Translate this page into:
A patient with diffuse oedema of the eyelids, infraorbital area and indurated plaques over the scalp
Corresponding author: Dr. Indukooru Subrayalu Reddy, A-8 Anand Sheel Enclave, Nandi Nagar, Road Number 14 Banjara Hills, Hyderabad - 500 034, Telangana, India. drreddyis@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Reddy IS, Somani VK, de Padua M, Gowrishankar S. A patient with diffuse oedema of the eyelids, infraorbital area and indurated plaques over the scalp. Indian J Dermatol Venereol Leprol 2023;89:436-8.
A 65-year-old man presented with asymptomatic, indurated swelling of the eyelids and infraorbital area for eight months. Patient first noticed puffiness of eyelids and infraorbital areas, which progressively increased, followed by development of areas of induration over the scalp. Patient denied any preceding skin lesions over the face and scalp. He did not receive radiotherapy or chemotherapy in the past. The extent and degree of induration of eyelids progressively increased, resulting in impaired vision [Figure 1]. Patient first noticed puffiness of eyelids and infraorbital areas, which progressively increased, followed by development of areas of induration over the scalp. Patient denied any preceding skin lesions over the face and scalp. He did not receive radiotherapy or chemotherapy in the past. Two months later, the patient developed a well-delineated indurated plaque over the vertex of scalp with the surrounding area showing diffuse, brawny induration. There were discrete, hyperpigmented, follicular papules coalescing to form an indurated plaque over the left side of vertex [Figure 2]. Patient denied having any preceding skin lesions over the face and the scalp and not received radiotherapy nor chemotherapy in the past. No bleeding or ulceration was noted over the lesion. The posterior cervical and submental lymph nodes were enlarged, painless and firm to hard in consistency.
Skin biopsies were taken from the indurated plaque over the vertex and the left infraorbital area. Both the samples showed similar histopathology. The epidermis was unremarkable. The deep dermis showed prominent, dilated, irregular vascular channels of varying calibre [Figure 3]. The endothelial cells lining the vascular channels were atypical, plump and spindle shaped with hyperchromatic nuclei [Figure 4]. The high-power view showed neoplastic cells arranged in sheets exhibiting enlarged, pleomorphic and vesicular nuclei with scanty to moderate amount of cytoplasm and mitotic activity [Figure 5]. Immunohistochemistry with CD31 showed strong positivity of neoplastic cells through the entire thickness of the dermis [Figure 6].
Question
What is your diagnosis?

- Oedema of eyelids and infraorbital area, more pronounced over the right side

- Indurated plaque over the vertex, with surrounding area of brawny induration and hyperpigmented, indurated plaque over the left occipital area
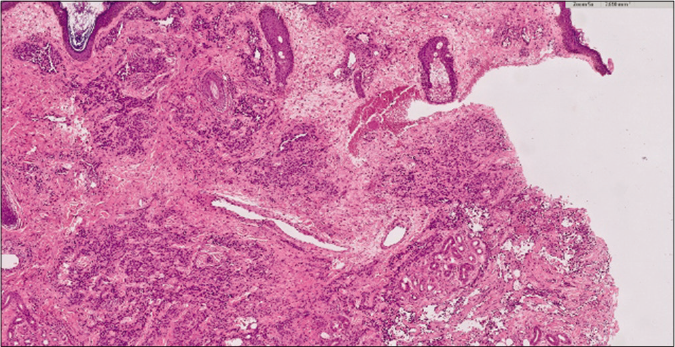
- Epidermis is normal. Deep dermis dermis shows prominent, dilated, irregular vascular channels of varying calibre (H&E ×5)
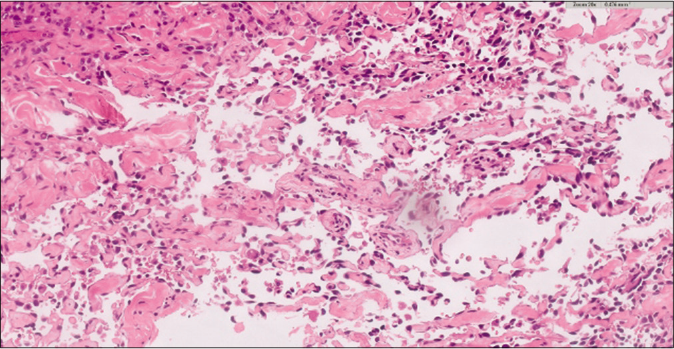
- Dermis showing meshwork of anastomosing, dilated blood vessels. The blood vessels are lined by crowded, atypical endothelial cells with enlarged, hyperchromatic nuclei (H&E ×20)
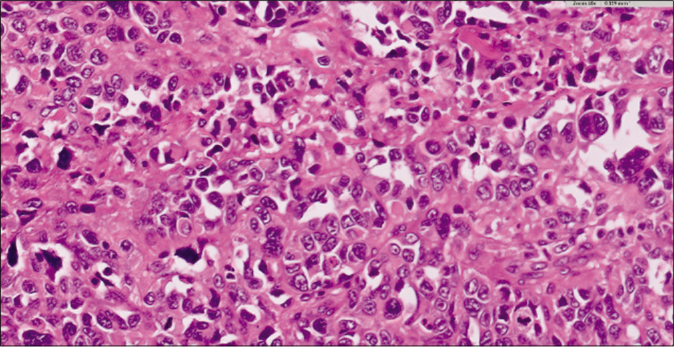
- Neoplastic cells are arranged in sheets and exhibit enlarged, pleomorphic, vesicular nuclei with moderate to scanty cytoplasm and mitotic figures (H&E ×40)

- Neoplastic cells are positive for CD31 (IHC ×10)
Answer
Idiopathic cutaneous angiosarcoma of the head and neck
Discussion
Angiosarcoma was first described by Wilson Jones in 1964 as a malignant angioendothelioma.1 It is a rare, malignant, mesenchymal tumour of vascular origin involving the face and scalp. There are three main clinicopathological subtypes of cutaneous angiosarcoma with an overall incidence of approximately 0.01/100,000 affecting primarily adult patients.2,3 The three clinicopathological subtypes are as follows: idiopathic cutaneous angiosarcoma of the head and neck, angiosarcoma complicating lymph edema (Stewart-Trevis syndrome) and post-irradiation angiosarcoma.
Rarely, angiosarcomas can occur sporadically in patients with xeroderma pigmentosum, epidermolysis bullosa, vinyl chloride disease, in gouty tophus, in renal transplant recipients and in patients with AIDS.
This patient falls in the category of the first type, namely, idiopathic cutaneous angiosarcoma of the head and neck. This typically affects patients in the seventh to ninth decades of life, more common in males with male-to-female ratio of 2.5:1. It commonly involves the upper part of the face and scalp.4 It usually presents as bruise-like patches, single or multiple reddish or purple papules, nodules and plaques. Ulceration and bleeding from the lesions is rarely observed. Exclusive periorbital involvement is occasionally observed.5 Very rarely, angiosarcoma can present as recurrent angioedema.6 The other rare presentations are rosacea-like eruption and rhinophyma-like lesions.7 Early lesions of angiosarcoma need to be differentiated from ecchymoses, port-wine stain and early Kaposi sarcoma.
The histopathology is similar in all three types of angiosarcoma.8 The tumour is poorly circumscribed, multifocal, involving the dermis and subcutaneous fat. The tumour shows an angiomatous and solid pattern. The angiomatous areas show a meshwork of anastomosing dilated blood vessels, permeating between the dermal collagen bundles (dissection of collagen). The vessels are lined by crowded endothelial cells with large, hyperchromatic nuclei. Solid areas show poorly differentiated tumor cells which are spindle shaped to polygonal. Focal epithelioid change is rarely observed.
All forms of angiosarcoma carry a poor prognosis. In one series, only 15% of patients survived for five years after the diagnosis.9 A retrospective study of angiosarcoma of the scalp and face showed an improved five-year survival rate of 43% by combined modality of therapy.10 Patients with lesions <5–10 cm in diameter were successfully treated with radical wide-field radiotherapy and surgery. Combination of surgery, radiotherapy and taxane (paclitaxel and docetaxel) has been shown to improve overall survival of the patients.
The present case is reported because of its rarity, extensive and multifocal involvement of the eyelids, periorbital area and the scalp.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Malignant angioendothelioma of the skin. Br J Dermatol. 1964;76:21-39.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous vascular proliferations. Part III Malignant neoplasms, other cutaneous neoplasms with significant vascular component, and disorders erroneously considered as vascular neoplasms. J Am Acad Dermatol. 1998;38:143-75.
- [CrossRef] [PubMed] [Google Scholar]
- The spectrum of mesenchymal skin neoplasms reflected by the new WHO classification. Onkologie. 2004;27:401-6.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous angiosarcoma of the face. J Eur Acad Dermatol Venereol. 2003;17:594-5.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous angiosarcoma presenting as recurrent angioedema of the face. Br J Dermatol. 2000;143:1346-8.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous angiosarcoma of the face: Clinicopathologic and immunohistochemical study of a case resembling rosacea clinically. J Am Acad Dermatol. 1998;38:837-40.
- [CrossRef] [PubMed] [Google Scholar]
- Angiosarcoma of the face and scalp, prognosis and treatment. Cancer. 1987;59:1046-57.
- [CrossRef] [PubMed] [Google Scholar]
- Outcomes after definitive treatment for cutaneous angiosarcoma of the face and scalp. Head Neck. 2010;33:661-71.
- [CrossRef] [PubMed] [Google Scholar]





