Translate this page into:
A curious case of solitary black nail
Corresponding author: Dr. Shekhar Neema, Department of Dermatology, Base Hospital, Lucknow, Uttar Pradesh, India. shekharadvait@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Neema S, Pathania V, Tripathi A, Kothari R, Singh V, Singh A. A curious case of solitary black nail. Indian J Dermatol Venereol Leprol. 2025;91:S90-S91. doi: 10.25259/IJDVL_1028_2024
A 51-year-old man, presented with progressive blackish discolouration and dystrophy of right index fingernail of 8-years duration. There was no history of trauma, animal handling or gardening. There was no history of discharge or itching. Dermatological examination revealed diffuse, mildly tender swelling involving the distal part of the right index finger. The overlying nail plate was hyperpigmented, dystrophic and friable. Hyperpigmentation also involved proximal nail fold, hyponychium and periungal areas (positive Hutchinson’s sign) [Figure 1]. Dermoscopy showed longitudinal melanonychia involving the entire nail. It was variegated in colour with longitudinal splitting of nail plate and grey to black pigment network in periungual and subungual skin [Figure 2]. Nail matrix biopsy showed normal epidermis with increase in basal melanin pigment, with dermis showing a mildly cellular mesenchymal lesion on a dense collagenous background. The cells were arranged as intersecting fascicles displaying oval to spindle shape with bland nuclei, fine chromatin, occasional prominent nucleoli and moderate amount of eosinophilic cytoplasm. Immunohistochemistry showed tumour cells to be positive for vimentin and focal S100, negative for Human Melanoma Black - 45 (HMB 45).
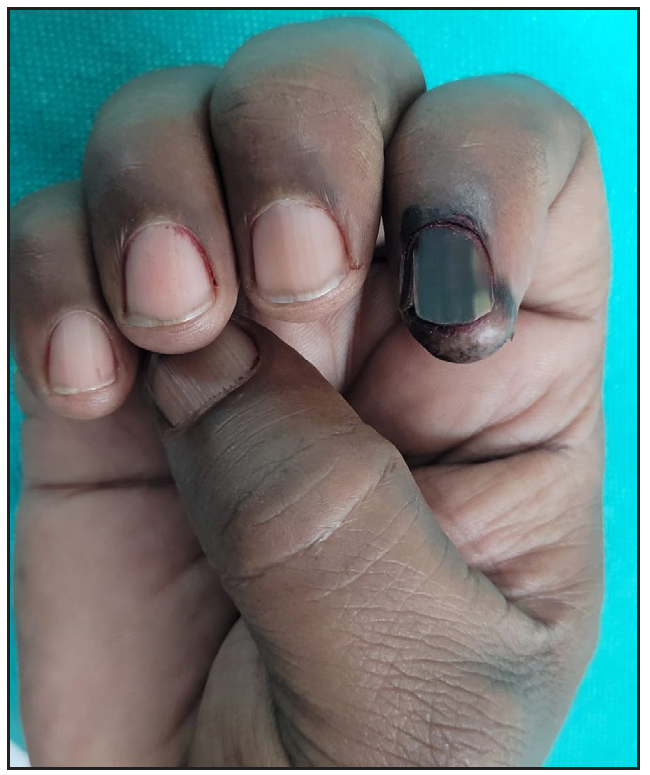
- Hyperpigmented, dystrophic and friable nail plate with hyperpigmentation of proximal nail fold, hyponychium and periungual areas.
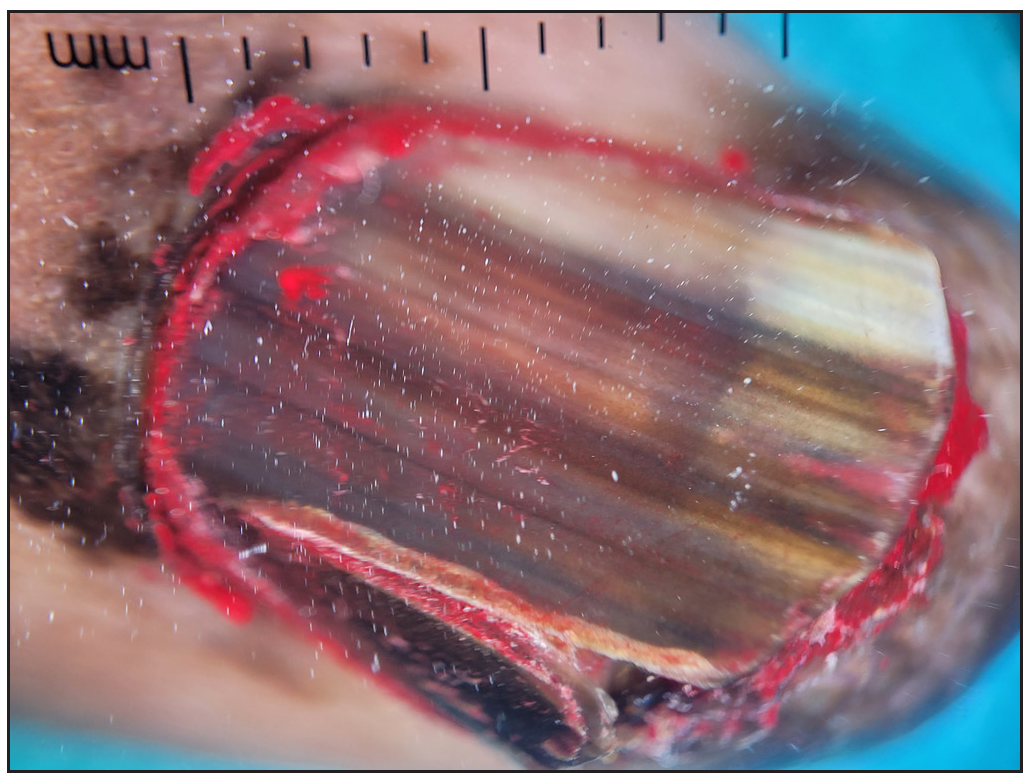
- Longitudinal pigmented band involving>2/3rd of the nail, variegated in colour with longitudinal splitting of the nail plate. Reticular pigment network involving proximal nail fold.
Sry - related HMg - Box gene 10 (SOX 10) and CD34; Ki 67 was < 1% [Figures 3a-3f]. Systemic examination and investigations such as chest radiograph, abdominal ultrasonography (USG) and positron emission tomography (PET) scan were within normal limits.
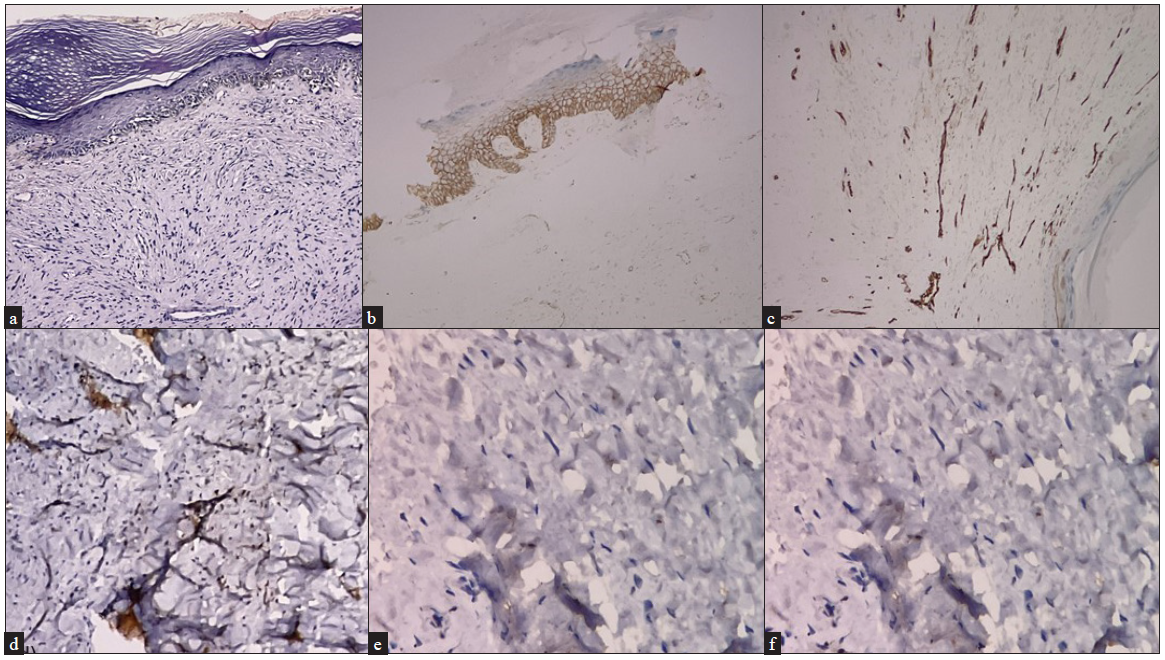
- Nail matrix biopsy showing, (a) spindle cell tumour arranged in intersecting fascicles with interspersed thin-walled capillaries (Haematoxylin and eosin, 200x), (b) negative Immunohistochemistry (IHC) for Pan CK (cytokeratin) 200x, (c) negative CD34 (IHC 200x), (d) negative S-100 (IHC 200x), (e) positive beta-catenin IHC straining (200x) and (f) <1% Ki67 IHC stain positivity (200x)
Question
What is the diagnosis?
Answer
Diagnosis: Benign Myofibroblastic Tumour
Inflammatory myofibroblastic tumours (IMT) are rare neoplasms of intermediate malignant potential. They generally present as soft tissue masses in the abdomino-pelvic region and rarely in the head and neck, bladder, female genitalia, lung and central nervous system. Primary cutaneous IMT is very uncommon. It presents as painless, slowly enlarging, erythematous nodule or plaque.1A review of 18 cases of cutaneous IMT reported the median age of presentation being 33 years, more common in males and most lesions being located on extremities and trunk.2 The differential diagnosis is wide and includes dermatofibroma, melanoma, squamous cell carcinoma, atypical fibroxanthoma or fibrous histiocytoma. Surgical excision is the treatment of choice and recurrence is uncommon. To the best of our knowledge, primary cutaneous IMT involving the nail unit has not been reported so far. It may present as longitudinal melanonychia and arouse suspicion of subungual melanoma. The dermoscopic features of subungual melanoma are wide pigmented band, variegated colour, nail dystrophy and Hutchinson’s sign.3 The present case showed dermoscopic features suggestive of subungual melanoma. The presence of spindle cells on histopathology and characteristic dermoscopic features suggested a differential diagnosis of spindle cell melanoma or desmoplastic melanoma. A complete set of IHC including SOX 10 and CD 34 for desmoplastic and spindle cell melanoma respectively aided in a final diagnosis of benign myofibroblastic tumour.4,5
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Cutaneous inflammatory myofibroblastictumor with CARS-ALK fusion: Case report and literature review. J CutanPathol. 2022;49:795-801.
- [Google Scholar]
- Cutaneous inflammatory myofibroblastic tumour: A case report and literature review. Eur J Dermatol. 2017;27:676-7.
- [CrossRef] [PubMed] [Google Scholar]
- Melanonychia - Clues for a correct diagnosis. Cureus. 2020;12:e6621.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- SOX10 expression distinguishes desmoplastic melanoma from its histologic mimics. Am J Dermatopathol. 2013;35:576-81.
- [CrossRef] [PubMed] [Google Scholar]
- Neurofibroma-like spindle cell melanoma: CD34 fingerprint and CGH for diagnosis. Am J Dermatopathol. 2012;34:668-70.
- [CrossRef] [PubMed] [Google Scholar]






