Translate this page into:
A patch of alopecia on chin
2 Departments of Pathology, K. S. Hegde Medical Academy, Deralakate, Mangalore 574 160, Karnataka, India
Correspondence Address:
Manjunath M Shenoy
Department of Dermatology, K. S. Hegde Medical Academy, Deralakate, Mangalore - 574 160, Karnataka
India
| How to cite this article: Shenoy MM, Girisha B S, Teerthanath S. A patch of alopecia on chin. Indian J Dermatol Venereol Leprol 2006;72:179-181 |
 |
 |
 |
 |
 |
 |
A 16-year-old boy presented with a patch of hair loss on his chin region since 6 months. He gave history of having had an itchy elevated lesion, which gradually led to the formation of the present hairless patch. He was given an antifungal cream for application by a medical practitioner, which he had been applying since 1½ months without any improvement.
Examination revealed an otherwise healthy adolescent boy with a single, oval, indurated plaque with sparse hairs compared to the surrounding skin [Figure - 1]. Minimal scaling and faint erythema were evident on closer examination. Tactile sensations were preserved over the lesion.
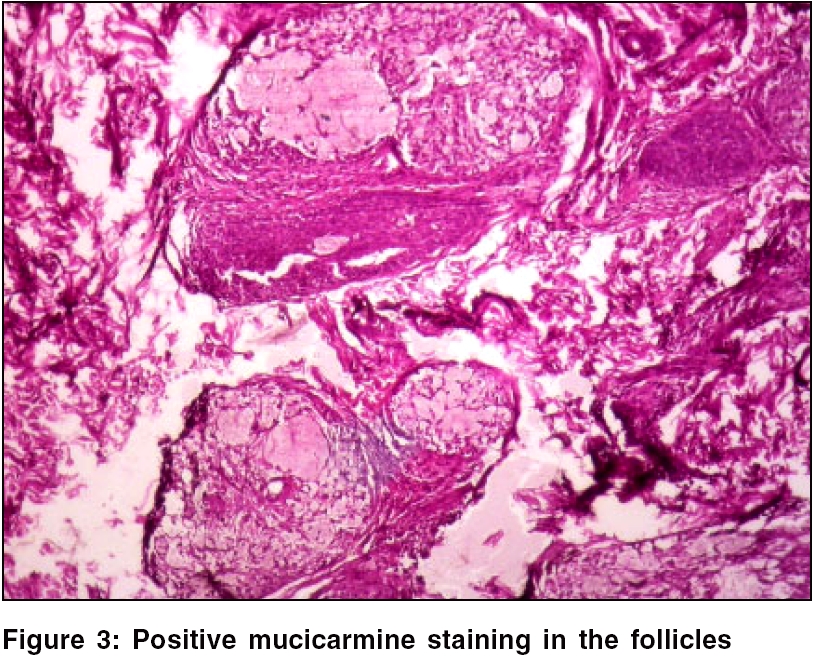
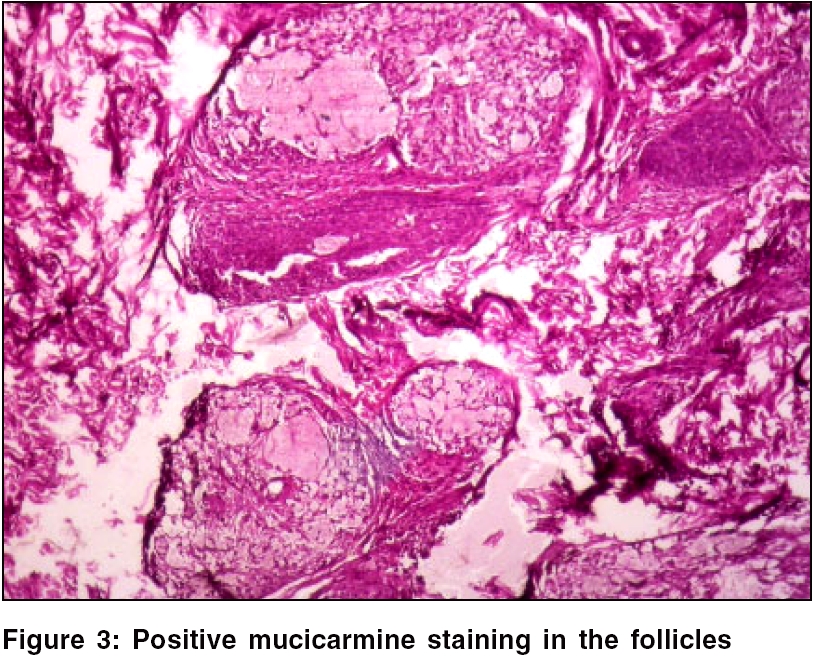
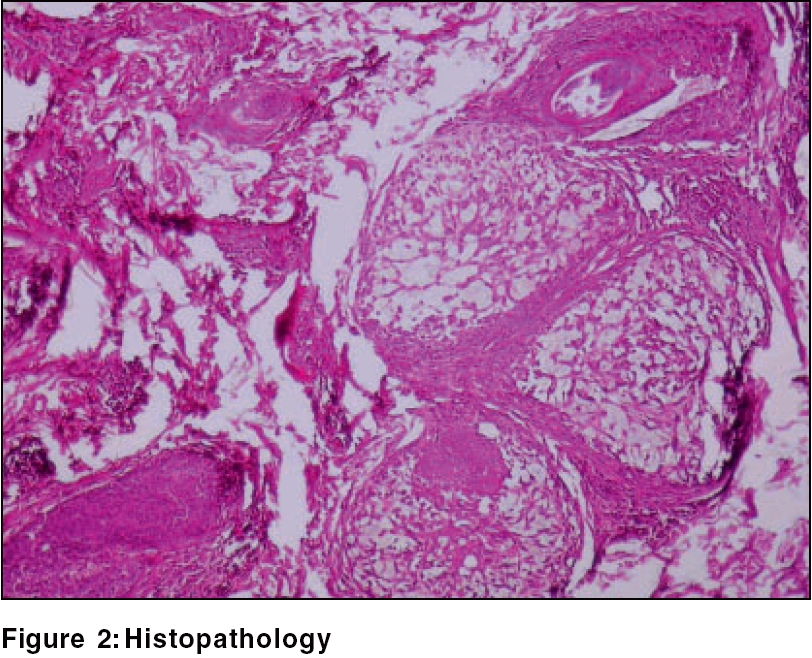
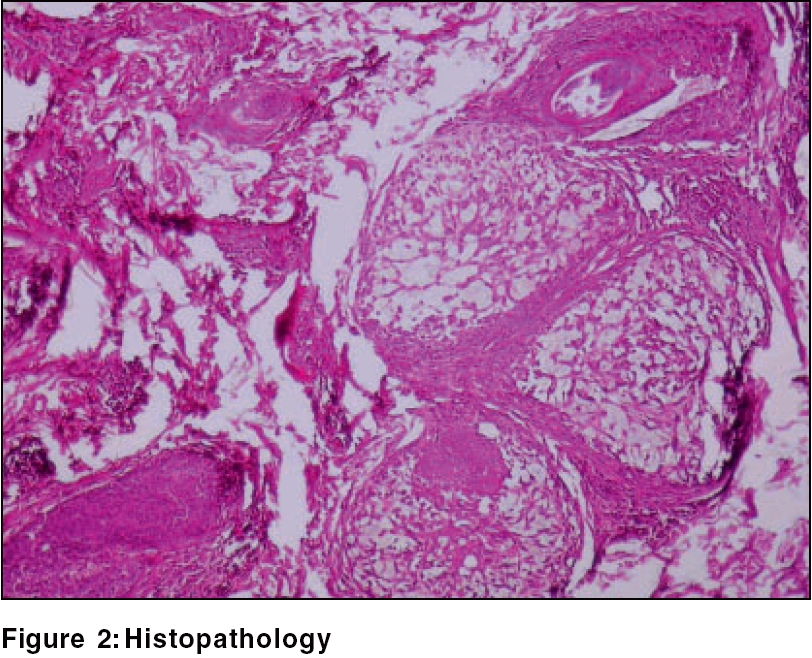
Complete blood count, ESR, urine analysis reports were normal. Scraping for fungal elements was negative. Histopathology from the margin of the lesion is shown in [Figure - 2][Figure - 3].
What is your diagnosis?
Diagnosis: Alopecia mucinosa (follicular mucinosis) Histopathology revealed a normal epidermis with vacuolar changes of the outer root sheath and sebaceous gland epithelium. Mucin was demonstrable within follicular infundibular epithelium and the same was confirmed by mucicarmine staining. There was perifollicular infiltration of lymphocytes and eosinophils. No atypical cells or granuloma were noticed. These findings along with the clinical presentation pointed to a diagnosis of alopecia mucinosa.
Discussion
Alopecia mucinosa consists of follicular papules and/or indurated plaques that demonstrate distinctive histopathologic changes in the hair follicles that lead to the clinically apparent hair loss. Pinkus first reported alopecia mucinosa in 1957.[1] Accumulation of mucinous material in the damaged hair follicles and sebaceous glands is associated with an inflammatory condition and subsequent hair loss. The face, the neck and the scalp are the most frequently affected sites, although lesions may appear on any part of the body.[1] Cutaneous lesions consist of grouped skin-colored papules or erythematous plaques with scaling. Mucin can be squeezed out at times. Indurated scaly plaques and patchy alopecia with sensory impairment may resemble leprosy in many cases.[2]
The three clinical variants of the disease consist of a primary acute disorder of young persons, a primary chronic disorder of older persons and a secondary disorder associated with benign or malignant disease.[1] The primary disorder of young persons consists of focal cutaneous lesions with limited progression and spontaneously resolves between 2 months and 2 years. Primary chronic alopecia mucinosa of older persons affects people older than 40 years. Lesions have a widespread distribution and they may persist or recur indefinitely. No associated disorders are identified. The secondary alopecia mucinosa may be associated with either benign disease or malignant disease. Benign diseases include the inflammatory conditions like lupus erythematosus, lichen simplex chronicus, leprosy, alopecia areata and angiolymphoid hyperplasia.[1],[3] Secondary alopecia mucinosa is also associated with malignant disease, including mycosis fungoides, Kaposi′s sarcoma and Hodgkin disease.[1]
Criteria previously reported to differentiate primary type from lymphoma-associated alopecia mucinosa have proved ineffective. Location on the head and neck region was common in both primary and lymphoma-associated types, but the latter had lesions also on other body sites. In fact, solitary lesions at presentation were common in patients with idiopathic type (68.8%) but uncommon in those with lymphoma-associated alopecia mucinosa (7.1%).[4]
Our patient was a young male with slowly progressing solitary lesion of alopecia mucinosa without any associated benign or malignant diseases, thus fitting into the primary disorder of young persons. Although the question of whether alopecia mucinosa is a transitional state evolving into mycosis fungoides is unresolved, it is proven that alopecia mucinosa may precede the development of mycosis fungoides by several years. Long-term follow-up is crucial in all variants of alopecia mucinosa. He was treated with topical fluticasone propionate cream and was advised monthly follow-up.
| 1. |
Alopecia mucinosa. Gerstner GL, Lebwohl MG. Last updated 12th May 2005.http://www.emedicine.com/DERM/topic15.htm Last accessed 24th July 2005.
[Google Scholar]
|
| 2. |
Kumar B. Metabolic disorders. In: Valia RG, AG Valia, editor. IADVL Text book and atlas of dermatology. 1st ed. Bhalani Publishing House: Mumbai; 1994. p. 901-37.
[Google Scholar]
|
| 3. |
Edward A. Inflammatory diseases of the epidermal appendages and of cartilage. In: Elder D, Elenitsas R, Jaworsky C, Johnson Jr B, editors. Lever's Histopathology of the Skin. 8th ed. Lippincott-Raven: Philadelphia; 1997. p. 403-21.
[Google Scholar]
|
| 4. |
Cerroni L, Fink-Puches R, Bδck B, Kerl H. Follicular mucinosis: A critical reappraisal of clinicopathologic features and association with mycosis fungoides and Sιzary syndrome. Arch Dermatol 2002;138:182-9.
[Google Scholar]
|
Fulltext Views
3,198
PDF downloads
3,687





