Translate this page into:
A controlled trial of narrowband ultraviolet B phototherapy for the treatment of uremic pruritus
2 Department of Dermatology and Venereology, Government Medical College, Kozhikode, Kerala, India
3 Department of Nephrology, Government Medical College, Kozhikode, Kerala, India
4 General Hospital, Kasaragod, Kerala, India
Correspondence Address:
Pentamveli Beegum Sherjeena
Melethil House, Karinchapadi, Vattaloor P.O., Malappuram - 676 507, Kerala
India
| How to cite this article: Sherjeena PB, Binitha MP, Rajan U, Sreelatha M, Sarita S, Nirmal C, Deepthi NS. A controlled trial of narrowband ultraviolet B phototherapy for the treatment of uremic pruritus. Indian J Dermatol Venereol Leprol 2017;83:247-249 |
Sir,
Chronic renal disease is associated with many cutaneous manifestations. Uremic pruritus is very resistant to treatment and markedly affects the quality of life.[1],[2] We performed a controlled trial with systematic allocation in order to analyze the effects of narrowband ultraviolet B phototherapy in patients suffering from uremic pruritus.
The study group comprised thirty consecutive patients with Stage IV and V chronic renal disease who attended the outpatient clinic of Government Medical College, Kozhikode. from April 2012 to March 2013. They were referred from the department of nephrology for management of pruritus. The study was approved by the Institutional Ethics Committee, and written informed consent was obtained from all study participants. Patients above the age of 18 years, and those having a uremic pruritus score of more than 5 on the visual analog scale were enrolled for the study. Patients with a history of photosensitivity, early renal disease (Stage I, II and III), pregnancy and lactation were excluded. Those who had pruritus secondary to other skin or systemic diseases were also excluded. Uremic pruritus was defined as pruritus appearing shortly before the onset of dialysis, with three or more episodes of itching over a period of two weeks. The symptoms appeared at least once a day, lasted for at least a few minutes and caused discomfort. The itch appeared in a regular pattern during preceding six months.[3]
The patients were allocated alternately to Group A or Group B, which comprised fifteen patients each. Phototherapy was administered using the Spiegel series ultraviolet A 18 narrowband ultraviolet B 18 whole body phototherapy chamber, marketed by DermaIndia. The Group A patients received narrowband ultraviolet B phototherapy every third day for fifteen sessions. No antihistamines or topical emollients were used. As all of them had type IV and V skin phototypes, a starting dose of 200 mJ/cm2 was given, according to the St. John's phototherapy guidelines. It was increased by 10% every successive session, to a maximum of 1038 mJ at the end of fifteen sessions. Group B patients were treated only with topical liquid paraffin and oral cetirizine (10 mg/day) for the same duration. All patients were followed up to note the improvement of pruritus or side effects due to narrowband ultraviolet B phototherapy (erythema, photosensitivity, vesiculobullous lesions or increased pruritus). The severity of pruritus was evaluated in both groups using the visual analog scale. This was done at baseline, once weekly for the first four weeks, and then at the end of the 3rd and 6th month. The visual analog scale is a consistent and objective method to assess the intensity of pruritus. A questionnaire was used to record the distribution, severity, frequency and sleep disturbances during the past 24 hours on a scale of 1–10, ranging from no pruritus to intractable pruritus.[4]
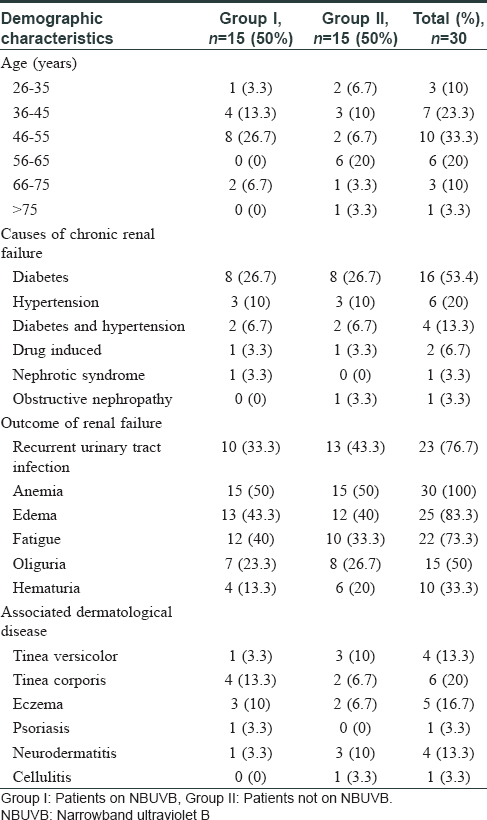
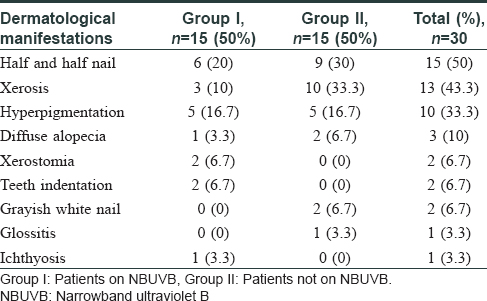
Statistical analysis was performed using the statistical package for the social sciences 17.0 software. Calculation of frequency tables and plotting of graphs was done using the master chart. Intergroup comparisons were done by the Mann–Whitney U-test, and intragroup analysis was done by the Friedman and Wilcoxon test. The mean age of patients was 45.7 years, with a male to female ratio of 2:1. All of them were on maintenance hemodialysis. The duration of chronic renal disease was more than six years in 21 (70%) patients. Diabetes mellitus was the most common cause of chronic renal failure, seen in 16 (53.3%) patients. The demographic features, causes and outcome of chronic renal failure and associated dermatological diseases are shown in [Table - 1]. Twenty (66.7%) patients were on antidiabetic drugs, ten (33.3%) on antihypertensives, and four (13.3%) on lipid lowering agents. The most common dermatological manifestation was half-and-half nails, seen in fifteen (50%) patients. Xerosis was seen in thirteen (43.3%) patients [Table - 2].
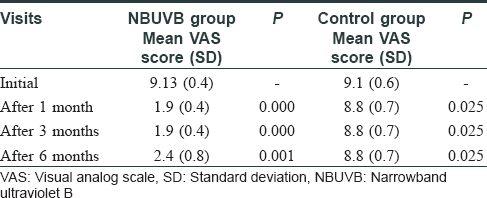
No significant differences in clinical features or laboratory results were found between the groups at the beginning of the study. The blood urea and serum creatinine levels were elevated in all patients. At the beginning of the study, the visual analog scale of pruritus ranged from 8 to 10 in both groups. Following phototherapy, a decrease in pruritus was noticed as early as the fourth session (285 mJ/cm2) in Group A. It decreased to a level of 1–3 in all patients after three months of therapy. A maximum of seven sessions (405 mJ/cm2) was required to show improvement. Re-evaluation at the end of six months revealed that this improvement was sustained in all except for two patients, whose visual analog scale decreased to 2 at the end of three months, but showed a marginal increase to 4 at the end of six months. The decrease of pruritus in the control group was unremarkable, with scores varying from 7 to 9. At the end of the study period, the final treatment outcome revealed a significant decrease of pruritus (P = 0.001) in the study group compared to the control group [Table - 3]. No side effects were observed due to narrowband ultraviolet B phototherapy, probably due to the short duration and low dose. At the end of the study, the blood urea and serum creatinine levels remained unchanged in both groups.
The mechanism of action of phototherapy in the reduction of pruritus is unclear. Photo-inactivation of pruritogenic substances, formation of photo-adducts with antipruritic effects, and production of vitamin D that alters divalent ions have been suggested as possible reasons.[5] In addition, ultraviolet B phototherapy attenuates T-helper 1 cell differentiation and decreases the production of interleukin-2.[6]
The small sample size, short duration of follow-up, lack of blinding and allocation concealment were the limitations of our study. The results demonstrate that narrowband ultraviolet B phototherapy may be considered as an effective therapeutic option for the treatment of the intractable uremic pruritus. Better designed studies are needed to confirm its long-term efficacy and safety.
Acknowledgment
We are grateful to Dr. Biju George, Assistant Professor, Department of Community Medicine, for his valuable assistance with the statistical analysis of our study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Udayakumar P, Balasubramanian S, Ramalingam KS, Lakshmi C, Srinivas CR, Mathew AC. Cutaneous manifestations in patients with chronic renal failure on hemodialysis. Indian J Dermatol Venereol Leprol 2006;72:119-25.
[Google Scholar]
|
| 2. |
Narita I, Alchi B, Omori K, Sato F, Ajiro J, Saga D, et al. Etiology and prognostic significance of severe uremic pruritus in chronic hemodialysis patients. Kidney Int 2006;69:1626-32.
[Google Scholar]
|
| 3. |
Zucker I, Yosipovitch G, David M, Gafter U, Boner G. Prevalence and characterization of uremic pruritus in patients undergoing hemodialysis: Uremic pruritus is still a major problem for patients with end-stage renal disease. J Am Acad Dermatol 2003;49:842-6.
[Google Scholar]
|
| 4. |
Elman S, Hynan LS, Gabriel V, Mayo MJ. The 5-D itch scale: A new measure of pruritus. Br J Dermatol 2010;162:587-93.
[Google Scholar]
|
| 5. |
Mettang T, Pauli-Magnus C, Alscher DM. Uraemic pruritus – New perspectives and insights from recent trials. Nephrol Dial Transplant 2002;17:1558-63.
[Google Scholar]
|
| 6. |
Ko MJ, Yang JY, Wu HY, Hu FC, Chen SI, Tsai PJ, et al. Narrowband ultraviolet B phototherapy for patients with refractory uraemic pruritus: A randomized controlled trial. Br J Dermatol 2011;165:633-9.
[Google Scholar]
|
Fulltext Views
4,058
PDF downloads
1,538





