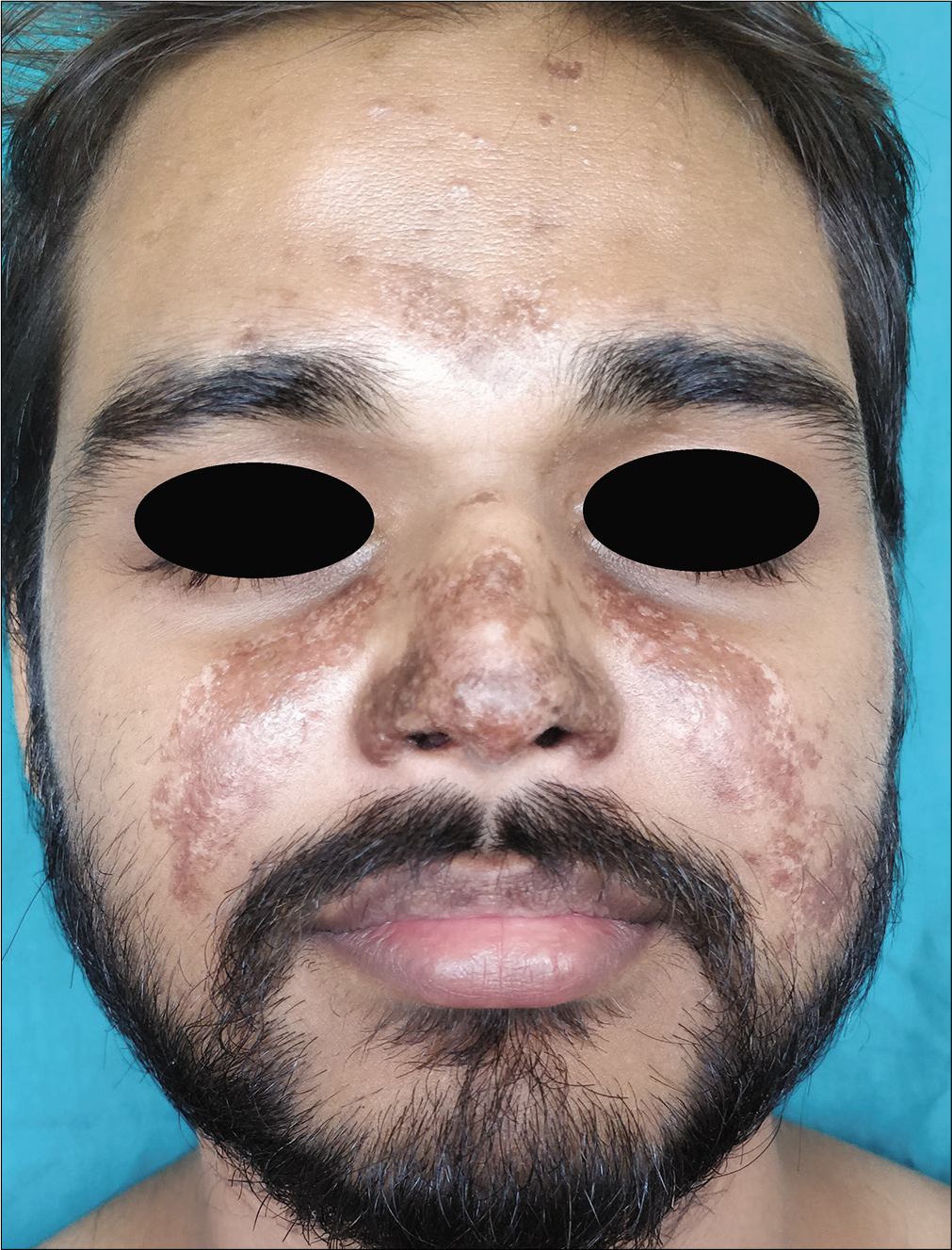
A 26-year-old man presented to the dermatology outpatients' department of the All India Institute of Medical Sciences, Bhubaneswar with single asymptomatic swelling on the left cervical area for8 weeks and reddish skin lesions on photoexposed areas along with oral ulcers, fever, joint pain, nausea and vomiting since 6 weeks. Examination revealed single enlarged non-tender left cervical lymph node of size 4cm × 4cm without any surface change, skin lesions in the form of multiple erythematous edematous macules, plaques with necrosis on surface distributed on the forehead, V area of the neck, upper back, extensor of arms along with malar erythema and edema, ulcers on the lips and hard palate [Figures 1-3]. Systemic examination revealed hepatosplenomegaly.Hemoglobin was 8 g%, antinuclear antibody (4 + speckled pattern) and anti-double-stranded DNA were positive. Other hematological parameters were within normal limits. Liver function tests were deranged (aspartate transaminase-349, upper limit of normal-37; alanine aminotransferase-313, upper limit of normal-40). Renal function tests, urine routine microscopy and chest x-ray were normal. Skin biopsy from the ulcerated plaque on the chest showed segmental epidermal necrosis, subepidermal split with perivascular lymphocytic infiltration[Figure 4]. Based on cutaneous and laboratory findings a provisional diagnosis of systemic lupus erythematosus associated lymphadenitis was made. Lymph node biopsy revealed the absence of neutrophils, hematoxylin body and paracortical foci of coagulative necrosis containing karyorrhectic debris surrounded by histiocytes suggestive of necrotizing lymphadenitis [Figure 5]. Immunohistochemistry revealed the predominance of a cluster of differentiation 68/ myeloperoxidase + histiocytes [Figure 6]. The patient was finally diagnosed with both Kikuchi-Fujimoto disease and systemic lupus erythematosus. The treatment was started with oral prednisolone 0.5mg/kg/day (40 mg/day) along with hydroxychloroquine 6.5mg/kg/day. After around 10 days of medication, the lymph node size decreased by 50% and skin and mucosal lesions started healing. However high-grade fever, sweating, nausea and vomiting, hepatosplenomegaly and deranged liver function testpersisted leading to suspicion of hemophagocytic lymphohistiocytosis. Further investigations revealed raised lactate dehydrogenase- 23499(N: 225– 450U/L), fasting hypertriglyceridemia TG-224mg/dL (N-60-150), fibrinogen-290.8 mg/dl (N: 200-400mg/ dl), hyperferritinemia (16,500, N: 18-270 ng/mL). Bone marrow biopsy was normal. The total HScore came as 218(>169)[Table 1]. The patient was diagnosed to have hemophagocytic lymphohistiocytosis. Oral prednisolone was increased to 80 mg per day. After 3 weeks systemic symptoms subsided along with complete disappearance of cervical swelling and skin lesions [Figures 7-9]. At the end of 1 month of treatment, the HScore came down to 18 with lactate dehydrogenase-463.8 U/L, ferritin-88.5 ng/mL, fibrinogen- 389 mg/dL, triglyceride- 140 mg/dL, Hb- 16 g/dL, aspartate transaminase-31 U/L and alanine aminotransferase- 65 U/L.Prednisolone was subsequently tapered and stopped after 22 weeks. Currently, the patient is only on hydroxychloroquine without any recurrence of cervical swelling, skin lesions and systemic symptoms.

- Enlarged left cervical lymphnode

- Malar rash-erythema and edema onthe malar area and dorsum of nose

- Erythematous macules, plaques with surface necrosis “V”area of the neck
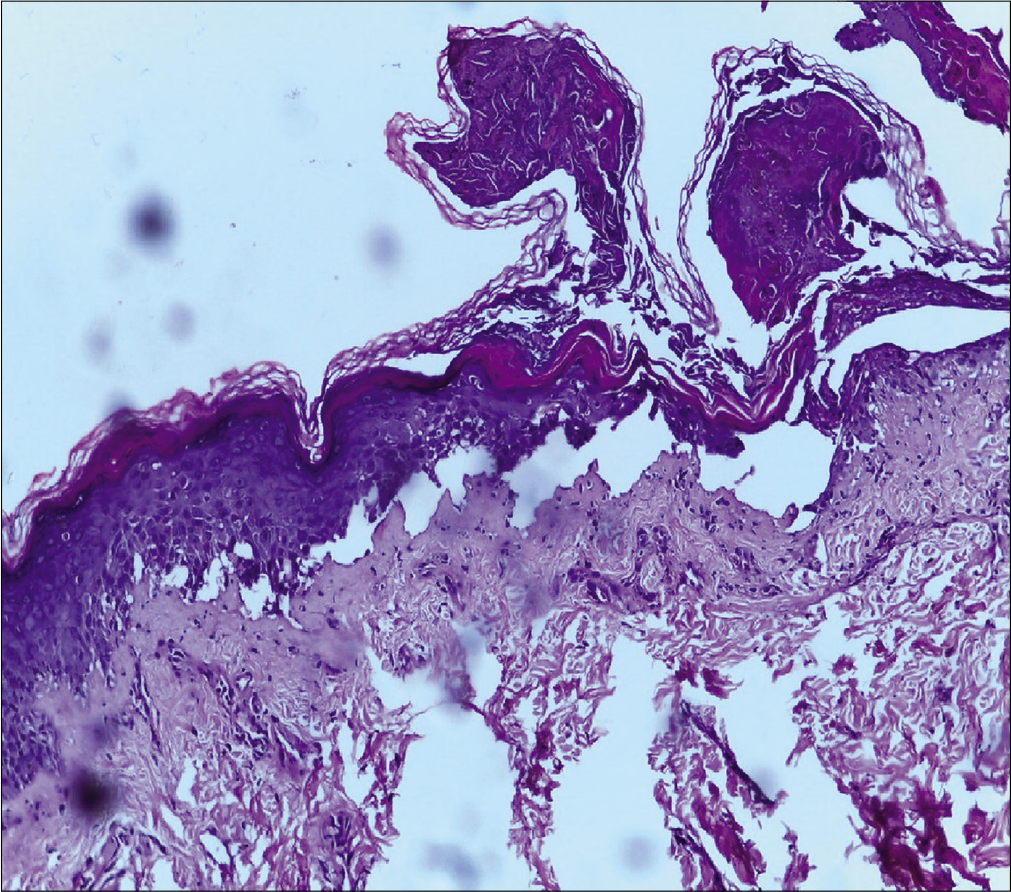
- H and E stain ×10, segmental epidermal necrosis, subepidermal split
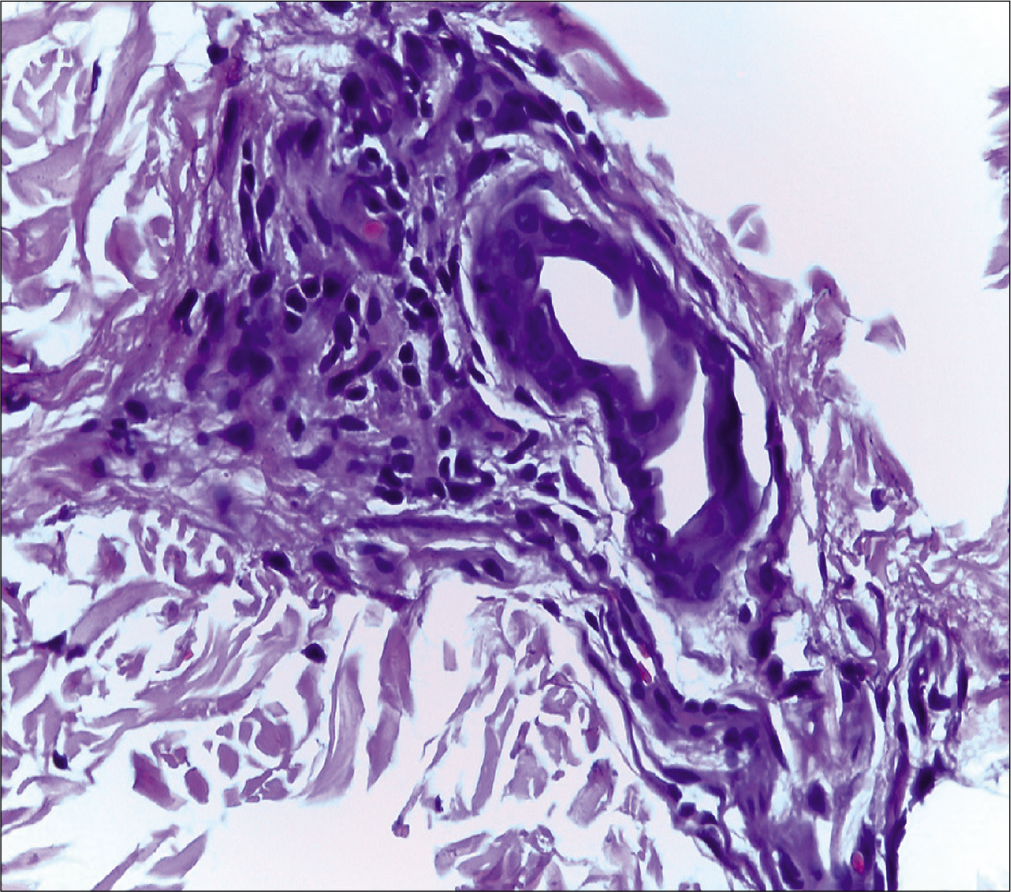
- H and E stain ×40, perivascular lymphocytic infiltration
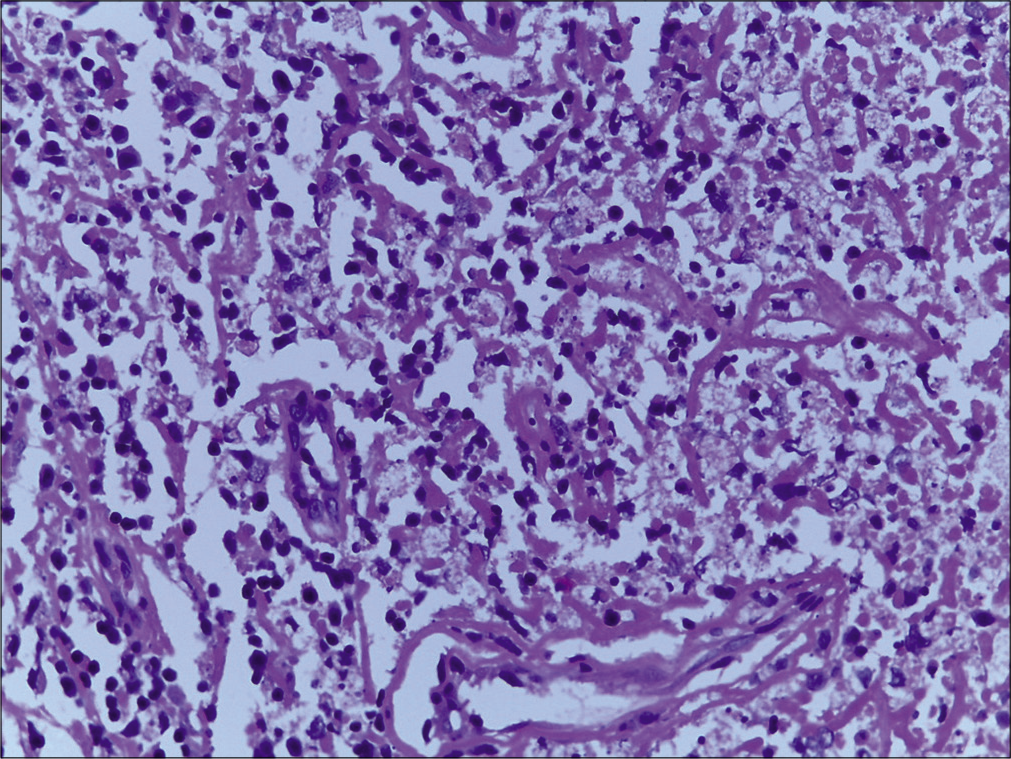
- Lymphnode histology: H and E stain×40, absence of neutrophils, hematoxylin body and paracortical foci of coagulative necrosis containing karyorrhectic debris surrounded by histiocytes
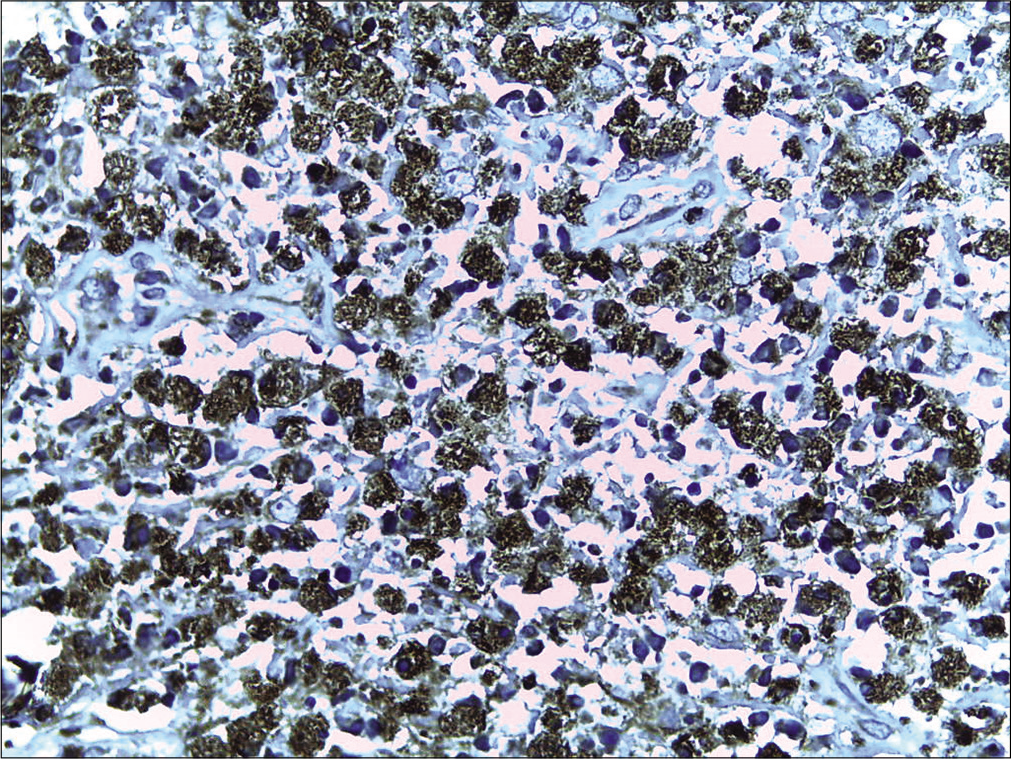
- A cluster of differentiation 68 + histiocytes on immunohistochemistry

- Complete disappearance of enlarged cervical lymphnode
- Subsidence of malar erythema and edema with postinflammatory hyperpigmentation
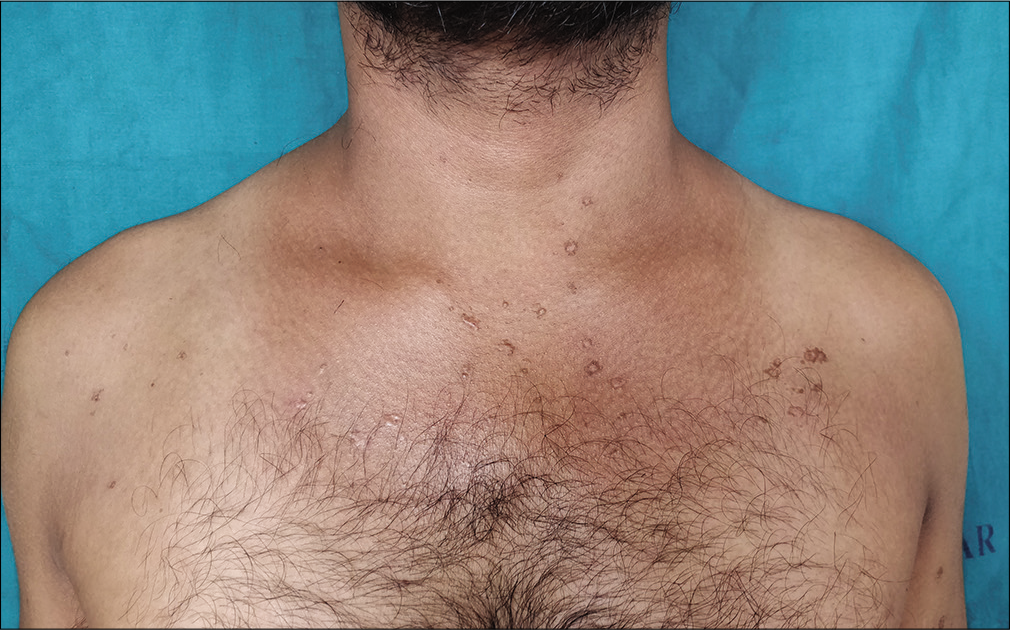
- Subsidence of erythematosus plaques with postinflammatory hyperpigmentation
| Parameter | HScore | Our patient Baseline (total score=218) |
|---|---|---|
| Fever (°C) | 0 (<38.4), 33 (38.4-39.4) or 49 (>39.4) | >39.4 (49) |
| Organomegaly | 0 (no), 23 (hepatomegaly or splenomegaly) or 38 (hepatomegaly and splenomegaly) | Hepatosplenomegaly (38) |
| Cytopenia | 0(one lineage), 24(two lineages) or 34(three lineages) | Hb 8 g%, (0) |
| Ferritin (ng/mL) | 0 (<2000), 35 (2000-6000) or 50 (>6,000) | 16,500, (50) |
| Triglyceride (mmol/L) | 0 (<1.5), 44 (1.5-4) or 64 (>4) | 2.6 (44) |
| Fibrinogen (g/L) | 0 (>2.5) or 30 (<2.5) | 3.89 g/L (0) |
| Hemophagocytosis in bone marrow | 0 (no) or 35 (yes) | No (0) |
| AST (IU/L) | 0 (<30) or 19 (>30) | 349 (19) |
| Known underlying immunosuppression | 0 (no) or 18 (yes) | Yes (18) |
AST: Aspartate aminotransferase, Hb: Hemoglobin
Kikuchi-Fujimoto disease is characterized by lymphadenopathy (cervical lymph nodes 80%), fever, flu-like prodrome.1 Skin findings include malar rash, macular, papular and morbilliform rash, nodules, urticaria and often resemble systemic lupus erythematosus.2,3 Other systemic manifestations include hepatosplenomegaly, aseptic meningitis, acute cerebellar ataxia, encephalitis and polyarthritis.4 Owing tosimilar presentations, it is often difficult to distinguish Kikuchi-Fujimoto disease and systemic lupus erythematosus clinically. Antinuclear antibodies and anti-double-stranded DNA are negative in cases of Kikuchi-Fujimoto disease. Histopathology of lymph nodes shows absence or paucity of hematoxylin bodies, plasma cells and neutrophils in Kikuchi-Fujimoto disease which are usually seen in systemic lupus erythematosus. In addition, T lymphocytes predominate in Kikuchi-Fujimoto disease, whereas B lymphocytes predominate in systemic lupus erythematosus.3 Another close differential diagnosis is non-Hodgkin lymphoma. However, immunohistochemistry studies and bone marrow study can help in distinguishing both conditions. Our patient had fever, joint pain, oral ulcers, and skin lesions resembling systemic lupus erythematosus, anemia, positive antinuclear antibodies and anti-double-stranded DNA. Hence, he fulfilled more than four American College of Rheumatology criteria of systemic lupus erythematosus. Histopathology and immunohistochemistry study of lymph node revealed paracortical foci of coagulative necrosis containing karyorrhectic debris with the absence of neutrophils, hematoxylin body and presence of numerous a disease. The patient was finally diagnosed to have Kikuchi-Fujimoto disease and systemic lupus erythematosus.
Mostly, watchful waiting without any medications is the most common approach to treat Kikuchi-Fujimoto disease, due to its benign course. The use of oral corticosteroids is recommended in severe extranodal or generalized Kikuchi disease.4 For systemic lupus erythematosus depending on disease severity, hydroxychloroquine and/or immunosuppressives are used.However, in disease flare with systemic manifestations corticosteroids are the main stay of therapy in systemic lupus erythematosus.
In our case, use of prednisolone 0.5 mg/kg along with hydroxychloroquine 6.5 mg/kg improved his joint pain, skin lesions and decreased lymph node size by 50%over 10 days. However persistenthigh-grade fever, myalgia and weakness with profuse sweating lead to suspicion of hemophagocytic lymphohistiocytosis which was confirmed by higher Hscore 218. Probability score (HScore) is considered for early diagnosis of hemophagocytic lymphohistiocytosis.5 TheHScore is calculated by taking into consideration the presence of immunosuppression, fever, cytopenia (s), splenohepatomegaly, hyperferritinemia, hypertriglyceridemia, evidence of histiocytic hemophagocytosis in bone marrow aspirate and elevated liver cluster of differentiation 68/myeloperoxidase suggestive of histiocytic necrotizing lymphadenitis or Kikuchi-Fujimoto transaminases. A composite score of 169 has a sensitivity of 93% and specificity of 86% with the accurate classification of hemophagocytic lymphohistiocytosis in 90% of the patients.
Hemophagocytic lymphohistiocytosis is a rare, potentially fatal, hyperinflammatory syndrome with severe constitutional symptoms and carries a poor prognosis.5 The clinical characteristics of hemophagocytic lymphohistiocytosis associated with Kikuchi-Fujimoto disease may be difficult to understand because of rarity. In contrast to the benign course of Kikuchi-Fujimoto disease, the association of hemophagocytic lymphohistiocytosis increases mortality and hence needs early intervention. Our case had hemophagocytic lymphohistiocytosis associated with Kikuchi-Fujimoto disease along with systemic lupus erythematosus which has been rarely reported in literature which was diagnosed and treated successfully. Hence, physicians must be aware of such an association in poorly responding cases with lymphadenopathy and systemic symptoms so they can be investigated, diagnosed and treated at the earliest.A review of the literature showed only two case reports of such association.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal the identity but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Enigmatic Kikuchi-Fujimoto disease: A comprehensive review. Am J Clin Pathol. 2004;122:141-52.
- [CrossRef] [PubMed] [Google Scholar]
- Kikuchi's disease: Case report and systematic review of cutaneous and histopathologic presentations. J Am Acad Dermatol. 2008;59:130-6.
- [CrossRef] [PubMed] [Google Scholar]
- Kikuchi's disease (histiocytic necrotizing lymphadenitis):A clinicopathologic study of 79 cases with an analysis of histologic subtypes, immunohistology, and DNA ploidy. Am J Surg Pathol. 1995;19:798-809.
- [CrossRef] [PubMed] [Google Scholar]
- Enthesitis-related arthritis in Kikuchi-Fujimoto disease. Mod Rheumatol. 2008;18:492-5.
- [CrossRef] [PubMed] [Google Scholar]
- Development and validation of the HScore, a score for the diagnosis of reactive hemophagocytic syndrome. Arthritis Rheumatol. 2014;66:2613-20.
- [CrossRef] [PubMed] [Google Scholar]





