Translate this page into:
A rare case of metastatic superficial cutaneous calcification due to tumour lysis in a case of non-Hodgkin lymphoma
Corresponding author: Dr Biju Vasudevan Department of Dermatology, Armed Forces Medical College, Pune, Maharashtra, India. biju.deepa@rediffmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sinha A, Kumar V, Vasudevan B, Chandra M. A rare case of metastatic superficial cutaneous calcification due to tumour lysis in a case of non-Hodgkin lymphoma. Indian J Dermatol Venereol Leprol 2021;87:696-9.
Sir,
Calcinosis cutis, first described by Virchow in 1855, is a term used for a group of disorders where calcium gets deposited in the skin. It is classified into four etiological types: dystrophic, metastatic, iatrogenic and idiopathic. Metastatic calcification occurs in the setting of abnormal calcium or phosphate metabolism and may be associated with hypercalcemia and/ or hyperphosphatemia. Metastatic calcification has been reported in Hodgkin disease and leukemia very rarely.
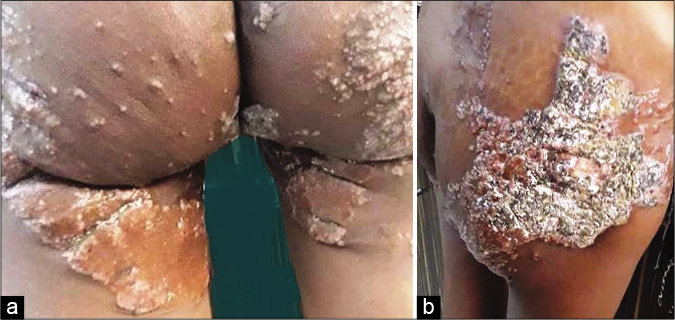
A 30-year-old woman presented to the dermatology outpatient department of a tertiary care hospital for evaluation of painful reddish hard lesions over both buttocks. Three months prior, the patient had been diagnosed with non-Hodgkin’s lymphoma-B cell type when she presented with a history of chronic relapsing fever, low back pain and weight loss of 15 kg six months duration. Whole body fluorine-18 fluoro- d-glucose positron emission tomography integrated with computed tomography (F18 FDG PET-CT) scan done at the time of initial presentation had revealed hypermetabolic cervical and axillary lymphadenopathy with bilateral breast involvement and multiple lytic skeletal lesions [Figure 1]. The patient was started on chemotherapy with monthly cycles of rituximab, cyclophosphamide, doxorubicin, vincristine and prednisolone (R-CHOP).

- PET scan showing involvement of various soft tissues and skeleton by non-Hodgkin’s lymphoma before chemotherapy. Cervical lymph nodes – SUV max – 13.70, axillary lymph nodes – 14.13, breast – 15.75, skeletal lesions – 10.87
One month after the first cycle of chemotherapy, she started developing these reddish raised lesions over both buttocks and because of the pain, she could not lie supine.
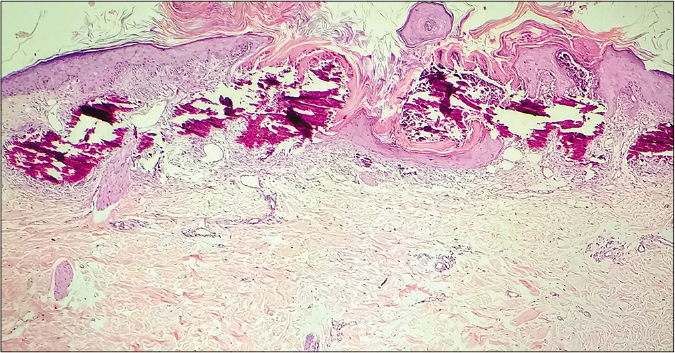
On examination, the patient’s vital parameters were normal. Dermatological examination revealed involvement of both gluteal regions and back of thighs with well defined, irregular discrete to confluent, symmetrical reddish-brown verrucous rocky hard to smooth crusted plaques and a few peripherally scattered papules involving the gluteal region and posterior aspect of thighs bilaterally [Figures 2 and 3]. There was tenderness on deep pressure. The proximal half of all the fingernails and toenails revealed melanonychia [Figure 4] and the patient also had diffuse alopecia over scalp with loss of eyebrows and eyelashes due to the chemotherapy.
- (a) Calcified hypertrophic plaque on both buttocks and posterior upper thighs (b) Close-up of lesions on the right buttock

- Close up of the calcified plaques on the upper posterior thigh

- Melanonychia of finger nails following chemotherapy
Skin biopsy from the lesion over buttocks revealed numerous basophilic, granular and amorphous deposits within the upper dermis and epidermis surrounded by a palisade of histiocytes [Figures 5 and 6]. Surrounding dermis showed fibroplasia with sparse mixed inflammatory infiltrate. Von Kossa stain showed calcium deposits. Repeat PET-CT scan showed dense coarse calcification in uterus, perineum, lower back and bilaterally in breast parenchyma, axillary lymph nodes, kidneys, elbows, gluteal regions and posteromedial aspect of upper thighs [Figure 7]. When compared to initial PET-CT done three months back, previously active lesions of non-Hodgkin lymphoma showed reduction in size and number and were no longer FDG avid. Serum calcium (15 mg/dl), ionic calcium and phosphorus (7.3 mg/dl) were raised. As the serum albumin, parathormone and calcitriol levels were normal and the patient had no associated radiological findings, pseudohyperparathyroidism and ectopic calcitriol production were ruled out. The patient was hence diagnosed to have metastatic calcinosis cutis following tumor lysis with visceral metastatic calcification. She was started on tab. diltiazem 180 mg once a day and tab. sodium alendronate 70 mg once a week.
- Histopathology from skin lesion showing features of calcinosis cutis in the epidermis and upper dermis. Hematoxylin and eosin stain, 100×.
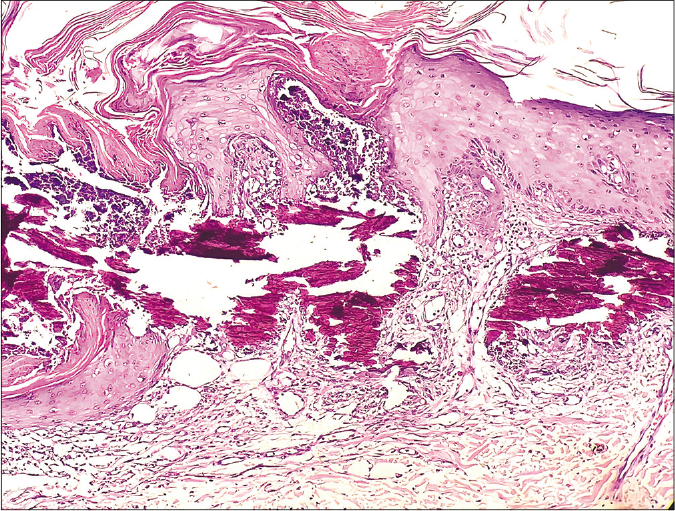
- High-power view of histopathology showing the extensive calcification in the upper dermis. Hematoxylin and eosin stain, 400×
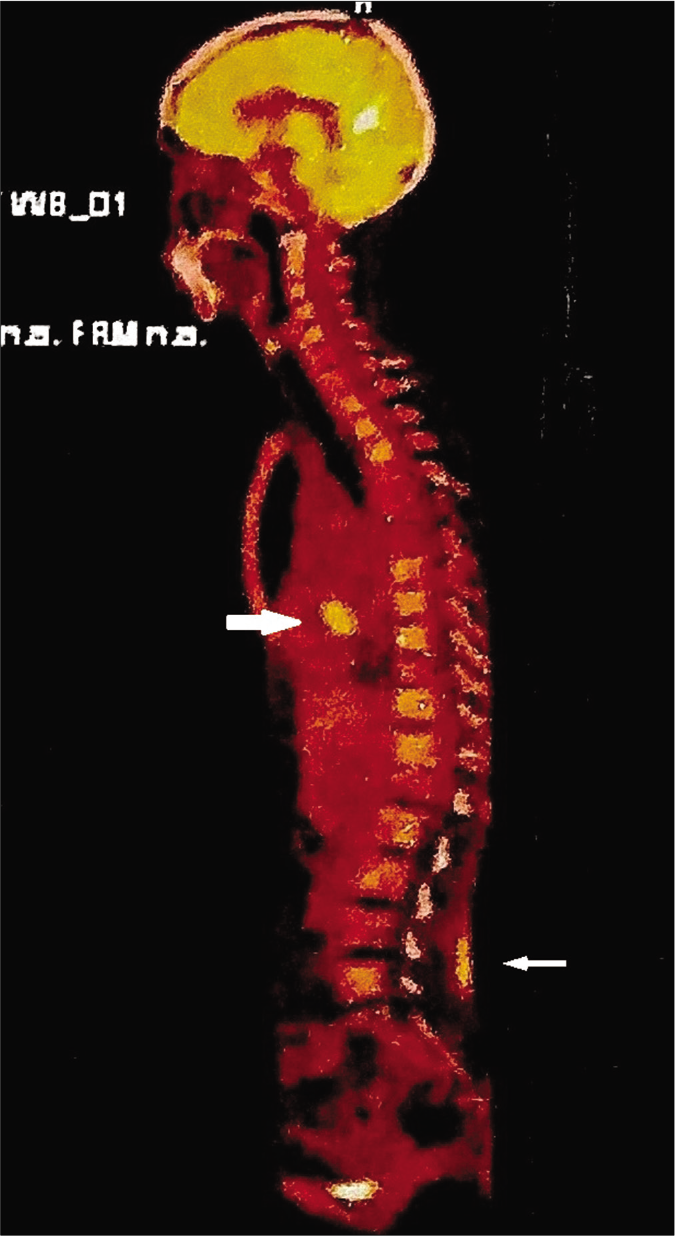
- PET scan showing the calcification in breasts and skin of lower back (shown by white arrows)
Calcinosis cutis can be classified based on the type of calcification process as dystrophic, metastatic, idiopathic and iatrogenic. Dystrophic calcification is seen in previously damaged, necrotic, inflamed or neoplastic skin tissue with normal serum calcium and phosphate levels.1 Id iopathic calcinosis cutis is seen usually in children with no previous tissue injury or metabolic defect and normal serum calcium and phosphorous.2 Iatrogenic calcinosis cutis is usually seen following treatment or procedures.3 Metastatic calcification occurs when there are associated abnormalities in calcium and phosphorus metabolism. The common causes of metastatic calcification are chronic renal failure, hyperparathyroidism, Paget disease, hypervitaminosis D, milk-alkali syndrome, sarcoidosis and calciphylaxis.4
Hypercalcemia has been reported in various malignancies. The causes could be increased bone resorption due to skeletal involvement, various factors produced by the tumors such as parathormone-related protein, osteoclast activating factor, ectopic calcitriol production and tumor lysis.
One case each of metastatic calcification has been reported previously in Hodgkin lymphoma5 and non-Hodgkin lymphoma.6 However, the patients presented with metastatic calcification in various visceral organs only. In our case, the skin manifestations were the presenting complaint and this led to the early diagnosis of metastatic calcification, thus aiding appropriate management of the patient. An extensive literature search could not reveal such cutaneous manifestations as the presenting feature due to metastatic calcification in non-Hodgkin lymphoma cases.
Another interesting aspect of the case was that the calcification was restricted to epidermis and upper dermis which is also a rare finding.
Even though tumor lysis is a very rare cause of metastatic calcification, the onset of calcinosis following one cycle of chemotherapy, presence of increased ionic and serum calcium along with hyperphosphatemia, and calcification in various organs in the absence of other etiologies point to tumor lysis as the cause in this patient. The lysis of tumor would have led to release of osteoclast stimulating cytokines, release of calcium from bone, hypercalcemia and increased ionic calcium resulting in the deposition in various organs and soft tissues as in the cases of tumor lyses described following chemotherapy in Hodgkin lymphoma.7,8 Another interesting aspect in our case was the calcification being restricted to epidermis and upper dermis. Usually, the idiopathic and dystrophic variants of calcinosis cutis present with deeper and larger deposits. Early detection, involvement of upper dermal vessels, friction area predominant disposition and source of tumour lysis being non-Hodgkin lymphoma could have led to the appearance of smaller and superficial calcifications in our patient.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Calcinosis cutis: Part I. Diagnostic pathway. J Am Acad Dermatol. 2011;65:1-12.
- [CrossRef] [Google Scholar]
- Cutaneous deposition diseases. Part II. J Am Acad Dermatol. 1998;39:527-46.
- [CrossRef] [Google Scholar]
- Metastatic calcinosis cutis in a patient with Hodgkin's lymphoma. Dermatol Online J. 2018;24:13030/qt7z73b3kk.
- [CrossRef] [Google Scholar]
- Metastatic calcification of multiple visceral organs in non-Hodgkin's lymphoma. J Nucl Med. 1995;36:820-1.
- [Google Scholar]
- The hypercalcemia of cancer, Clinical implications and pathogenic mechanisms. N Engl J Med. 1984;310:1718-27.
- [CrossRef] [Google Scholar]
- B cell malignancies presenting with unusual bone involvement and mimicking multiple myeloma, Study of nine cases. Am J Med. 1987;83:10-6.
- [CrossRef] [Google Scholar]





