Translate this page into:
A rare presentation of elephantiasis involving vulvae in an Indian female
2 Department of Biochemistry, All India Institute of Medical Sciences, Bhopal, Madhya Pradesh, India
Correspondence Address:
Mahendra Pratap Singh
Department of Surgery, All India Institute of Medical Sciences, Bhopal - 462 020, Madhya Pradesh
India
| How to cite this article: Singh MP, Saluja R. A rare presentation of elephantiasis involving vulvae in an Indian female. Indian J Dermatol Venereol Leprol 2020;86:753 |
Sir,
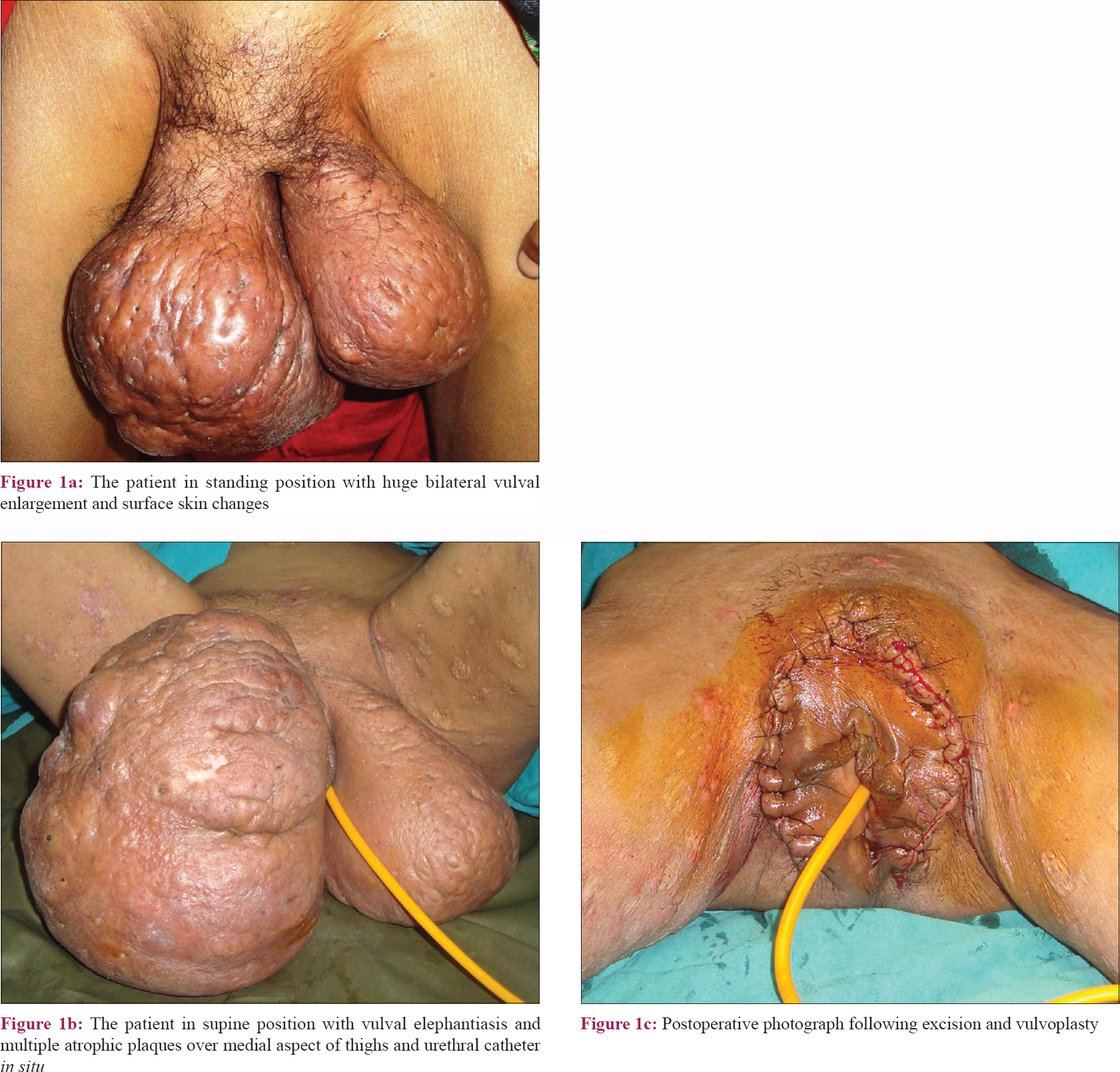
We recently came across an interesting case of elephantiasis vulvae, in a middle-aged married Indian female, where a surgical excision and reconstruction resulted in a satisfactory outcome. A 45-year-old Indian female presented to the Laxmi Narayan Medical College Hospital, Bhopal, with a 14-year history of progressively enlarging vulval swellings affecting her daily physical activities including coitus. The patient reported that the swelling on the right vulva appeared 4 years prior to that of the left, with local itching, redness, and aching pain but she denied any history of abnormal vaginal discharge or menstrual irregularity. She had previously been treated with antibiotics, antifilarial, antifungal drugs, and also tried pressure garments without any beneficial result. She had an associated feeling of marked social embarrassment. She denied previous surgery, exposure to radiation, or edematous condition in her family. On physical examination, the patient showed difficulty in walking with unusually wide gait. Genital examination revealed disfigured vulvae with huge bilateral, pedunculated swellings, hanging on both the right and left labia majus, measuring 30 cm × 15 cm and 15 cm × 10 cm size, respectively, and mimicking scrotum with buried penis. The overlying skin was thickened with extensive rugosities and was chronically infected showing foul smelling, seropurulent discharge with surrounding excoriations. The medial aspect of thigh showed multiple atrophic plaques. The rest of her physical examination including inner vaginal wall, urethra, and inguinal lymph node area was unremarkable [Figure - 1]a and [Figure - 1]b.
 |
Imaging study with local ultrasonography and magnetic resonance imaging demonstrated fibro-fatty tissue with fluid-filled cystic spaces in deep dermis. Thoracoabdominal computed tomography scan was unremarkable. Lymphoscintiography study revealed normal inguinal and pelvic lymph nodes. Her laboratory values were significant for anemia (hemoglobin 7 gm%) and raised erythrocyte sedimentation rate (30 mm) at first hour. The night blood smear and serology for microfilarial antigen, serology for syphilis and human immunodeficiency virus, tissue smear for Donovan bodies, nucleic acid amplification test to detect lymphogranuloma venereum (LGV), Mantoux test for tuberculosis, and Pap smear were all reported negative. The smear from surface discharge showed Staphylococcus aureus and stained negative for acid-fast bacilli and fungus. Fine-needle aspiration cytology showed hypocellular smears with occasional chronic infiltrate of lymphocytes in a proteinacious background. A diagnosis of elephantiasis vulvae secondary to chronic skin infection was made after excluding the other known causes.
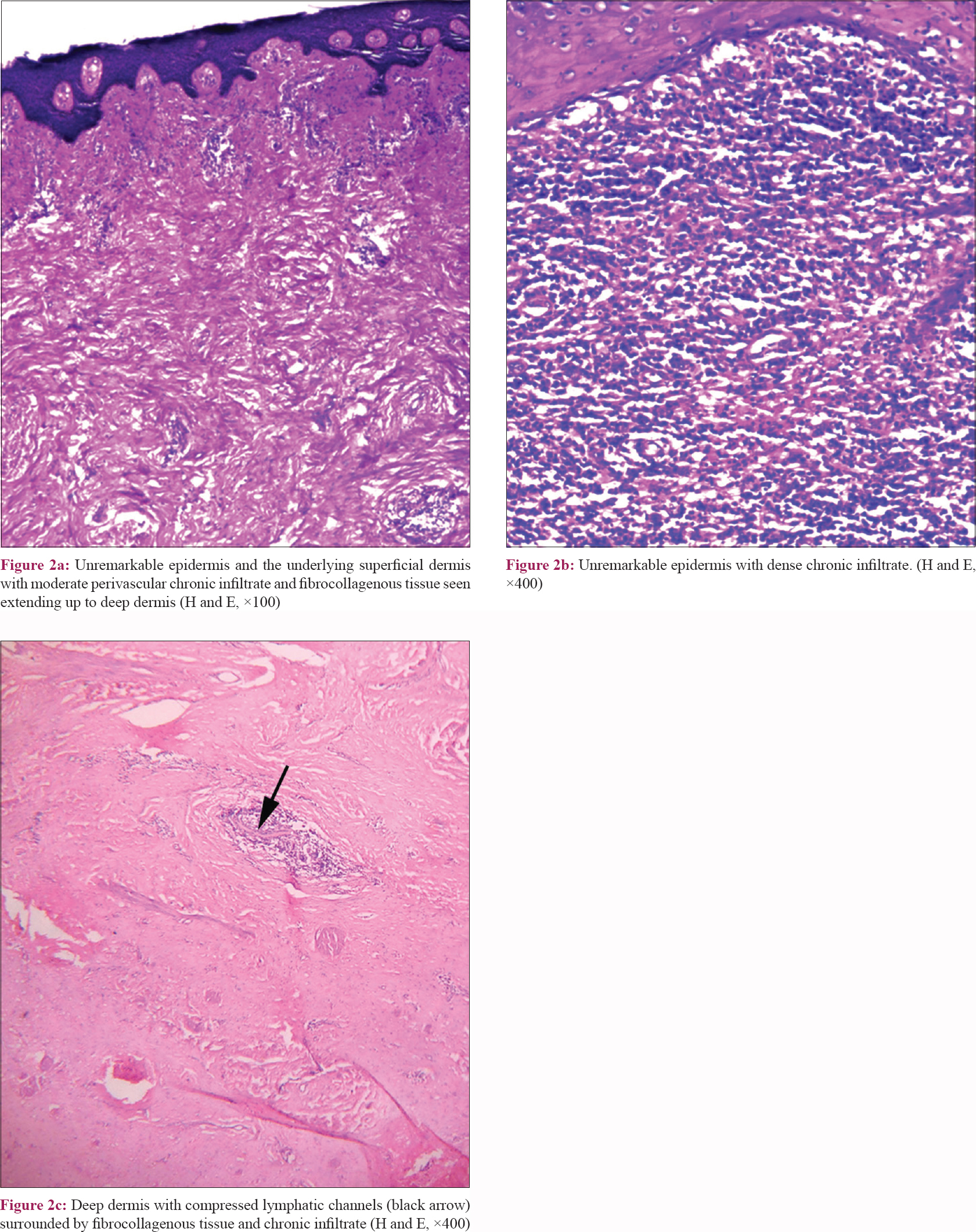
After correcting anemia and controlling local infection with culture sensitive antibiotics, we performed surgical debulking of excessive fibro-fatty tissue and excision of loose hanging vulval skin, wide to inner labial flap. A vulvoplasty to maintain natural bulge with primary closure of defect with normal adjacent skin was done [Figure - 1]c. On histopathological examination, the excised polypoid soft tissue mass was grossly fibrotic, grayish yellow, and firm on cut section. Microscopically, the lesion was covered by acanthotic epidermis, and superficial and deep dermis showed dense collagen and numerous dilated lymphatics. Tissue smear for Donovan bodies and LGV, malaria parasite, and microfilaria were all reported negative. The features were consistent with chronic lymphedema changes in elephantiasis vulvae [Figure - 2]a-c].
 |
Postoperatively, seroma formation was noted under right flap which was drained with pressure. Compression bandage dressing was continued and she was discharged after a week with advise to use suitably designed undergarment facilitating pressure drainage and maintain local hygiene. The patient showed satisfactory outcome at 1 year of postoperative follow-up.
The term “elephantiasis” was first used by a Roman encyclopedist Celsus (30 BC–50 AD) to describe “elephant-like appearance” of massively enlarged lower limbs due to chronic lymphatic obstruction, but this crippling disease of tropics and subtropics was known to ancient Indians much before the biblical time as “Slipada” (Sli = elephant, pada = leg) as described in Sushruta Samhita and also known to Greece and Medieval Persia.[1],[2] Subsequently, the term was also used to describe similar enlargement in other body parts such as trunk, upper limbs, breast, and external genitalia. The common causes of chronic lymphatic dysfunction are lymphatic filariasis due to Wuchreria bancrofti and Brugia malayi[3] and sexually transmitted diseases such as LGV and donovanosis.[4] It has also been reported following tubercular lymphadenitis,[5] neoplastic diseases, surgery, and radiation. In a few cases, the available laboratory investigations could not ascertain the cause.[6]
Vulval elephantiasis represents a rare form of localized chronic lymphedema. It is both a physical and mental burden to the patient and family. Elephantiasis commonly affects the body parts diffusely with recurring inflammation; exceptionally, lymphedema involves circumscribed region of skin producing pedunculated swelling and localized elephantiasis.[7] Classic elephantiasis tropica is commonly caused by obstruction of the lymphatic system with filarial parasites in our country although we could not detect the same in the present case. Genital lymphoedema has been shown to be associated with chronic pyogenic infection.[8] We assume that recurring inflammation secondary to chronic skin infection could have resulted in lymphatic dysfunction in our case.
Surgical excision of the enlarged mass wide to the inner labial flap with vulvoplasty showed an encouragingly acceptable result.[5] Lymphoscintiography study is helpful in preoperative functional evaluation of chronic lymphedema particularly in cases with uncertain etiology and in planning lymphatic shunting procedure.[9] The result of initial decongestive lymphatic therapy in managing elephantiasis is unsatisfactory. There is still no effective treatment available to manage elephantiasis with uncertain etiology and this highlights the need to search for other specific causes with newer laboratory methods.
Acknowledgment
The auhors also thank Dr. Ashwani Tandon and Dr. T Santosh, Department of Pathology and Lab Medicine, AIIMS Bhopal, for their expert pathological description. Author would like to acknowledge support from LN Medical College Hospital, Bhopal.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
MPS acknowledges the support of LN Medical College Bhopal and AIIMS Bhopal for infrastructure support. RS would like to acknowledge the support from the DBT, India, for Remalingswami Re-entry Fellowship.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Hajdu SI. Elephantiasis. Ann Clin Lab Sci 2002;32:207-9.
[Google Scholar]
|
| 2. |
Golzari SE, Kazemi A, Ghaffari A, Ghabili K. A brief history of elephantiasis. Clin Infect Dis 2012;55:1024.
[Google Scholar]
|
| 3. |
Khanna NN, Joshi GK. Elephantiasis of female genitalia. Case report. Plast Reconstr Surg 1971;48:379-81.
[Google Scholar]
|
| 4. |
Gupta S, Ajith C, Kanwar AJ, Sehgal VN, Kumar B, Mete U. Genital elephantiasis and sexually transmitted infections – Revisited. Int J STD AIDS 2006;17:157-65.
[Google Scholar]
|
| 5. |
Chintamani Singh J, Tandon M, Khandelwal R, Aeron T, Jain S, et al. Vulval elephantiasis as a result of tubercular lymphadenitis: Two case reports and a review of the literature. J Med Case Rep 2010;4:369.
[Google Scholar]
|
| 6. |
Kos M, Ljubojević N, Ilić-Forko J, Babić D, Jukić S. Elephantiasis of the vulva of an unclear etiology: Case report. Lijec Vjesn 1996;118:158-60.
[Google Scholar]
|
| 7. |
Lu S, Tran TA, Jones DM, Meyer DR, Ross JS, Fisher HA, et al. Localized lymphedema (elephantiasis): A case series and review of the literature. J Cutan Pathol 2009;36:1-20.
[Google Scholar]
|
| 8. |
Nishimoto S, Kinoshita M, Miyazaki Y, Kawai K, Kakibuchi M. Lymphoedema of the penis and scrotum as a sequela of chronic skin infection. J Surg Case Rep 2016;2016. pii: rjw127.
[Google Scholar]
|
| 9. |
Vaqueiro M, Gloviczki P, Fisher J, Hollier LH, Schirger A, Wahner HW. Lymphoscintigraphy in lymphedema: An aid to microsurgery. J Nucl Med 1986;27:1125-30.
[Google Scholar]
|
Fulltext Views
5,603
PDF downloads
2,184





