Translate this page into:
A retrospective case series of 10 patients with malignant melanomas arising from small- and medium-sized congenital melanocytic nevi in South Koreans
Corresponding author: Prof. Seok-Jong Lee, Department of Dermatology, Kyungpook National University Hospital, 130 Dongdeok-Ro, Jung-Gu, Daegu 41944, South Korea. seokjong@knu.ac.kr
-
Received: ,
Accepted: ,
How to cite this article: Kim JY, Kim SM, Park KD, Jang YH, Lee WJ, Lee SJ. A retrospective case series of 10 patients with malignant melanomas arising from small- and medium-sized congenital melanocytic nevi in South Koreans. Indian J Dermatol Venereol Leprol 2021;87:293-7.
Sir,
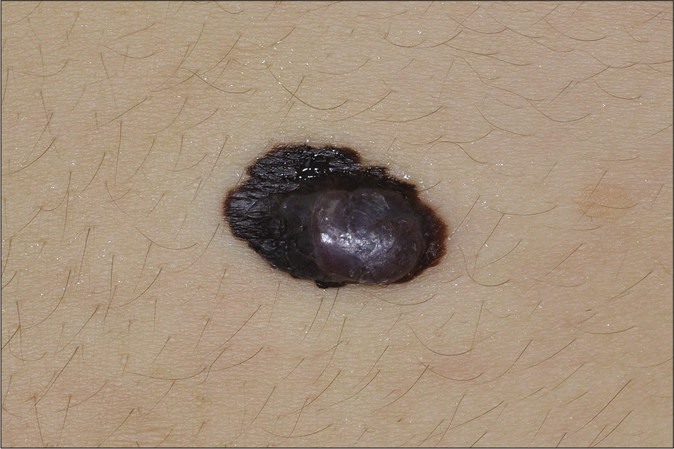
Unlike giant congenital melanocytic nevi, small and mediumsized congenital melanocytic nevi are not considered as precursors of malignant melanoma. However, malignant melanomas arising from small and medium-sized congenital melanocytic nevi have been seen in clinical practice [Figure 1a-d]. In the present study, we retrospectively investigated the incidence and clinicopathological features of malignant melanomas arising from small and mediumsized congenital melanocytic nevi and compared their features with invasive malignant melanomas arising from non-congenital melanocytic nevi. The study was based on the medical records of patients with small and mediumsized congenital melanocytic nevi and patients with invasive malignant melanomas, diagnosed at Kyungpook National University Hospital, Daegu, South Korea between January 2011 and June 2017.

- Malignant melanoma arising from medium-sized congenital melanocytic nevus. A 45-year-old woman’s nodule on 5.0 cm × 3.5 cm sized congenital melanocytic nevus on her left lower back (Patient 1)

- Malignant melanoma arising from small-sized congenital melanocytic nevus. A 43-year-old woman’s nodule on 0.8 cm × 0.7 cm sized congenital melanocytic nevus on her right shin (Patient 3)
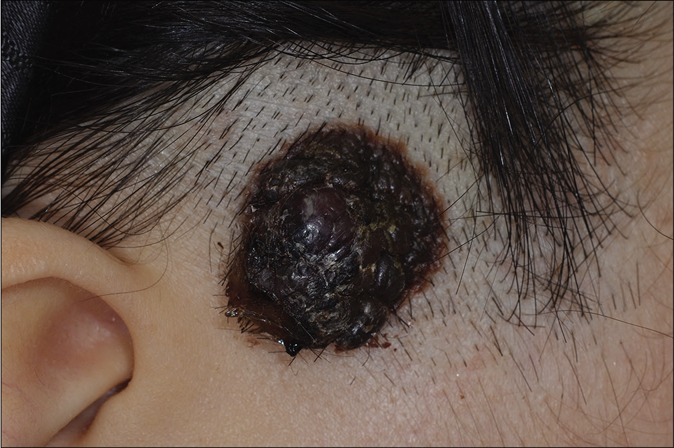
- Malignant melanoma arising from medium-sized congenital melanocytic nevus. A 21-year-old woman’s nodule on 2.1 cm × 2.0 cm sized congenital melanocytic nevus on her right sideburn (Patient 4)
- Malignant melanoma arising from medium-sized congenital melanocytic nevus. A 36-year-old woman’s nodule on 1.7 cm × 1.2 cm sized congenital melanocytic nevus on her lower back (Patient 9)
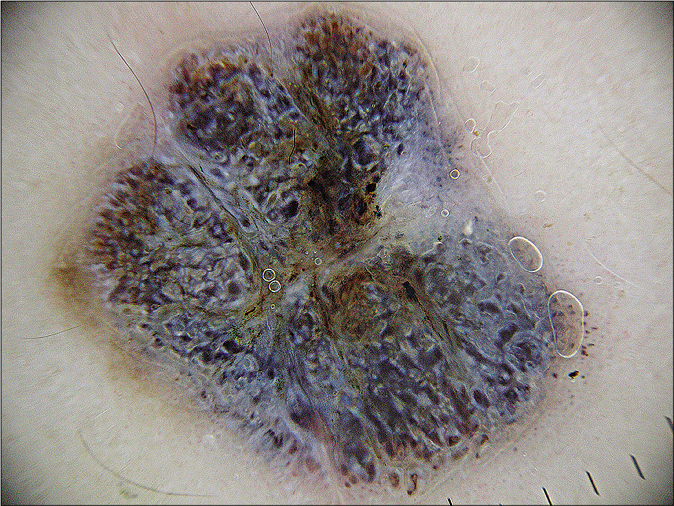
- Dermoscopic image of Patient 3. Asymmetric pigmentation, multiple colors (white, brown, blue, purple, black) and blue whitish veils are observed
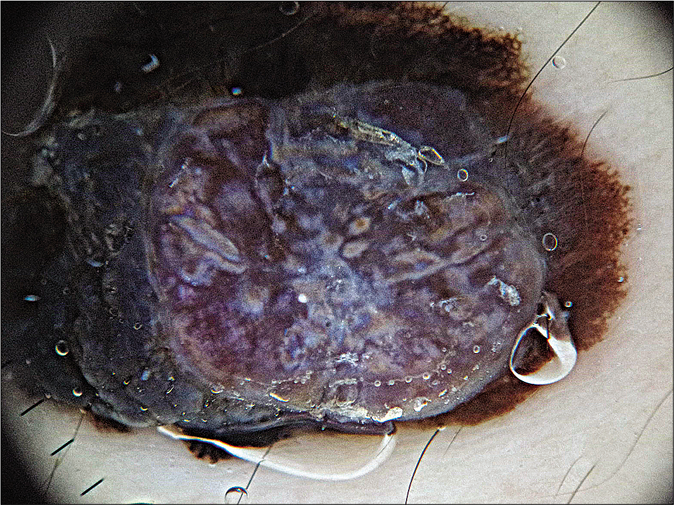
- Dermoscopic image of Patient 9. A nodule shows multiple colors (blue-white, white, brown, purple, black) and blue whitish veils but asymmetric pigment network and atypical vascular pattern are not remarkable
A congenital melanocytic nevus is defined as one which has been present since birth and has clinical features of melanocytic nevi. They are classified into three groups according to the largest projected adult diameter based on the New York University Registry classification: small (<1.5 cm), medium (1.5-19.9 cm) and large or giant (≥20.0 cm).1 The size of each congenital melanocytic nevus was measured on the first visit to this hospital. All malignant melanomas were diagnosed histologically by a skin biopsy. Dermoscopic findings of malignant melanomas arising from small and medium-sized congenital melanocytic nevi were also evaluated. The ethics committee of the institutional review board approved this study (Kyungpook National University Hospital 2018-03-011). A χ2 test using SAS version 9.3 (SAS Institute Inc, Cary, NC) was conducted for statistical analysis. A p-value of <0.05 indicated statistical significance.
All patients in this study had Fitzpatrick skin types III or IV. Malignant melanomas were found in 10 (2.7%) of 377 small and medium-sized congenital melanocytic nevi, out of a total 371 patients during the 6.5-year period of this retrospective study and all 10 were invasive melanomas [Figure 2a and b]. These accounted for 8.2% (10/122) of all invasive malignant melanomas during the same study period. One (2.2%) malignant melanoma developed in 45 small-sized congenital melanocytic nevi and 9 (2.7%) in 332 medium-sized. It was found that these 10 patients first visited this hospital a mean of 16.7 months after the suspected lesion of melanoma each developed. The patients with malignant melanomas arising from small and medium-sized congenital melanocytic nevi were predominantly women (8:2) and their mean age at diagnosis was 49.2 years. They initially developed as mainly nodules (80%), usually located eccentrically (75%) on nevi. On dermoscopic examination, blue-whitish veil and multiple colors were detected in malignant melanomas arising from small and mediumsized congenital melanocytic nevi but the asymmetric pigment network suggestive of classic malignant melanoma was not noticeably present [Figure 1e and f]. Table 1 shows the clinicopathological characteristics of the 10 malignant melanomas arising from small and medium-sized congenital melanocytic nevi. The patients with malignant melanomas arising from small and medium-sized congenital melanocytic nevi were significantly younger compared to those arising from noncongenital melanocytic nevi [mean age: 49.2 vs 63.0 years, respectively; Table 1, P = 0.003]. Although acral melanomas are predominant in Koreans, the 10 malignant melanomas arising from small and mediumsized congenital melanocytic nevi were distributed evenly throughout the body [Table 1, P = 0.001]. The Breslow thicknesses, rates of metastases, tumor stage, treatment and recurrence rates were not significantly different between the two groups [Table 1, P > 0.05]. Table 1 also shows a comparison of clinicopathological characteristics between malignant melanomas arising from small and medium-sized congenital melanocytic nevi and malignant melanomas arising from noncongenital melanocytic nevi.
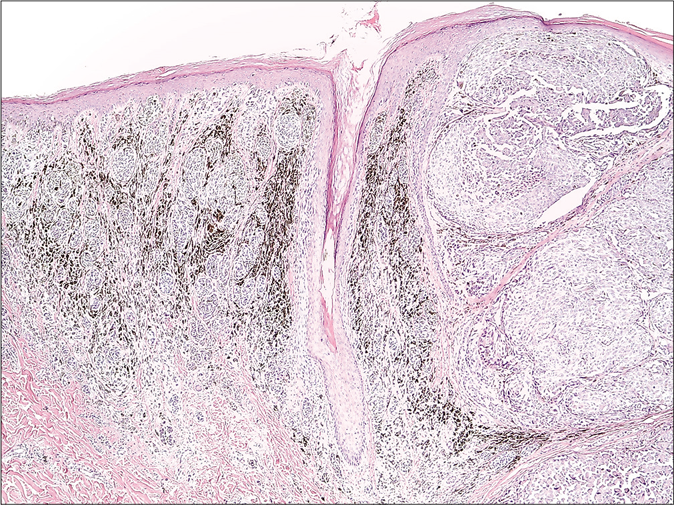
- Malignant melanoma arising from medium-sized congenital melanocytic nevus (Patient 9). Benign nevus cells (Left side of image) and malignant melanoma cells (right side of image) were observed together (H and E, ×400)
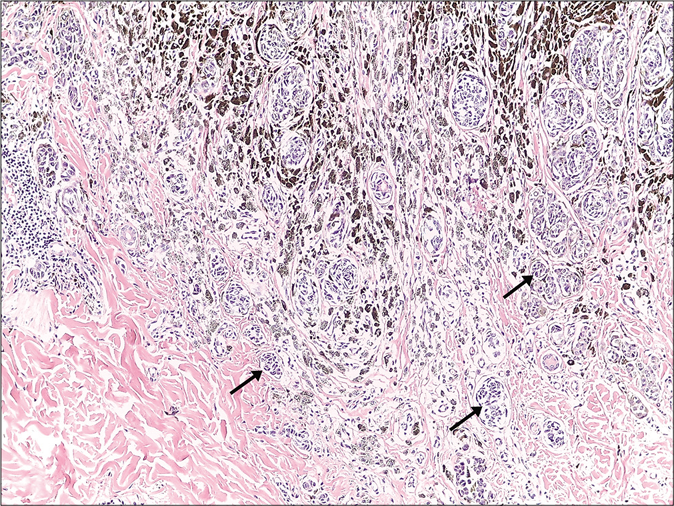
- Benign nevus cell nests were observed in the relatively deep area in the dermis (black arrows, H and E, ×100)
| Characteristics | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 | Patient 7 | Patient 8 | Patient 9 | Patient 10 | smCMN-MM (n=10) | non-CMN-MM (n=110*) | P |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | Woman | Woman | Woman | Woman | Man | Woman | Woman | Woman | Woman | Man | Woman 80% | Woman48.2% | 0.095 |
| Age (year) | 45 | 52 | 43 | 21 | 54 | 62 | 90 | 32 | 36 | 57 | Mean 49.2 | Mean 63.0 | 0.003 |
| CMN size (cm) | 5.0×3.5 | 1.8×1.1 | 0.8×0.7 | 2.1×2.0 | 2.3×1.7 | 2.0×1.2 | 5.5×3.0 | 3.0×3.0 | 1.7×1.2 | 3.5×1.5 | Mean 2.8×1.9 | N/A | |
| Presence of nodule | + | − | + | + | − | + | + | + | + | + | 80% | N/A | |
| Eccentric location of the nodule | + | N/A | − | + | N/A | + | + | − | + | + | 75% | N/A | |
| Location | Left lower back | Right neck | Right shin | Right sideburn | Right palm | Right popliteal | Left ankle | Right shin | Lower back | Right lower abdomen | Head and neck: 20% | ||
| Trunk: 30% | |||||||||||||
| Extremities: 40% | |||||||||||||
| Hand and foot: 10% | Head and neck: 15.5% | ||||||||||||
| Trunk: 10.9% | |||||||||||||
| Extremities: 8.2% | |||||||||||||
| Hand and foot: 65.5% | 0.001 | ||||||||||||
| Breslow thickness (mm) | 2.1 | 1.1 | 1.4 | 8.0 | 1.2 | 7.5 | 13.0 | 6.0 | 4.1 | 2.5 | Mean 4.7 | Mean 5.7 | 0.535 |
| Presence of ulceration | + | − | − | + | − | + | + | + | − | + | 60% | 71.8% | 0.475 |
| Mitosis | ≥1 | ≥1 | ≥1 | ≥1 | 0–1 | ≥1 | ≥1 | ≥1 | ≥1 | ≥1 | 90% ≥1 | 80.9% ≥1 | 0.687 |
| Positive sentinel lymph node | − | − | − | − | − | − | − | − | + | + | 20% | 28.2% | 0.725 |
| Positive distant metastasis | − | − | − | − | − | − | − | − | − | − | 0% | 5.5% | 1.000 |
| AJCC stage | IIB (T3bN0M0) | IB (T2aN0 M0) | IB (T2aN0 M0) | IIC (T4bN0 M0) | IB (T2aN0M0) | IIC (T4bN0 M0) | IIC (T4bN0M0) | IIC (T4bN0M0) | IIIA (T4aN1aM0) | IIIA (T3bN1aM0) | Stage I: 30% | Stage I: 9.1% | 0.212 |
| Stage II: 50% | Stage II: 60% | ||||||||||||
| Stage III: 20% | Stage III: 25.5% | ||||||||||||
| Stage IV: 0% | Stage IV: 5.5% | ||||||||||||
| Recurrence | Lung | - | - | Submandibular lymph node | - | Right inguinal lymph node | - | - | - | - | 30% | 21.8% | 0.692 |
smCMN-MM: Malignant melanoma arising from small-and medium-sized congenital melanocytic nevi, non-CMN-MM: Malignant melanoma arising from noncongenital melanocytic nevi skin, AJCC: American Joint Committee on Cancer, N/A: Not available. *Two of 122 invasive malignant melanomas from giant CMN were excluded from non-CMN-MM group
One most important issue in congenital melanocytic nevi management is the risk of malignant transformation into melanoma. The risk for the development of malignant melanoma in giant congenital melanocytic nevi is well-known through a lot of past research which shows quite a high incidence rate of about 2% to 10%.2 However, malignant melanomas arising from small and medium-sized congenital melanocytic nevi are rare. One group reported that none of the 239 patients with 1 to 19 cm congenital melanocytic nevi developed melanomas and another reported that no malignant melanoma occurred in 230 medium-sized congenital melanocytic nevi in 227 patients.3,4 However, Rhodes and Melski confirmed the presence of a preexisting small-sized congenital melanocytic nevi at the site of melanoma based on histology and patient history in 2.6% and 14.9% of cases, respectively.5 In this study, we encountered 10 (2.7%) invasive malignant melanomas in 377 small- and medium-sized congenital melanocytic nevi over a duration of 6.5 years. The incidence was as high as that (2.3%) of malignant melanomas arising from giant melanocytic nevi in South Korea.6 The age-standardized incidence rates of cutaneous malignant melanoma in the general population in South Korea was only 0.66 per 100,000 people for men and 0.58 for women.7 Although our hospital is a tertiary referral center in Korea, the annual incidence rate of new malignant melanoma patients from new outpatients in our department is about 0.6%. It is also important to note that although the incidence rate of cutaneous malignant melanoma in South Korea is higher in men than in women; malignant melanomas arising from small-and medium-sized congenital melanocytic nevi have occurred predominantly in women (80%) in this study. Further research is needed to confirm whether gender is one of the predisposing factors. In addition, most of the malignant melanomas arising from small- and medium-sized congenital melanocytic nevi arose with nodular shape; hence, features of nodular melanoma such as multiple colors, symmetrical shape and blue-whitish veil in some cases were observed in the dermoscopic examination.8 They were significantly different from the findings suggestive of classic malignant melanoma.
There are some limitations to our study. Firstly, as our hospital is a tertiary referral center in Korea, determining the exact incidence of this condition may be biased and inaccurate. A further nationwide study of malignant melanomas arising from small- and medium-sized congenital melanocytic nevi is needed to enhance our understanding of this critical issue. Secondly, most congenital melanocytic nevi were diagnosed based on only clinical diagnosis and history from the patients and/or their parents and no other special analyses was performed. Lastly, 5-year overall survival could not be obtained because of a short follow-up period.
In conclusion, we observed that small- and medium-sized congenital melanocytic nevi might be one of the precursors of cutaneous melanoma in Koreans. Although we were unable to find any previous reports of malignant melanomas arising from small- and medium-sized congenital melanocytic nevi from other Asian countries, careful medical observation is required for small- and mediumsized congenital melanocytic nevi in colored people. The invasive form developed earlier, and more often on nonacral areas, compared to malignant melanomas arising from noncongenital melanocytic nevi. Therefore, congenital melanocytic nevi must be regularly photographed and observed for any changes, regardless of size, to prevent delay in diagnosis and treatment of potential malignant melanomas. Palpation and biopsy of the suspected lesion is more important than observing it with dermoscopy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2018R1C1B5085905).
Conflicts of interest
There are no conflicts of interest.
References
- Congenital nevocytic nevi and malignant melanomas. J Am Acad Dermatol. 1979;1:123-30.
- [CrossRef] [Google Scholar]
- Giant congenital melanocytic nevus. An Bras Dermatol. 2013;88:863-78.
- [CrossRef] [PubMed] [Google Scholar]
- The risk of melanoma in patients with congenital nevi: A cohort study. J Am Acad Dermatol. 1995;32:595-9.
- [CrossRef] [Google Scholar]
- Risk of melanoma in medium-sized congenital melanocytic nevi: A follow-up study. J Am Acad Dermatol. 1998;39:428-33.
- [CrossRef] [Google Scholar]
- Small congenital nevocellular nevi and the risk of cutaneous melanoma. J Pediatr. 1982;100:219-24.
- [CrossRef] [Google Scholar]
- Clinical characteristics and risk of melanoma development from giant congenital melanocytic naevi in Korea: A nationwide retrospective study. Br J Dermatol. 2012;166:115-23.
- [CrossRef] [PubMed] [Google Scholar]
- Nationwide trends in the incidence of melanoma and non-melanoma skin cancers from 1999 to 2014 in South Korea. Cancer Res Treat. 2018;50:729-37.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic evaluation of nodular melanoma. JAMA Dermatol. 2013;149:699-709.
- [CrossRef] [PubMed] [Google Scholar]





