Translate this page into:
A cross-sectional study to analyze the clinical subtype, contact sensitization and impact of disease severity on quality of life and cost of illness in patients of hand eczema
Correspondence Address:
Deepika Pandhi
Department of Dermatology and STD, University College of Medical Sciences and Associated Guru Teg Bahadur Hospital, University of Delhi, Delhi - 110 095
India
| How to cite this article: Kataria V, Pandhi D, Bhattacharya SN. A cross-sectional study to analyze the clinical subtype, contact sensitization and impact of disease severity on quality of life and cost of illness in patients of hand eczema. Indian J Dermatol Venereol Leprol 2020;86:663-668 |
Abstract
Background: The high incidence, chronicity, frequent recurrences and severity of hand eczema leads to a massive impact on the quality of life. Despite great medical and socioeconomic importance, there is a paucity of data that addresses the cost of illness and economic factors associated with hand eczema. Most of the studies have originated from Europe and none have been reported from India.
Aim: To analyze the clinical subtype, the pattern of contact sensitization and the impact of severity of disease on the quality of life and cost of illness in patients of hand eczema.
Methods: Hundred patients of hand eczema were recruited and evaluated for morphological patterns of the condition, hand eczema severity index and quality of life (Dermatology Life Quality Index questionnaire). All patients were subjected to patch tests with Indian standard series, cosmetic series and personal or work-related products. The economic burden of hand eczema was measured by both its direct and indirect costs.
Results: Morphologically, chronic dry fissured eczema 36 (36%) was the most common pattern followed by mixed type 19 (19%), hyperkeratotic palmar eczema 15 (15%), vesicular eczema with recurrent eruption 9 (9%), nummular eczema 7 (7%) and wear and tear dermatitis 7 (7%). Seventy nine patients gave positive patch test results. Etiological profile of the most common allergens, as established with a patch test, include potassium dichromate 18 (18%) followed by cetrimonium bromide 17 (17%), nickel 16 (16%), gallate 14 (14%), garlic 9 (9%) and patient's own product 8 (8%). Allergic contact dermatitis was the most common clinical pattern of hand eczema seen in 45 (45%) patients, followed by an irritant 14 (14%) and a combination of both 13 (13%). The average total cost of illness was INR 13,783.41 (0–93,000) per individual per year with an average direct cost of INR 2,746.25 ± 1,900 and indirect cost of INR 4911.73 ± 13237.72, along with a positive correlation with the Dermatology Life Quality Index (P = 0.00). The hand eczema severity index was marginally correlated with direct costs (P = 0.07) and highly correlated with indirect costs (P = 0.024).
Conclusion: Hand eczema has a huge impact on the quality of life and economic consequences.
Limitations: In our study, parameters like Dermatology Life Quality Index and hand eczema severity index could have been affected by the chronicity of disease as being a tertiary referral centre, most of the recruited patients had severe and persistent hand eczema at the time of visit. Also, cost of illness was based on retrospective calculations on recall basis.
Introduction
Hand eczema is a multifactorial, common dermatological disorder with a the chronic and relapsing course.[1] Predisposing endogenous factors and external factors both play important roles in hand eczema causation. A poor prognosis is associated with a young age of disease onset, history of atopic dermatitis and extensive involvement with eczema. Hand eczema is, usually disabling or distressing to the sufferer, difficult to treat and likely to negatively impact the quality of life. This leads to psychosocial interference, sleep or mood disturbance, change of daily activities and cessation of hobbies. Thereby, it emphasizes the need for a detailed evaluation using the Dermatology Life Quality Index subscales to identify the psychosocial impact of the disease.[2] It is broadly assumed that the costs incurred by patients of chronic hand eczema are significant.[3],[4] However, despite its great medical and socioeconomic importance, there is a paucity of data that addresses the cost of illness and economic factors in chronic hand eczema. Most of the studies have originated from Germany and Europe, where the cost of illness was found to be highly influenced by gender, occupation, sick leaves and severity of the disease.[3],[4] As there may be significant sociocultural differences, we decided to study the impact of disease on the quality of life and assess the direct and indirect cost of illness in patients with hand eczema.
Methods
The present cross-sectional study recruited patients from the outpatient department of Guru Teg Bahadur Hospital, New Delhi, over a period of 15 months from January 2015 to March 2016. The institutional research ethics committee approved the study. After a written and informed consent, each patient with hand eczema, fulfilling the inclusion criteria (clinically established hand eczema in a patient above 16 years of age, willing to undergo patch test),and absence of exclusion criteria (pregnant or breastfeeding and current treatment with systemic immunosuppressive medication) was recruited in the study. As per the predesigned case record form, a detailed comprehensive history about their hand eczema, symptoms, duration, occupational details, aggravating factors, treatment, atopy, sick leaves, recurrence and the total cost of illness in last 12 months (direct and indirect) was elicited. Atopic status of patients was established based on personal or family history of atopy as per Hanifin and Rajka criteria and/or raised serum immunoglobulin E and the presence of atopy stigmata. Direct expenses included medical costs including the cost of prescribed and nonprescribed drugs, transportation cost while indirect expenses covered lost workdays (e.g. sick leave), loss of productivity and the possible need for a change of jobs. Hand eczema severity index and quality of life were assessed using the Dermatology Life Quality Index questionnaire. Laboratory investigations like hemogram, absolute eosinophilic count and serum immunoglobulin E were carried out. After complete clinical examination and recording of details pertaining to the nature, extent and morphology of lesions, the patients were subjected to patch testing. Patch testing was performed after clearance of eczema and withdrawal of therapy with topical steroids and included assessment of the probable relevant contactants in each individual patient. Any cosmetic cream or emollient used by the patient was used during testing. The protocol established by the International Contact Dermatitis Research Group was adopted throughout the study. 5 The antigens used for the procedure included the Indian standard series of 25 antigens and cosmetic series of 43 antigens, which were approved by the Contact and Occupational Dermatosis Forum of India and marketed by Systopic Pharmaceuticals Ltd., India, and other relevant allergens—as per the case history. Homemakers and other patients who reported a history of cooking were also tested with vegetable extract in 1:5 dilution with sterile water (other patients including cooks and vegetable vendors). Patch test reading was taken on Day 2 (48 h) and Day 4 (96 h). It was interpreted using criteria laid down by International Contact Dermatitis Research Group and classified into the following clinical types on the basis of relevant criteria for the classification of chronic hand eczema subtypes: 6
- Allergic contact dermatitis: Positive patch test for relevant allergen and/or allergen avoidance successful in preventing flares and/or presence of eczema spreading
- Irritant contact dermatitis: Excessive contact of hands with water or irritants, either private or occupational
- Atopic hand eczema: A family history of atopy and/or history of atopy (allergic rhinitis or asthma) and/or raised serum IgE and atopy stigmata
- Not specified: When a patient was patch test negative and did not fit into criteria of atopy and no obvious history of wet work[7] or contact with irritant was present
- Allergic contact dermatitis + atopic hand eczema: Patch test positive with relevant antigen either in personal use or workplace along with the personal history of atopy
- Allergic contact dermatitis + irritant contact dermatitis: Patch test positivity with a relevant or correlating antigen along with a history of wet work or contact with known irritants
All statistical analysis was carried out using the Statistical Package for the Social Sciences (SPSS) software version 20.0. The categorical comparison was done by Chi-square/Fischer's test. Nonparametric tests like the Mann–Whitney and Kruskal–Wallis tests were applied to find a correlation between categorical and continuous variables. Spearman's correlation was applied to find the correlation between the continuous variables.
Results
The mean age of the patients with hand eczema was 35.62 (18–64) years with a majority of patients belonging to the age group of 18–47 years (85%). The occupation of the patients inducted in the study included housewives 40 (40%), masons 15 (15%), clerical worker 8 (8%), students 7 (7%), factory workers 5 (5%) and miscellaneous, including hairdresser, painter, health care worker, shopkeeper, electrician, teacher, driver, farmer, vegetable vendor, butcher and tailor.
Clinical presentation
Morphologically, chronic dry fissured eczema was the most common pattern seen in 36 (36%) of patients followed by mixed type (19%), hyperkeratotic palmar eczema (15%), vesicular eczema with recurrent eruption (9%), nummular eczema (7%) and wear and tear dermatitis (7%).
Patch test
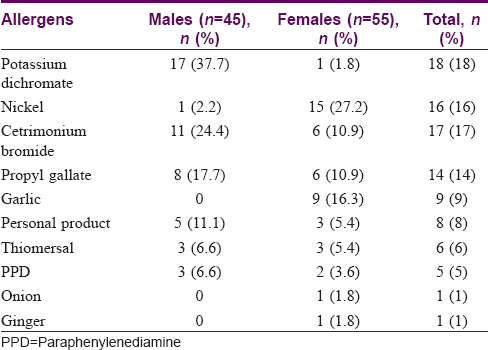
Out of the 100 patch-tested patients, 79 (79%) patients gave positive patch test results [Table - 1], while 21% had a negative result. Potassium dichromate 17 (37.7%) was the most common sensitizer in males, while in females it was nickel 15 (27.2%). A positive response to work-related antigen was found in masons 15 (100%), factory workers 2 (40%), homemakers 21 (52.5%) and clerical workers 2 (25%). Out of the 79 patients with positive patch tests, 23 had hand eczema severity index score of more than 12; 33 had a score between 6 and 12 and 23 had a score less than 6. At the time of statistical analysis, the patch test positivity was found to be marginally correlated with the severity index of hand eczema (P = 0.062). Allergic contact dermatitis was the most common clinical pattern of hand eczema observed in 45 (45%), followed by an irritant contact dermatitis 14 (14%) and a combination of both 13 (13%). Overall, 50 (50%) of the patients had a personal history of atopy, with females (31) outnumbering males (19) and 23 (23%) had a family history of atopy.
Investigations
The average serum immunoglobulin E value was 368.4 ± 267.4, with a median value of 370. However, its values were not found to be correlated with the atopic status of the patients. The average absolute eosinophilic count value was 314 ± 266 (median = 231.50). Surprisingly, again no positive correlation between absolute eosinophilic count and atopy was evident (P = 0.506).
Hand eczema severity index and dermatology life quality index
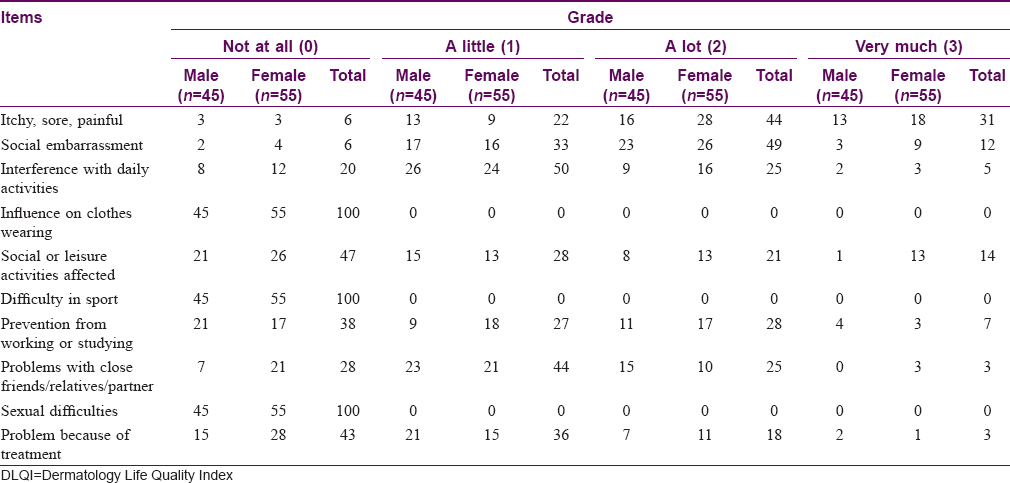
The median value for the hand eczema severity index score was 9.0 (2.0–88). The mean hand eczema severity index score was higher in males as compared with females but was statistically insignificant (P = 0.231). Upon further analysis, after stratifying based on the cutoff values, 33.3% of the males had a hand eczema severity index score of more than 12 compared with 18.2% females (P = 0.216). The average Dermatology Life Quality Index score was 8.18 ± 3.4 (2–22), with no significant difference between males and females (P = 0.231). A highly significant correlation was evident between the Dermatology Life Quality Index and the hand eczema severity index (P = 0.001). As depicted in [Table - 2], the evaluation of subscales of the Dermatology Life Quality Index questionnaire revealed that the items itchy, sore, painful and evaluating social embarrassment were most affected seen among 94 patients of hand eczema, followed by the third item that asked about interference with daily activities (80), enquiring about problems with close friends/relatives/partner (72), asking about prevention from working or studying (62) and the item that addressed problems because of treatment (57). The least affected was the item that evaluated the social or leisure activities affecting 53% of the patients. Social embarrassment because of hand eczema was observed in 94 (94%) of the patients, out of which 49 (52%) being affected a lot and 12 (12.7%) reporting that they were very much affected. Hand eczema caused interference with daily activities in 80 (80%) of the patients.
Cost of illness
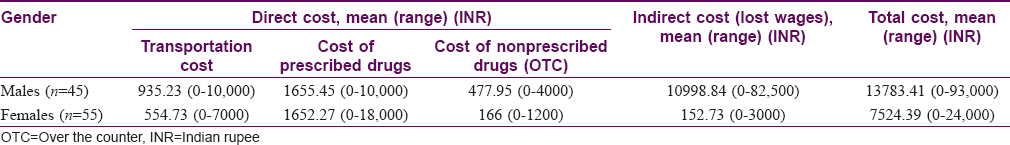
The average total cost of illness was INR 13,783.41 (0–93,000) per individual per year with an average direct cost of INR 2,746.25 ± 1,900 and indirect cost of INR 4911.73 ± 13237.72 [Table - 3]. The direct and indirect costs positively correlated with the Dermatology Life Quality Index (P = 0.00) and the hand eczema severity index. The direct, as well as the indirect cost of illness, increased with higher hand eczema severity index value (P = 0.040, 0.021, respectively). Among the 15 patients working as masons, 11 (73.3%) had a total cost of illness more than INR 5185 per year. Interestingly, a change of occupation attributable to exacerbation of hand eczema was reported by only 3 masons out of the 100 study subjects.
Discussion
In our study, the majority of the females with hand eczema were engaged in household work (72.8%) and males in unskilled work, such as that of a mason, laborer, farmer, factory worker, etc.
Contact sensitization in the present study [79%; [Table - 1] was comparable with Sharma et al.[8] (80%) and Bajaj[9] (80.3%) and much higher than Hald et al.[10] (45.6%) and Handa et al.[11] (65%). The higher frequency of contact sensitization could be attributed to extensive antigen testing of patients in our and some of the previous studies.[12],[13] In our study, potassium dichromate was the most common sensitizer. In addition, it was also the most common sensitizer in males 17 (37.7%) as compared with females 1 (1.8%; P = 0.0001). Cetrimonium bromide, a water-soluble cationic quaternary surfactant, was the second most common sensitizer in our study 17 (17%)—11 (24.4%) in males and 6 (10.9%) in females. The next common sensitizer was nickel sulfate 16 (16%). Interestingly, contact sensitization to gallate was seen in 14 (14%) of our cases—8 (17.7%) males and 6 (10.9%) females. A few Indian[14],[15],[16], as well as Western studies[17],[18], have reported allergic contact dermatitis because of propyl gallate, in the form of depigmentation and/or cheilitis. However, none of them was specific for hand eczema. Therefore, we suggest patch testing of all patients with suspected allergic contact dermatitis with cosmetic series, using their own products like creams or cosmetics, must be carried out to avoid missing this allergen.
Our study attempted to characterize different clinical subtypes. Allergic contact dermatitis 45 (45%) was the most common clinical pattern of hand eczema, followed by allergic contact dermatitis with atopic hand eczema 19 (19%), allergic contact dermatitis with irritant contact dermatitis 13 (13%), atopic hand eczema 7 (7%) and 2% could not be classified into any of the subtypes. Irritant contact dermatitis was significantly more in females13 (23.6%) versus males 1 (2.2%) (P = 0.002), in accordance with a recent Danish study by Diepgen et al.[19] It could be attributed to the impact of domestic wet work.
Contact sensitization in atopic patients is a matter of debate. High prevalence of hand involvement in patients with active atopic dermatitis has been reported by Simpson et al.,[20] while Suman et al. reported a much lower percentage (36%) of atopic patients compared with the present study (50%). In the present study, the difference may be attributed to the evaluation of the history of atopy and childhood eczema, absolute eosinophilic count and serum immunoglobulin E, along with the diagnostic criteria (Hanifin and Rajka), rather than using diagnostic criteria alone as was done in the latter study.
The chronicity and frequent recurrences of hand eczema lead to a massive impact on the quality of life. In an American observational study, 80% of their patients experienced negative psychosocial interference, sleep or mood disturbance, change of daily activities and cessation of hobbies.[2] A single small Indian study of 46 patients concluded that impairment of quality of life was mainly dependent on increased frequency (>4 episodes/year) and not on the hand eczema severity.[21] The Dermatology Life Quality Index is a valid objective tool to measure the quality of life.[22] A positive correlation between it and the hand eczema severity index shows a close relationship between quality of life and disease severity and supports measurement of the Dermatology Life Quality Index as a clinically relevant parameter. Interestingly, hand eczema contributed to reluctance in social and leisure activities in 53 (53%) of the patients, with females 13 (23.6%) getting affected ''very much,'' significantly more (P = 0.002) as compared with males 1 [1.8%; [Table - 2]. However, we could not come across any study comparing grades of subscales with gender or any other parameter.
The cost-of-illness studies identify and measure the monetary estimate of the total burden of a particular disease. These studies are valuable because they give an insight into the factors that contribute to high costs incurred by this often disabling disease, and thereby help in the prevention of the disease or use of effective treatment. Therefore, it is surprising that despite its great medical and socioeconomic importance, there is a paucity of data that addresses the cost of illness and economic factors in chronic hand eczema. Most of the studies have originated in Europe, and have emphasized that the costs associated with chronic hand eczema are affected not only by disease severity but also by the relationship of chronic hand eczema to work (causal and/or affecting work performance).[23] A study involving 10 European dermatology departments found that more than 50% of cases of hand eczema were reported to be work-related chronic hand eczema.[24]
In a questionnaire-based study including 1,238 subjects of hand eczema by Meding et al., 21.4% reported sick leave of a minimum of 7 days on at least one occasion. Cortesi et al.[4] evaluated the cost of illness in patients with severe chronic hand eczema refractory to standard therapy with topical potent corticosteroids by calculating direct (e.g. drug treatment and travel) and indirect (i.e. loss of productivity) mean costs/patient-month. Overall, calculated mean costs turned out to be 418.3 €/patient-month, with a loss of productivity contributing 43.7%, and hospitalization and travel contributing 16.1% and 10.3%, respectively. Diepgen et al.[3] studied the cost of illness in occupational hand eczema patients in which the societal costs associated with occupational hand eczema amounted to 8,799 € per patient, maximally attributable to productivity losses that highlight the impact of hand eczema on work productivity. There was no substantial difference in the costs generated in the preceding 12 months between patients with low and high disease severity at their assessment visit. The average total cost of illness was INR 13,783.41 per individual per year with average direct cost INR 2,746.25 and indirect cost INR 4911.73 in the present study. Direct, as well as indirect costs, have a significant correlation with hand eczema severity index (P = 0.040, 0.021) [Table - 3]. Indirect cost (lost wages) relates more with severity because the more severe the disease, more likely it is to affect the working ability of the patient with hand eczema and lead to absence from work, In addition, significantly, most of the patients in the present study were daily wage workers. Further, the total cost of illness also was highly correlated with the Dermatology Life Quality Index (P = 0.00). The total cost of illness, as well as quality of life, were found to be highly influenced by the history of sick leaves in the past 12 months (P = 0.00, 0.017, respectively), while a change of occupation was reported by only three male masons in our study.
Conclusion
It may be concluded that impaired quality of life and loss of productivity are the most important consequences in patients of hand eczema. Appropriate treatment is necessary to improve patient health and productivity, which will contribute to reducing societal costs. Patch testing should ideally include Indian standard, cosmetic series, plant series, patients own products and other work-related antigens in appropriate dilution. It is imperative to evaluate the quality of life, including subscales to identify the psychosocial impact of the disease. The limitations of our study include the lack of population representation, as this was a hospital-based study; bias toward more chronic disease because of ours being a tertiary, referral center and that the estimation of cost of illness was based on retrospective calculations.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Thyssen JP, Linneberg A, Menné T, Johansen JD. The epidemiology of contact allergy in the general population-prevalence and main findings. Contact Dermatitis 2007;57:287-99.
[Google Scholar]
|
| 2. |
Meding B, Wrangsjö K, Järvholm B. Fifteen-year follow-up of hand eczema: Predictive factors. J Invest Dermatol 2005;124:893-7.
[Google Scholar]
|
| 3. |
Diepgen TL, Scheidt R, Weisshaar E, John SM, Hieke K. Cost of illness from occupational hand eczema in Germany. Contact Dermatitis 2013;69:99-106.
[Google Scholar]
|
| 4. |
Cortesi PA, Scalone L, Belisari A, Bonamonte D, Cannavò SP, Cristaudo A, et al. Cost and quality of life in patients with severe chronic hand eczema refractory to standard therapy with topical potent corticosteroids. Contact Dermatitis 2014;70:158-68.
[Google Scholar]
|
| 5. |
Wilkinson DS, Fregert S, Magnusson B, Bandmann HJ, Calnan CD, Cronin E, et al. Terminology of contact dermatitis. Acta Derm Venereol 1970;50:287-92.
[Google Scholar]
|
| 6. |
Molin S, Diepgen TL, Ruzicka T, Prinz JC. Diagnosing chronic hand eczema by an algorithm: A tool for classification in clinical practice. Clin Exp Dermatol 2011;36:595-601.
[Google Scholar]
|
| 7. |
Anveden Berglind I, Alderling M, Järvholm B, Lidén C, Meding B. Occupational skin exposure to water: A population-based study. Br J Dermatol 2009;160:616-21.
[Google Scholar]
|
| 8. |
Sharma VK, Kaur S. Contact dermatitis of hands in Chandigarh. Indian J Dermatol Venereol Leprol 1987;53:103-7.
[Google Scholar]
|
| 9. |
Bajaj AK. Contact dermatitis hands. Indian J Dermatol Venereol Leprol 1983;49:195-9.
[Google Scholar]
|
| 10. |
Hald M, Agner T, Blands J, Veien NK, Laurberg G, Avnstorp C, et al. Clinical severity and prognosis of hand eczema. Br J Dermatol 2009;160:1229-36.
[Google Scholar]
|
| 11. |
Handa S, Kaur I, Gupta T, Jindal R. Hand eczema: Correlation of morphologic patterns, atopy, contact sensitization and disease severity. Indian J Dermatol Venereol Leprol 2012;78:153-8.
[Google Scholar]
|
| 12. |
Raghu MT, Karinagannanavar A, Parvathi CN. A study of clinical types of contact allergic dermatitis of hands and its association with allergens. Int J Appl Res 2015;1:643-50.
[Google Scholar]
|
| 13. |
Kishore NB, Belliappa AD, Shetty NJ, Sukumar D, Ravi S. Hand eczema-clinical patterns and role of patch testing. Indian J Dermatol Venereol Leprol 2005;71:207-8.
[Google Scholar]
|
| 14. |
Pandhi D, Vij A, Singal A. Contact depigmentation induced by propyl gallate. Clin Exp Dermatol 2011;36:366-8.
[Google Scholar]
|
| 15. |
Athavale NV, Srinivas CR. Contact cheilitis from propyl gallate in lipstick. Contact Dermatitis 1994;30:307.
[Google Scholar]
|
| 16. |
Kanthraj GR, Shenoi SD, Srinivas CR. Patch testing in contact cheilitis. Contact Dermatitis 1999;40:285.
[Google Scholar]
|
| 17. |
Gamboni SE, Palmer AM, Nixon RL. Allergic contact stomatitis to dodecyl gallate? A review of the relevance of positive patch test results to gallates. Australas J Dermatol 2013;54:213-7.
[Google Scholar]
|
| 18. |
Marston S. Propyl gallate on liposomes. Contact Dermatitis 1992;27:74-6.
[Google Scholar]
|
| 19. |
Diepgen TL, Andersen KE, Brandao FM, Bruze M, Bruynzeel DP, Frosch P, et al. Hand eczema classification: A cross-sectional, multicentre study of the aetiology and morphology of hand eczema. Br J Dermatol 2009;160:353-8.
[Google Scholar]
|
| 20. |
Simpson EL, Thompson MM, Hanifin JM. Prevalence and morphology of hand eczema in patients with atopic dermatitis. Dermatitis 2006;17:123-7.
[Google Scholar]
|
| 21. |
Charan UP, Peter CV, Pulimood SA. Impact of hand eczema severity on quality of life. Indian Dermatol Online J 2013;4:102-5.
[Google Scholar]
|
| 22. |
Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI) – A simple practical measure for routine clinical use. Clin Exp Dermatol 1994;19:210-6.
[Google Scholar]
|
| 23. |
Augustin M, Kuessner D, Purwins S, Hieke K, Posthumus J, Diepgen TL. Cost-of-illness of patients with chronic hand eczema in routine care: Results from a multicentre study in Germany. Br J Dermatol 2011;165:845-51.
[Google Scholar]
|
| 24. |
Diepgen TL, Purwins S, Posthumus J, Kuessner D, John SM, Augustin M. Cost-of-illness analysis of patients with chronic hand eczema in routine care in Germany: Focus on the impact of occupational disease. Acta Derm Venereol 2013;93:538-43
[Google Scholar]
|
Fulltext Views
3,850
PDF downloads
1,225





