Translate this page into:
A life-threatening consequence of erythema nodosum leprosum
Corresponding author: Prof. Sukhjot Kaur, Department of Dermatology, Dayanand Medical College and Hospital, Ludhiana, Punjab, India. sukhjotgoraya@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Malhi K, Singla L, Singh A, Kaur S. A life-threatening consequence of erythema nodosum leprosum. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_18_2024
Dear Editor,
Leprosy is a chronic infectious disease complicated by immune-mediated lepra reactions. Erythema nodosum leprosum (ENL) is a type III hypersensitivity reaction resulting in polymorphic cutaneous features and frequent systemic complications, including secondary haemophagocytic lymphohistiocytosis (HLH).1 Secondary HLH and ENL result from intricate interactions between Mycobacterium leprae and host immune response, forming a continuum.1 HLH in ENL is rare despite similar pathophysiology with very few documented case reports.1–4
A 23-year-old man presented in the emergency with recurring fevers and sudden onset of raised reddish lesions on his upper and lower limbs. About a month earlier, he had a similar episode that resolved spontaneously. On examination, he appeared disoriented with tachycardia, tachypnoea, pallor, and pitting pedal oedema. His face showed diffuse infiltration with supraciliary madarosis [Figure 1a] and ear lobes infiltration. His palms and soles exhibited multiple discrete dusky purpuric macules and papules with central necrosis [Figure 1b]. In addition, there was diffuse, non-tender erythematous swelling on both hands with right-sided ulnar clawing [Figure 1c]. Peripheral nerve examination revealed rope-like enlargement of the bilateral ulnar, radial cutaneous, popliteal and right median nerves. Due to altered sensorium, sensory testing was deferred. A slit skin smear from the ear lobes revealed acid-fast bacilli with a bacterial index of 6+. Histopathological examination showed lymphocytic and neutrophilic infiltrate and foamy macrophages laden with acid-fast bacilli [Figure 2a] along with leukocytoclasia and extravasation of the RBCs giving the impression of vasculonecrotic ENL [Figure 2b]. Zeihl–Neelsen stain demonstrated abundant acid-fast bacilli in globi [Figure 2c]. Further investigations revealed anaemia (Hb: 8.3 g/dL), leukopenia (2.34 * 103/μL), thrombocytopenia (80*103/μL), transaminitis (SGOT – 732 U/L; SGPT – 271 U/L), elevated triglycerides (639 mg/dL) and ferritin (2000 ng/mL). High-resolution CT showed consolidation in the right lower lobe and mild bilateral pleural effusion. Abdominal ultrasound indicated splenomegaly (bipolar diameter = 15.7 cm). Blood and urine cultures were negative and Mycobacterium tuberculosis PCR from bronchoalveolar aspirate ruled out tubercular aetiology.

- Diffuse infiltration of the face with supraciliary madarosis.

- Multiple, discrete, dusky purpuric macules and papules with central necrosis over palms and soles.

- Diffuse non-pitting edema appreciated over hands with ulnar clawing appreciated on the right side (black arrow) and overlying discrete punched-out ulcers with central vasculonecrotic changes.
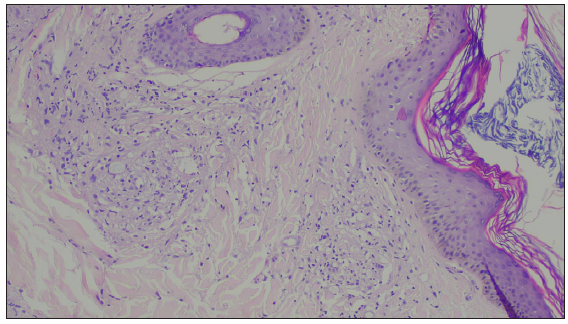
- Epidermal atrophy with diffuse dermal lymphocytic and neutrophilic infiltrate and foamy macrophages laden with acid-fast bacilli, consistent with lepromatous leprosy with ENL (Haematoxylin and eosin, 400×).
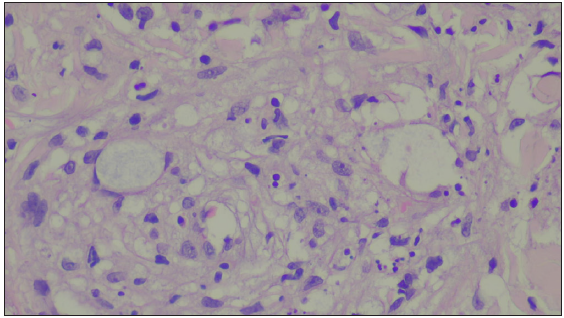
- Leukocytoclasia and extravasation of the RBCs, consistent with vasculonecrotic ENL (Haematoxylin and eosin, 400×).
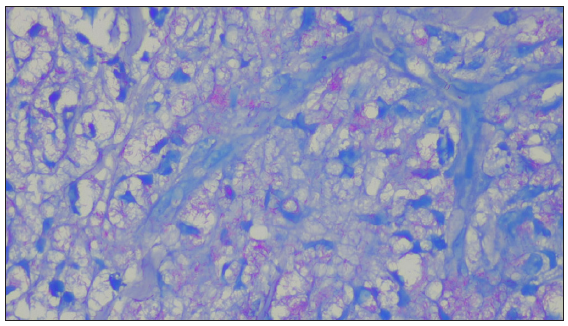
- Abundant acid-fast bacilli seen inside the dermal macrophages (Ziehl-Neelsen stain (5%), 1000×).
The patient was managed with oxygen support, intravenous fluids, and antibiotics (piperacillin-tazobactam) to manage worsening oxygen saturation and hypotension. Due to liver and kidney parameters derangement, initiation of active anti-leprosy treatment was delayed. The patient satisfied the 2009 HLH criteria with four clinical features (fever, splenomegaly, bicytopenia, and hepatitis) and one immune criterion (hyperferritinaemia).5 Considering the possibility of secondary HLH with vascular-necrotic ENL, the patient received intravenous steroid pulse therapy (methylprednisolone 2–4 mg/kg/dose for 2 days), followed by maintenance hydrocortisone. Haematological, liver, and kidney parameters improved with treatment and have been summarised in Table 1. Subsequently, patient was started on alternate anti-leprosy therapy (minocycline, ofloxacin, clofazimine) due to intolerance to World Health Organisation-MultiDrug Therapy (WHO-MDT) - Rifampicin and Dapsone with recurrent transaminitis (serum alanine aminotransferase – 552 IU/L; serum aspartate aminotransferase – 220 IU/L) and gastric distress. The patient was also subsequently started on thalidomide 100 mg thrice daily for managing ENL.
| Parameters | Reference values | Day 1 | Day 7 (post intravenous methylprednisolone) | Day 14 (post- intravenous methylprednisolone) |
|---|---|---|---|---|
| CBC | ||||
| Haemoglobin(g/dL) | 12-16 g/dL | 8.3 | 9.1 | 11.0 |
| TLC (/µL) | 4-11 x 103/ µL | 2.340 x 103 | 5.7 x 103 | 6.6 *103 |
| DLC (N/L/M/E/B) [*103/µL] | 150-450 x 103/ µL | 1.97/0.25/0.12/ 0/.02 | 3.85/0.68/0.59/0/0.002 | 5.93/0.19/0.48/0/0.001 |
| Platelet count (/µL) | 80 x 103 | 236 x103 | 199 *103 | |
| Liver function tests | ||||
| Total bilirubin (mg/dL) | 0.1-1.2 mg/dL | 3.67 | 1.23 | 1.1 |
| Conjugated bilirubin (mg/dL) | 0.3 mg/dL | 2.46 | 0.42 | 0.26 |
| SGOT (IU/L) | 0-40 IU/L | 732 | 149 | 42 |
| SGPT (IU/L) | 0-40 IU/L | 271 | 164 | 56 |
| Electrolytes | ||||
| Serum sodium (mmol/L) | 135-146 | 142 | 144 | 139 |
| Serum potassium (mmol/L) | 3.5-5 | 3.12 | 3.14 | 4.56 |
| Serum chloride (mmol/L) | 96-106 | 106 | 105 | 102 |
| Kidney function tests | ||||
| Serum urea (mg/dL) | 5-20 mg/dL | 44.0 | 25.0 | 23.0 |
| Serum creatinine (mg/dL) | 0.7-1.3 mg/dL | 0.69 | 0.41 | 0.45 |
| Serum triglycerides (mg/dL) | 159mg/dL | 639 | - | - |
| Serum ferritin (ng/mL) | 30-400 ng/mL | 2000 | - | - |
| Serum LDH (U/L) | 140-280 U/L | 1769 | - | - |
CBC, Complete blood counts; DLC, Differential leukocyte counts; LDH, Lactate dehydrogenase; SGOT, Serum glutamic-oxaloacetic transaminase; SGPT, Serum glutamic pyruvic transaminase; N/L/M/E/B, neutrophil/lymphocyte/monocyte/eosinophil/basophil; TLC, Total leukocyte counts.
ENL typically manifests with fleeting papulo-nodular eruptions and systemic complications like secondary HLH.1–4 Secondary HLH can be triggered by heightened CD8+ T-cell reactions to various viruses like Epstein–Barr virus (EBV) and cytomegalovirus (CMV) and bacterial, fungal or parasitic infections, or autoimmune disorders like lupus erythematosus.5 Symptoms of HLH encompass fever (the most common, occurring in 100% of cases), organ enlargement, neurological dysfunction, oedema, and liver abnormalities.5 Treatment for HLH typically involves systemic corticosteroids, commonly dexamethasone, as the cornerstone.6 In severe cases, therapies such as the etoposide-based HLH-94 and HLH-2004 protocols are employed.6 The initial phase of these protocols consists of daily dexamethasone dosing, ranging from 10 mg/m2 per day for weeks 1–2 to 1.25 mg/m2 per day for week 7 with subsequent tapering in week 8. Etoposide (VP-16) is also administered at 150 mg/m2 twice weekly for weeks 1–2, then once weekly after that.6 Differentials diagnosis of dapsone hypersensitivity syndrome, typically emerging within a few weeks after initiating MDT, was ruled out as the patient had not yet begun MDT. Sepsis with multiorgan dysfunction syndrome was also considered due to the multiorgan involvement and resistant shock but negative body fluid cultures negated this possibility. Cardiac, respiratory, and hepatic involvement may be observed in ENL even without concurrent HLH.7 Cardiac complications, such as wave changes, bundle branch block, QT prolongation and granulomatous deposits, may lead to cardiogenic shock.7 Respiratory issues, though infrequent, might present as lung parenchymal nodules. Hepatic transaminitis with granulomatous infiltration requires timely recognition for appropriate management. Our case represents a rare occurrence of ENL coexisting with HLH and vasculitic cutaneous lesions, an unprecedented finding. This highlights the crucial need for recognising and managing systemic complications associated with ENL to ensure the optimal patient outcome.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- A case of leprosy, erythema nodosum leprosum, and hemophagocytic syndrome: A continuum of manifestations of same agent-host interactions. Intractable Rare Dis Res. 2017;6:230-33.
- [CrossRef] [PubMed] [Google Scholar]
- A rare and challenging case of haemophagocytic lymphohistiocytosis in a patient of leprosy with recurrent erythema nodosum leprosum. Indian J Lepr. 2020;92:285-91.
- [Google Scholar]
- hemophagocytic lymphohistiocytosis in erythema nodosum leprosum: Case report of an unusual conundrum. Indian Dermatol Online J. 2022;13:778-80.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Hemophagocytic lymphohistiocytosis: An update on pathogenesis, diagnosis, and therapy. Best Pract Res Clin Rheumatol. 2020;34:101515.
- [CrossRef] [PubMed] [Google Scholar]
- Confirmed efficacy of etoposide and dexamethasone in HLH treatment: Long-term results of the cooperative HLH-2004 study. Blood. 2017;130:2728-38.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Lymph node abscess and cardiac involvement in a patient with nodular lepromatous leprosy (LL) with erythema nodosum leprosum (ENL): A rare occurrence. Lepr Rev. 2015;86:112-6.
- [PubMed] [Google Scholar]





