Translate this page into:
A pedunculated nodule over upper lip
Corresponding author: Prof. Somesh Gupta, Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi, Delhi, India. drsomesh.new@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gaurav V, Bhagwat A, Anand GRP, Gupta S. A pedunculated nodule over upper lip. Indian J Dermatol Venereol Leprol. 2024;90:823-5. doi: 10.25259/IJDVL_1128_2023
A 45-year-old male presented with a nodule over the left side of his upper lip for 10 years. It started as a small papule which gradually increased to the present size. On examination, a single pedunculated skin coloured to reddish-brown, non-tender, firm nodule of size 2.0 cm ´ 1.5 cm was observed over the upper lip [Figure 1]. A therapeutic excision was done and the nodule was sent for histopathology which showed a well-circumscribed multilobular dermal tumour composed of variably sized tubular structures with pink material in the lumen [Figure 2a]. These tubular structures were lined by doubled-layered epithelium [Figure 2b]. Some of these tubular structures showed decapitation secretions [Figure 2c]. The adjacent stroma was composed of collagen with some areas of sclerosis and hyalinization. There was no evidence of necrosis, nuclear atypia, abnormal mitotic activity or perineural invasion. The lesion resolved following excision [Figure 3].

- A skin coloured to reddish-brown nodule over the upper lip, below the left ala of the nose.
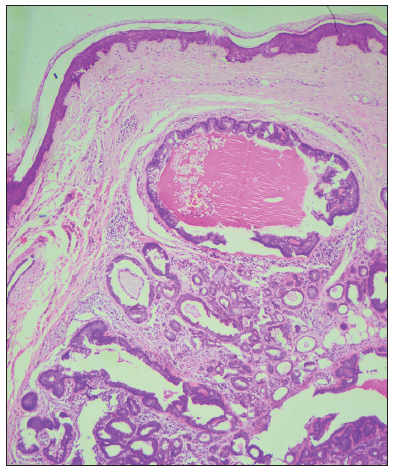
- Dermal tumour composed of variably sized tubular structures containing pink material in the lumen with adjacent stroma composed of collagen (Haematoxylin and Eosin, 40x).
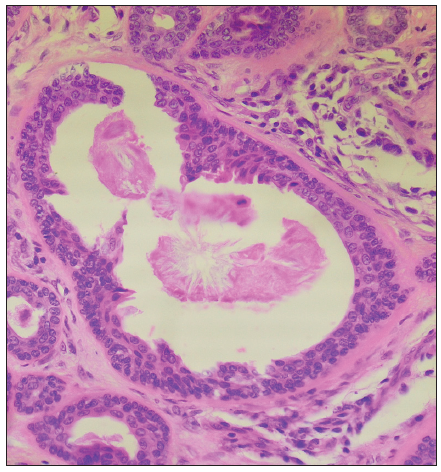
- Tubular structures lined by doubled-layered epithelium (Haematoxylin and Eosin, 400x).
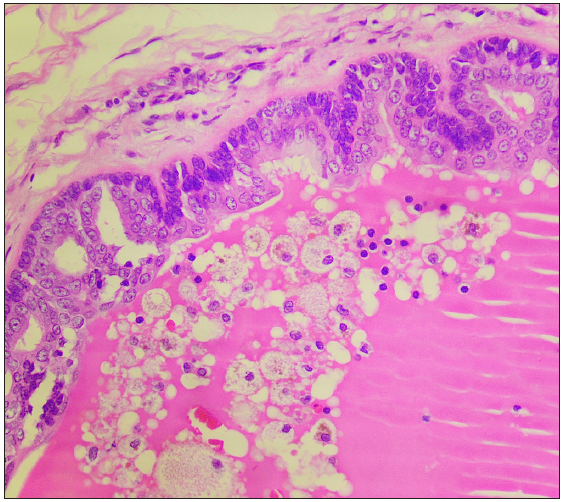
- Histopathology showing tubular structures with decapitation secretion (Haematoxylin and Eosin; 400x).

- Complete resolution following excision.
Question
What is your diagnosis?
Diagnosis
Tubular apocrine adenoma
Discussion
Tubular apocrine adenoma (TAA) is a rare benign adnexal neoplasm of apocrine derivation and usually presents as a painless slowly growing firm nodule. The most common site of involvement is the scalp (58%), despite the limited distribution of apocrine glands over this area. Besides the scalp, TAA can occur at other sites like the face, neck, upper and lower extremities, trunk and vulva. TAA was first reported by Landry and Winkelman and is mostly found in isolation and rarely in association with organoid lesions like naevus sebaceous and syringocystadenoma papilliferum (SCAP).1 The mean age at diagnosis is 48.9 ± 22.1 years and it is more common in females with a female-to-male ratio of 2:1.2
The exact origin of tubular apocrine adenoma is unknown. It is hypothesised to originate from primary epithelial germ cells, pluripotent appendageal cells or preexisting glands. Fisher proposed that TAA could be a minor variant of SCAP. Another theory based on histopathological similarities proposes that the superficial part of the lesion is formed by SCAP, while the deeper intradermal portion has characteristics akin to tubular papillary adenoma (TPA).3 Various adnexal tumours, such as TAA, papillary eccrine adenoma, apocrine cystadenoma, SCAP and TPA, exhibit notable similarities in their morphology, despite their distinct characteristics.4,5 Interestingly, about one-third of these tumours exhibit a composite nature, where histological features from two or three different types of adnexal tumours can coexist concurrently. To unite this diverse group of tumours, the term “tubulopapillary cystic adenoma with apocrine differentiation” has been introduced.5 Consequently, the term “tubular papillary adenoma” has been employed to describe lesions that fall within a spectrum ranging from papillary eccrine adenoma to tubular apocrine adenoma, as precise differentiation between these two entities can sometimes be challenging.5 Certain authors suggest the possibility of intermediate differentiation in adnexal tumours, which aligns with this idea. The emerging concept of “apo-eccrine glands” might prove valuable in this context as it helps explain the hypothesis of intermediate differentiation. It is worth noting, however, that these glands are not ubiquitous but present in specific areas of the body like the axillae, anogenital region, periumbilical region, areolae, external auditory canals, and the eyelids.4,5 Histologic features of TAA are characteristic and help in confirming the diagnosis. It is characterised by well-defined lobules of tubular structures within the dermis that may extend into the subcutis.2 The tubules are lined by two rows of cuboidal to columnar epithelial cells with decapitation secretion. There is minimal stroma which is usually fibrotic.4,5 Rarely, TAA may transform into apocrine adenocarcinoma.4,5 Complete surgical excision of the lesion to negative margins is usually curative.
In conclusion, the diagnosis and classification of sweat gland tumours pose challenges due to the subtle variations in the morphologies of different entities and the overlapping histopathological features. We report the occurrence of this rare tumour over the upper lip.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Tubular apocrine adenoma of the axilla: A rare adnexal tumor. Our Dermatol Online. 2015;6:360-1.
- [Google Scholar]
- A case of syringocystadenoma papilliferum with tubular papillary adenoma of the chest. J Nippon Med Sch. 2017;84:79-82.
- [CrossRef] [PubMed] [Google Scholar]
- Tubulopapillary cystic adenoma with apocrine differentiation: A unifying concept for syringocystadenoma papilliferum, apocrine gland cyst, and tubular papillary adenoma. Am J Dermatopathol. 2017;39:829-37.
- [CrossRef] [PubMed] [Google Scholar]
- Skin adnexal neoplasms - part 2: An approach to tumours of cutaneous sweat glands. J Clin Pathol. 2007;60:145-59.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





