A rare case of disseminated cutaneous histoplasmosis
Corresponding author: Dr. Sirisha Varala, Department of Dermatology, Osmania Medical College, Afzalgunj, Hyderabad, 500012, Telangana, India. itsme.siri@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Panuganti S, Varala S, Damarla SV, Prasad JVDS. A rare case of disseminated cutaneous histoplasmosis. Indian J Dermatol Venereol Leprol 2022;88:533-6.
Sir,
Histoplasmosis, a systemic mycotic infection is caused by the dimorphic fungus, Histoplasma capsulatum. It is acquired through the inhalation of fungal spores present in soil contaminated with bat or bird faeces.1 It is endemic in some regions of America, Africa, and West Bengal (Eastern India), with few sporadic cases reported from southern India.1,2 Disseminated cutaneous histoplasmosis is commonly seen in immunocompromised patients. Conditions that increase the risk of dissemination include acquired immunodeficiency syndrome, organ transplant, hematologic malignancies, and immunosuppressive agents.1 We herein report a case of disseminated cutaneous histoplasmosis in an HIV seronegative patient on long term methotrexate therapy from a non-endemic region.
A 65-year-old female presented with multiple, painful, red elevated lesions over the face and trunk with oral cavity erosions of five months duration. Few lesions were associated with purulent discharge and crusting. She had fever associated with chills and rigour, weight loss, dry cough, and shortness of breath one month prior to the onset of skin lesions and was treated as an acute exacerbation of asthma, following which systemic symptoms improved. She gave a history of working in an area that was heavily inhabited by birds, with plenty of bird excreta in soil. There was no significant travel history in the recent past. She was on treatment with low dose methotrexate (20 mg weekly once) and intermittent oral steroids, since the last four years for rheumatoid arthritis. On physical examination, she was undernourished and cachectic with pallor. On clinical systemic examination, there was no organomegaly. Cutaneous examination showed small hyperpigmented, crusted plaques over the face [Figure 1a] and multiple erythematous, annular to polycyclic plaques with erosions and crusting over the anterior and posterior aspects of the trunk [Figure 1b and c]. Multiple erosions were seen over the tongue and hard plate [Figure 1d]. Differential diagnoses considered were nutritional dermatosis, pemphigus foliaceous, necrolytic migratory erythema and acquired zinc deficiency. Skin biopsy revealed plenty of macrophages containing yeast forms with basophilic nucleus with perinuclear halo throughout the dermis [Figure 2a]. On periodic acid Schiff staining, dermis showed periodic acid Schiff-positive organisms with a perinuclear halo [Figure 2b]. Gomori’s methenamine silver staining showed multiple, small, black yeast cells [Figure 2c]. Direct immunofluorescence from perilesional skin was negative. Bone marrow aspirate showed plenty of macrophages with numerous organisms showing yeast-like appearance with encapsulation [Figure 2d]. Routine lab investigations revealed anaemia, hypoalbuminemia, and thrombocytosis. Tissue culture was not done due to the unavailability of Biosafety level 3 laboratory. Computed tomography of the abdomen revealed multiple, tiny, calcified granulomas in both lobes of the liver. Computed tomography of the chest revealed patchy fibrotic changes and subpleural fibrotic strands. A diagnosis of disseminated cutaneous histoplasmosis was made and the patient was started on oral itraconazole 200 mg per day, following which there was an improvement in lesions. The patient was later lost to follow up.

- Small crusted plaques over the face

- Multiple, well defined, annular to polycyclic plaques with erosions and crusting over anterior aspect of trunk

- Multiple, well defined, annular plaques with erosions over posterior aspect of trunk

- Erosions over hard palate
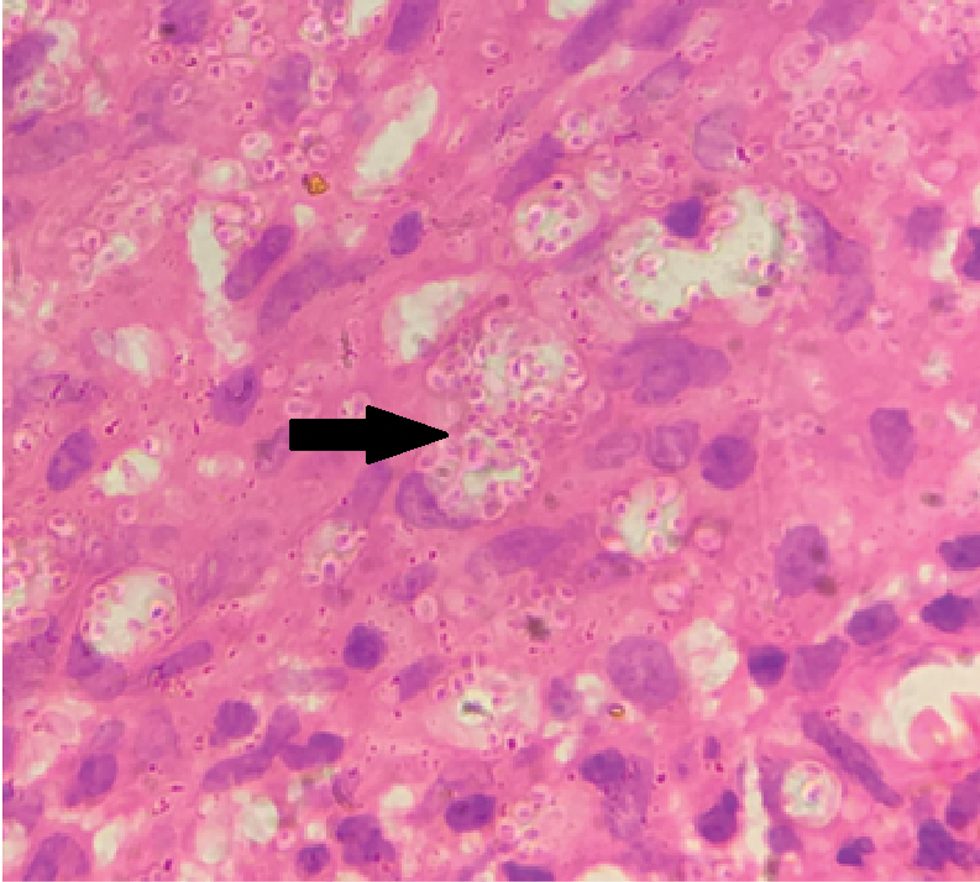
- Plenty of parasitized macrophages in dermis (arrow) (H & E, ×100)
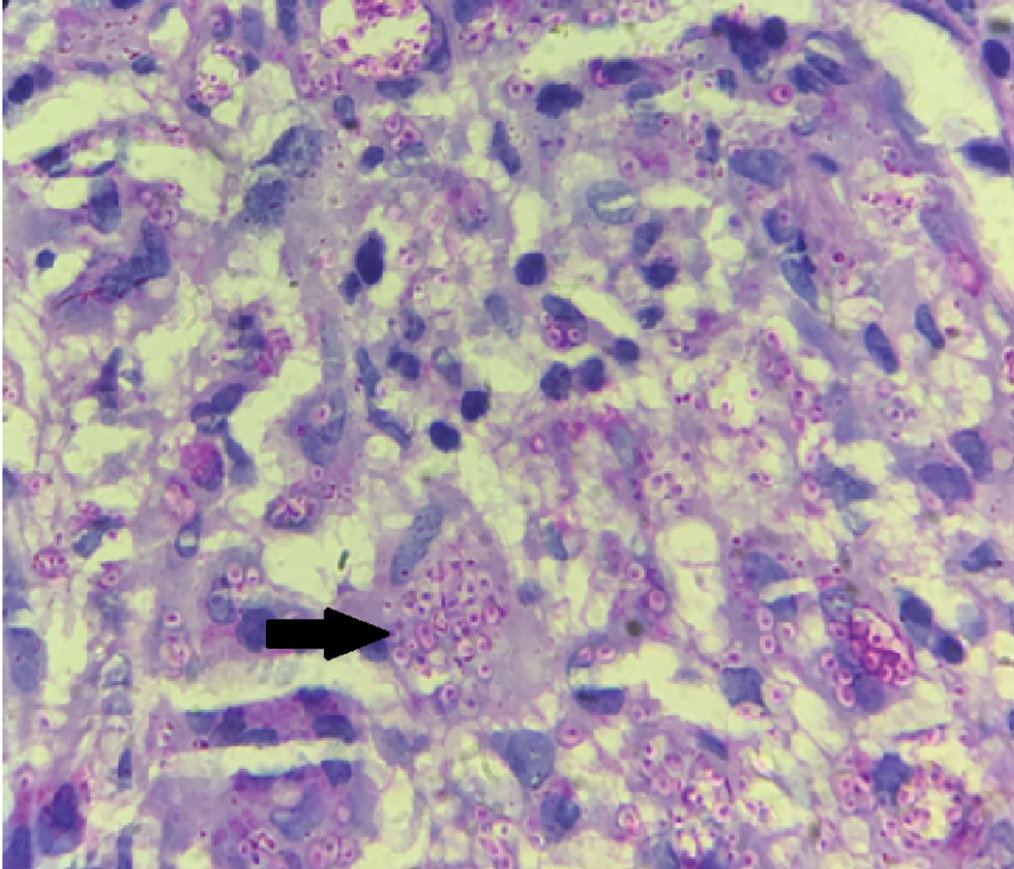
- Periodic acid Schiff positive organisms within the macrophages with perinuclear halo (arrow) (PAS stain, ×100)
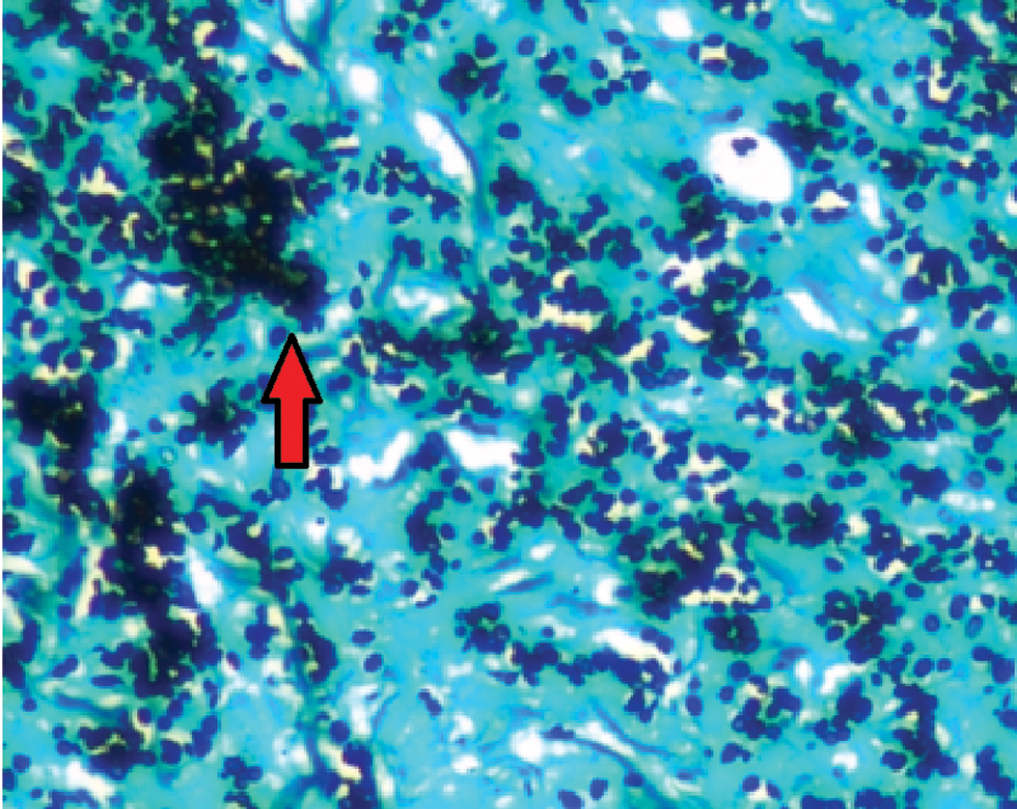
- Gomori’s methenamine silver stain showing yeast forms (arrow) (GMS stain, ×100)
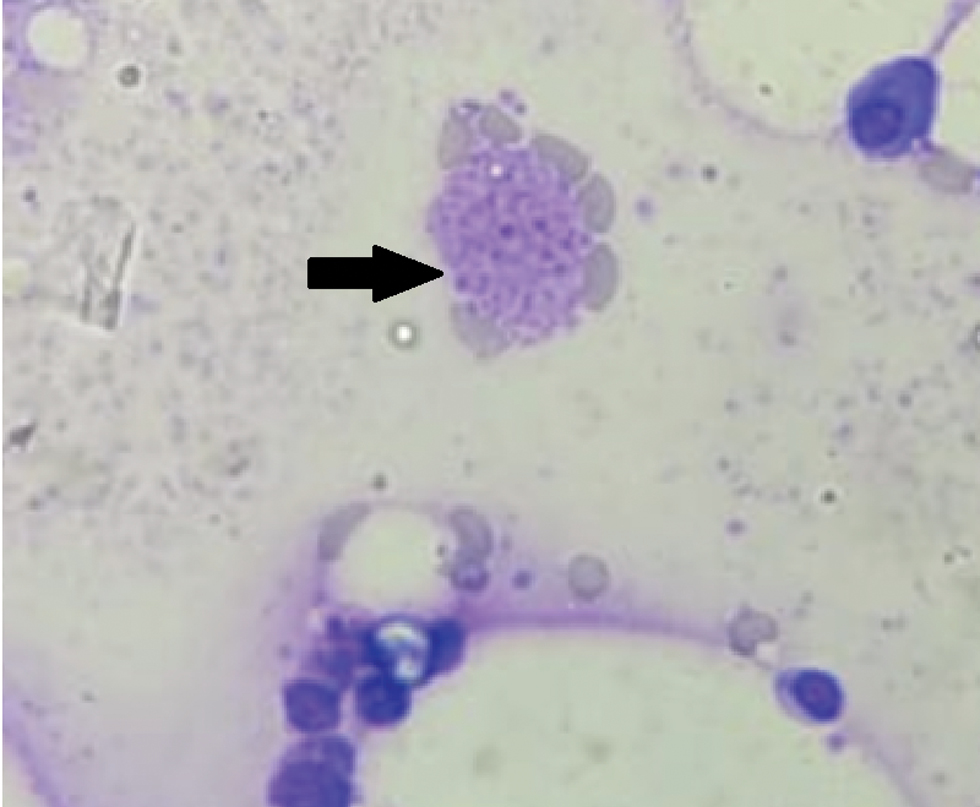
- Bone marrow aspirate smear showing macrophages with yeast like organisms (arrow) (Giemsa stain, ×100)
Histoplasmosis has a worldwide distribution, with the first case from India reported by Panja and Sen.3 Thereafter many cases were reported from Bengal, with sporadic reports from Maharashtra and other parts of the country.3 Our patient was a resident of a non-endemic region from South India but worked in an area where the soil was contaminated with bird excreta. We assume that our patient acquired the disease via inhalation of airborne conidia of Histoplasma capsulatum from the soil.
There are three clinical presentations of histoplasmosis, namely, primary cutaneous, pulmonary, and progressive disseminated (PDH) forms. Histoplasmosis is asymptomatic in 95% of the patients.4 However, the pulmonary infection may disseminate hematogenously to liver, spleen, kidney, lymph nodes, bone marrow and mucocutaneous tissues, resulting in progressive disseminated histoplasmosis which usually occurs in immunocompromised hosts. Cutaneous lesions are non-specific with varied presentations such as mucocutaneous erosions/ulcers, or multiple erythematous papules/nodules with scaling or crusting.5 However, annular to polycyclic erythematous plaques as seen in our case, have rarely been reported.
Our patient developed progressive disseminated histoplasmosis presumably due to immunosuppression secondary to chronic methotrexate therapy and oral steroids. Similar to our case, Roy et al.6 reported disseminated histoplasmosis following prolonged low dose methotrexate therapy, in whom the diagnosis was confirmed by bone marrow biopsy. Dussouil et al.7 reported a patient treated with methotrexate and corticosteroid therapy for rheumatoid arthritis who presented with disseminated histoplasmosis that partially mimicked dermatomyositis.
In our case, the diagnosis was made based on histopathology and bone marrow aspirate examination with special staining. Histopathology, a primary tool in the diagnosis of the disease, typically shows tiny 2–4 μm spores within the cytoplasm of macrophages which appear as round or oval bodies surrounded by a clear space and stains with special stains like periodic acid Schiff or Giemsa stain.8
Focal calcifications were seen in the liver in our case, which indicate prior infection with histoplasma. Focal calcifications are also seen in tuberculosis, which is a major public health problem in India leading to diagnostic difficulties.9 Amphotericin B is the drug of choice for disseminated histoplasmosis. However, in patients who cannot tolerate amphotericin B, itraconazole is a highly effective and alternative therapy and histoplasma is one of the rare opportunistic deep fungal infections causing organ damage. It is usually missed clinically, especially in non-endemic areas, in which case, a proper clinical history along with histopathology and special stains help in making an accurate diagnosis. Our case is unique in its morphological presentation with large erythematous polycyclic plaques as opposed to the classical presentation with papules and nodules.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- A case of oral localized histoplasmosis in an immunocompetent patient. Eur J Clin Microbiol Infect Dis. 2001;20:753-55.
- [CrossRef] [PubMed] [Google Scholar]
- Disseminated cutaneous histoplasmosis in an immunocompetent adult. Indian J Dermatol. 2012;57:206-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Disseminated histoplasmosis (a case report) J Postgrad Med. 1983;29:270-3.
- [PubMed] [Google Scholar]
- Chronic disseminated histoplasmosis bone marrow involvement in an immunocompetent patient. Indian J Hematol Blood Transfus. 2010;26:65-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Case report: Histoplasmosis in Himachal Pradesh (India): An emerging endemic focus. Am J Trop Med Hyg. 2017;97:1749-56.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Disseminated histoplasmosis following prolonged low-dose methotrexate therapy. Am J Hematol. 2000;63:59-60.
- [CrossRef] [PubMed Central] [Google Scholar]
- Disseminated histoplasmosis partially mimicking a dermatomyositis in a patient with rheumatoid arthritis. Br J Dermatol. 2015;173:797-800.
- [CrossRef] [PubMed] [Google Scholar]
- Disseminated histoplasmosis with oral and cutaneous manifestations. J Oral Maxillofac Pathol. 2013;17:139-42.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Liver calcifications and calcified liver masses: Pattern recognition approach on CT. Am J Roentgenol. 2018;211:76-86.
- [CrossRef] [PubMed] [Google Scholar]
- Disseminated histoplasmosis with atypical cutaneous lesions in an Italian HIV-infected patient: Another autochtonous case. HIV Med. 2003;4:145-8.
- [CrossRef] [PubMed] [Google Scholar]





