Translate this page into:
A probable association of symmetrical drug-related intertriginous and flexural exanthema with levocetirizine
Correspondence Address:
Manisha Balai
Department of Dermatology, Venereology and Leprology, R. N. T. Medical College, Udaipur - 313 001, Rajasthan
India
| How to cite this article: Virath R, Gupta LK, Balai M. A probable association of symmetrical drug-related intertriginous and flexural exanthema with levocetirizine. Indian J Dermatol Venereol Leprol 2020;86:696-699 |
Sir,
Symmetrical drug-related intertriginous and flexural exanthema is defined as benign and self-limiting drug eruption, characterized by sharply defined symmetric erythema in the gluteal area and flexural or intertriginous folds, without systemic involvement. Antibiotics, including amoxicillin and cephalosporins are the most common drugs causing it.[1] Herein, we report a case of symmetrical drug-related intertriginous and flexural exanthema showing symmetrical erythematous eruptions mainly on the flexural areas that developed after intake of levocetirizine.
A 30-year-old man presented with sharply demarcated, itchy, non-scaly, erythematous lesions on the neck, groin, buttocks, axillary folds, cubital fossae and popliteal fossae [Figure - 1]a, [Figure - 1]b, [Figure - 1]c, [Figure - 1]d. The lesions started 3 days after taking tablet levocetirizine at a dose of 5 mg twice daily for lichen simplex chronicus on right leg. The rash first developed on the neck and groin. With continued medication, there was aggravation of symptoms in the form of burning and development of erythema on other flexures in next 2 to 3 days. Hair, nail, mucosa, and systemic examination were unremarkable. There was no history of any other drug intake. The patient was applying topical clobetasol propionate for lichen simplex chronicus on the right leg lesion. There was a history of mild similar episode with levocetirizine in the past, which resolved spontaneously with drug withdrawal. Routine investigations including hemogram and serum biochemistry were normal. Histological examination showed mild hyperkeratosis, focal parakeratosis, spongiosis and mild perivascular mononuclear inflammatory cells infiltration [Figure - 2]. Levocetirizine was stopped and the patient was started on prednisolone 30 mg daily orally for 7 days. There was marked improvement in itching and complete subsidence of rash in 1 week. Patient was advised not to take levocetirizine, hydroxyzine and cetirizine in future. After 4 weeks, skin patch test with levocetirizine, cetirizine and hydroxyzine was done, each in a base consisting of 30% petrolatum and 30% water. Readings were taken at 48 hours and 72 hours and were negative. Patient, however, refused oral provocation test with levocetirizine. Naranjo causality score was 5, implying a causal association of levocetirizine to symmetrical drug-related intertriginous and flexural exanthema as “probable.”
 |
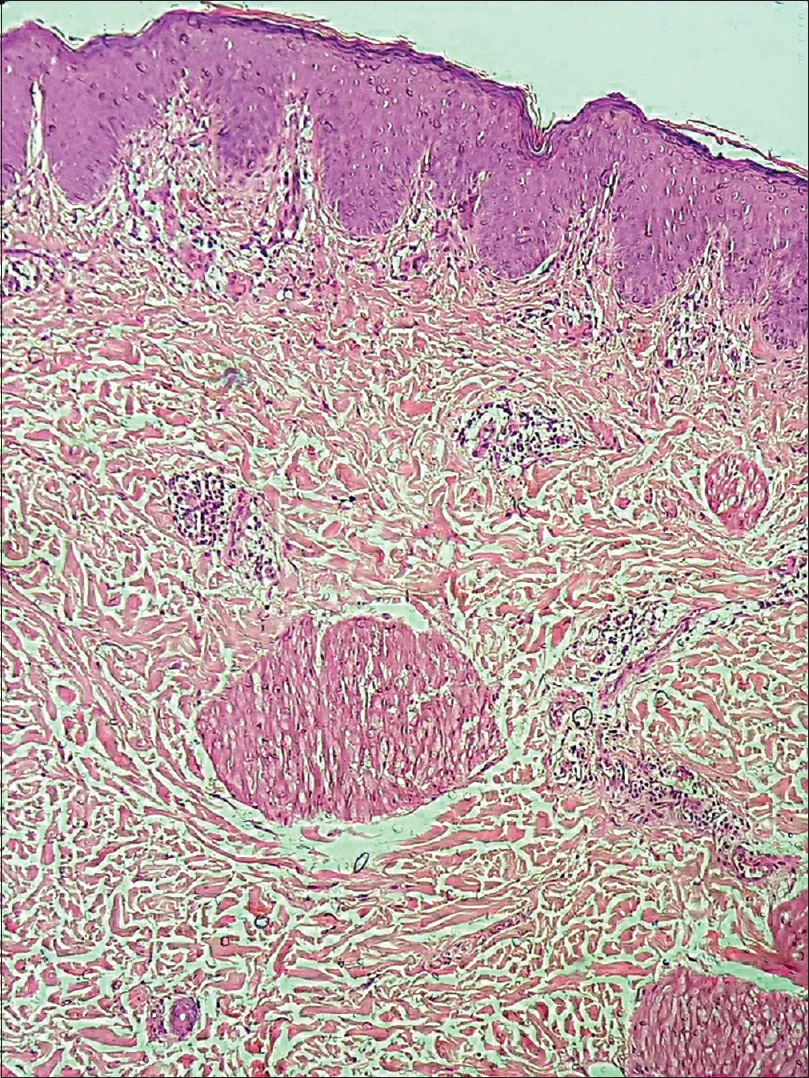 |
| Figure 2: Biopsy from the right groin area showed mild hyperkeratosis, spongiosis and mild perivascular mononuclear inflammatory cells (H and E, ×100) |
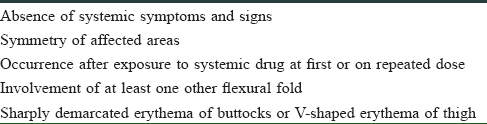
Häusermann et al.[2] coined the term symmetrical drug-related intertriginous and flexural exanthema in 2004, after noting cases of baboon syndrome related to drug exposure without prior sensitization. Among the medications causing symmetrical drug-related intertriginous and flexural exanthema, beta-lactam antibiotics, especially amoxicillin, are most common; others include pseudoephedrine, codeine, oxycodone, cimetidine, nystatin, and fluconazole, mercury, nickel, heparin, allopurinol, erythromycin, hydroxyurea, aminophylline, terbutaline, barium sulfate, iodinated radiocontrast media, intravenous immunoglobulin and cetuximab.[3] The exact mechanism involving symmetrical drug-related intertriginous and flexural exanthema is unknown. It is thought to be a type IV hypersensitivity reaction and is characterized by 5 diagnostic criteria [Table - 1].[2] Our patient fulfilled all of them. The morphology of the rash and histological findings were consistent with symmetrical drug-related intertriginous and flexural exanthema.
Although patch testing is essential for the diagnosis of symmetrical drug-related intertriginous and flexural exanthema, the rate of positive tests is not high and estimated to be approximately 50%.[4] Patch test done in our patient with levocetirizine, cetirizine and hydroxyzine using 10% concentration in petrolatum, on the uninvolved back skin was negative.
Levocetirizine dihydrochloride is a third-generation antihistamine. Despite a structural similarity of the three antihistamines, levocetirizine, cetirizine and hydroxyzine, cross-reactions among them are rarely reported.[5] Levocetirizine is generally considered to be a very safe drug but can sometimes cause adverse reactions, as seen in our case. However, onset of symptoms after second exposure to causative drug is quick but, in our patient, symptoms appeared after 72 hours of intake of levocetirizine, which is uncommon. Possibly the mild initial symptoms had gone unnoticed by the patient. Baboon syndrome induced by hydroxyzine has also been reported.[6] Antihistamines are very frequently used by dermatologists and are generally considered very safe. They can, however, paradoxically cause adverse reactions like fixed drug eruption and symmetrical drug-related intertriginous and flexural exanthema and, therefore, dermatologists should be aware of these rare adverse drugs reactions.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Mohapatra M, Panda M, Kar BR, Raj C. Symmetric drug-related intertriginous and flexural exanthema due to itraconazole: An uncommon side effect of a commonly used drug. Indian Dermatol Online J 2017;8:501-3.
[Google Scholar]
|
| 2. |
Häusermann P, Harr T, Bircher AJ. Baboon syndrome resulting from systemic drugs: Is there strife between SDRIFE and allergic contact dermatitis syndrome? Contact Dermatitis 2004;51:297-310.
[Google Scholar]
|
| 3. |
Elmariah SB, Cheung W, Wang N, Kamino H, Pomeranz MK. Systemic drug-related intertriginous and flexural exanthema (SDRIFE). Dermatol Online J 2009;15:3.
[Google Scholar]
|
| 4. |
Kim BJ, Kim HS, Lee JY, Kim HO, Park YM, La HO. Symmetrical drug-related intertriginous and flexural exanthema caused by celecoxib. Int J Dermatol 2014;53:e1-3.
[Google Scholar]
|
| 5. |
Lew BL, Haw CR, Lee MH. Cutaneous drug eruption from cetirizine and hydroxyzine. J Am Acad Dermatol 2004;50:953-6.
[Google Scholar]
|
| 6. |
Akkari H, Belhadjali H, Youssef M, Mokni S, Zili J. Baboon syndrome induced by hydroxyzine. Indian J Dermatol 2013;58:244.
[Google Scholar]
|
Fulltext Views
3,301
PDF downloads
1,510





