Translate this page into:
A retrospective study of the pattern of sexually transmitted diseases during a ten-year period
Correspondence Address:
| How to cite this article: Narayanan B. A retrospective study of the pattern of sexually transmitted diseases during a ten-year period. Indian J Dermatol Venereol Leprol 2005;71:333-337 |
Abstract
Background: Proper knowledge of the patterns of sexually transmitted diseases (STDs) in different geographical regions is necessary for evolving proper strategies for control of these diseases. Aims: To study the pattern of STDs and to analyze the changes during a ten-year period from 1990 among patients attending Medical College Hospital, KottayamMethods: Case records of 686 patients with STDs who attended the outpatient wing of the Department of Dermatology and Venereology were studied. Results: There were 504 males and 182 females in the total of 686 patients. Marital contact alone was reported by 123 (67.6%) female patients. Genital ulcer diseases (GUDs) accounted for the maximum number of STDs, with 504 cases (73.5%), followed by condyloma acuminatum (17.5%) and gonorrhea (10.1%). Forty-three patients had multiple infections. The total number of patients during the first year of study was 129, while it was 41 during the last year. Bacterial STDs showed a striking reduction in numbers. The decline was less marked in the case of viral STDs. Conclusion: The majority of patients had genital ulcer diseases. Spouses were the most common source of infection for female patients. There was a marked decline in the number of patients with various STDs during the ten-year period. The decline was more evident in the bacterial STDs resulting in an apparent increase of the viral STDs towards the end of the period of study.
 |
 |
Introduction
Sexually transmitted diseases (STDs) constitute a major public health problem for both developing and developed countries. The emergence of human immunodeficiency virus (HIV) infection has increased the importance of measures aimed at control of STDs. A proper understanding of the patterns of STDs prevailing in different geographic regions of a country is necessary for proper planning and implementation of STD control strategies. It is with this aim that the present study was undertaken.
METHODS
Case records of 686 patients with STDs who attended the Department of Dermatology and Venereology, Medical College, Kottayam for ten years, from January 1990 to December 2000 (excluding 1994, records for the year not being available) were analyzed in this retrospective study. Cases had been diagnosed based on the clinical presentation and investigations available in the hospital.
RESULTS
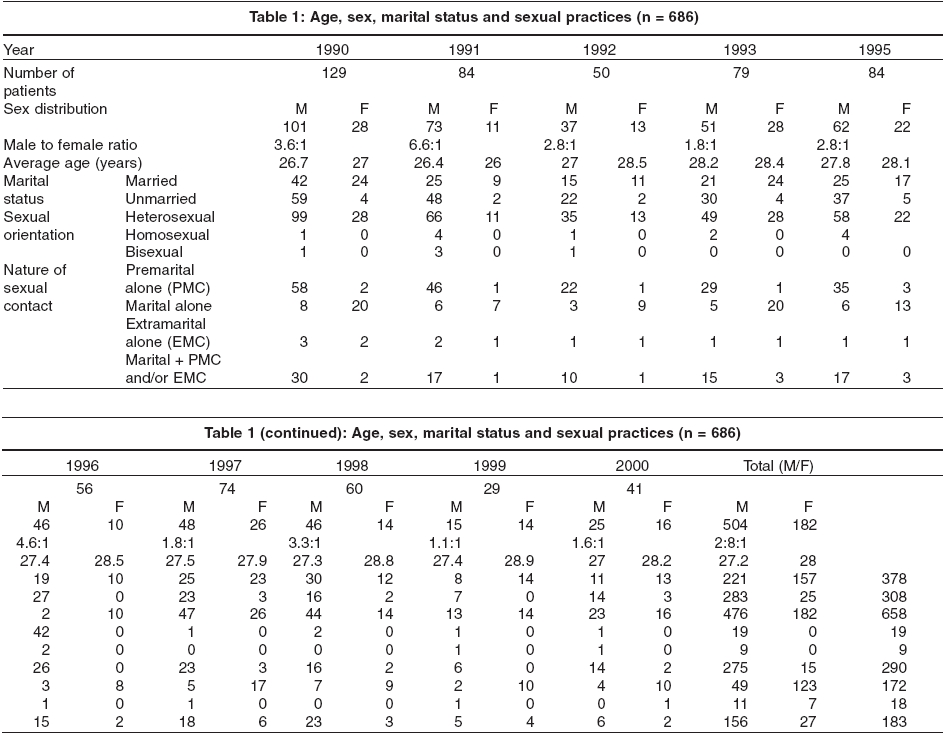
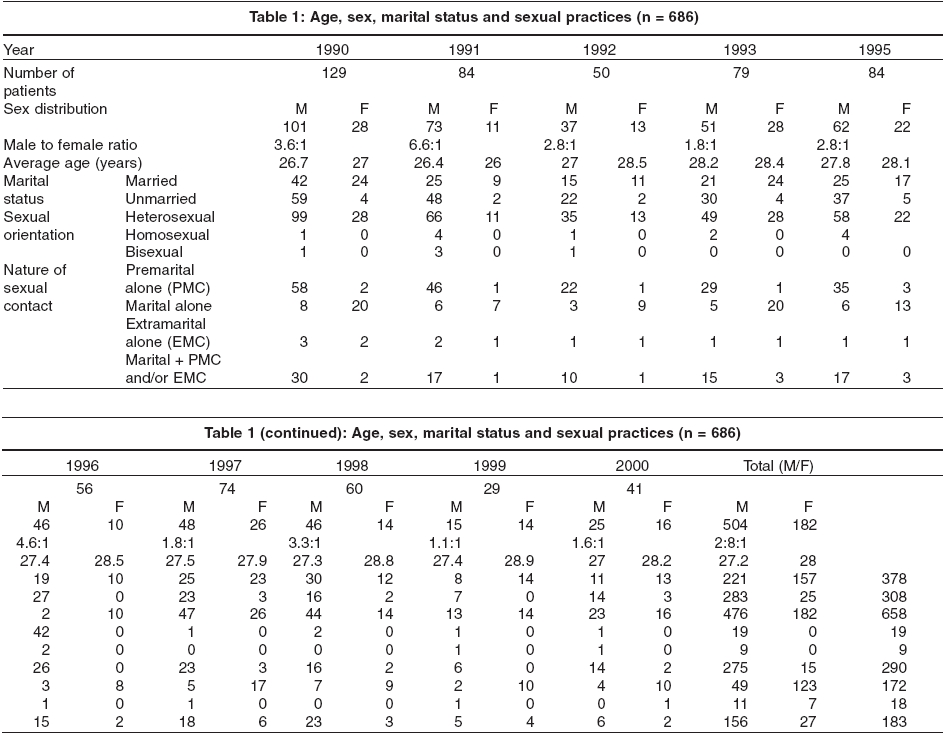
The total number of cases was 686, 504 males (73.5%) and 182 (26.5%) females [Table - 1]. There was an evident decline in the total number of cases during the ten years. During the first year of the study, the number of cases was 129 while in the tenth year it was only 41. Males outnumbered the females in a ratio of 2.8:1 during the ten-year period, but the ratio varied from year to year. The average age of patients during the ten-year period was 27.2 years for males and 28 years for females. There was no significant difference from year to year.
Out of the 686 patients, 378 (55.1%) were married and 308 (44.9%) were unmarried Of those married, 2 were widowed and 21 were either living separately from their spouses or were divorced. The majority (56%) of male patients was unmarried, while 86% of female patients were married [Table - 1]. There was a wide variation in the ratio of the married to the unmarried in the case of male patients from year to year.
Of the 686 patients, 658 (95.9%) were heterosexuals, while 19 (2.8%) were homosexuals and 9 (1.3%) were bisexuals [Table - 1]. All the homosexual and bisexual patients were males. The pattern was fairly constant throughout the ten-year period. A history of premarital contact alone was obtained from 275 (54.6%) male patients, while only 15 (8.2%) female patients gave such a history. Marital exposure alone was present in 49 (9.7%) males and 123 (67.6%) females. History of extramarital exposure alone was obtained from 11 (2.2%) males and 7 (3.8%) females; all these patients were divorced or separated. History regarding nature of exposure was not obtained in 23 cases. The nature of sexual contact did not show any appreciable change in pattern during the study period.
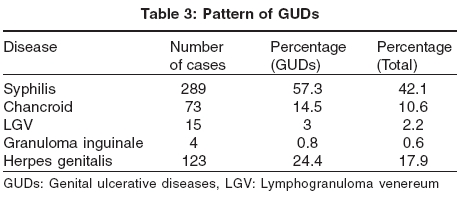
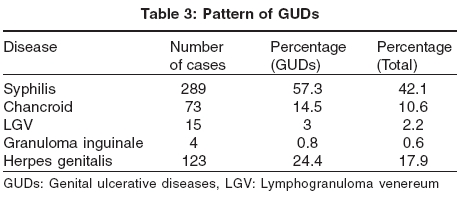
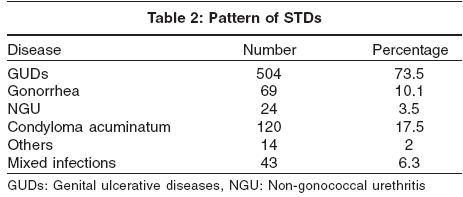
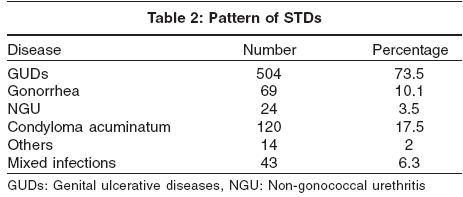
Genital ulcer diseases (GUDs) constituted the maximum number of cases. There were 504 (73.5%) cases of GUDs, followed by 120 (17.5%) cases of condyloma acuminata and 69 (10%) cases of gonorrhea [Table - 2]. Forty-three (6.3%) patients had mixed infections.
Among the patients with GUDs, 289 (57.3%) had syphilis [Table - 3]. This constituted 42.1% of the total cases. Secondary syphilis was the commonest presentation, with 189 (65.39%) patients having this type of syphilis. There were 24 (8.3%) cases of latent syphilis also.
Herpes genitalis was the second commonest disease with 123 (24.4%) cases. This accounted for 17.9% of the total cases. There were 56 cases of first episode infection, and the remaining 67 patients presented with recurrent herpes genitalis. There were 73 (14.5%) patients with chancroid, of which 20 cases were mixed infections and the rest showed features of chancroid alone. Of the patients with chancroid alone, ulcer alone was noted in 41 cases, ulcer with inguinal bubo in 9 cases and bubo alone in 3 cases. Complications, such as phimosis, paraphimosis and balanoposthitis, were seen in only 5 cases. Lymphogranuloma venereum accounted for 15 (3%) cases. There were 4 cases (0.8%) of granuloma inguinale. In one patient, squamous cell carcinoma developed at the site of the ulcer.
There were 69 (10.1%) cases of gonorrhea, most of uncomplicated gonorrhea. Two patients had associated balanitis. One female patient presented with Bartholin′s abscess.
There were 24 (3.5%) cases of non-gonococcal urethritis (NGU); one patient had associated epididymitis.
One hundred and twenty (17.5%) patients had condyloma acuminatum. Two of them had associated balanitis. Trichomonal vaginitis was observed in 2 patients. Four patients had candidiasis. There were 6 cases of scabies and 2 of pediculosis pubis. Forty-three (6.3%) patients had mixed infections, out of which 11 had mixed chancre.
Screening for HIV infection was done in 98 patients; the test was positive in 7 (7.1%) patients. Of these, 5 (71.4%) were males and 2 (28.6%) were females. Four of these patients were married and 3 were unmarried. Associated disease was syphilis in 5 out of the 7 cases. Screening for hepatitis B antigen (HBsAg) was done in 66 cases. Of these, 3 (4.5%) were positive for HBsAg of which 2 cases were associated with syphilis.
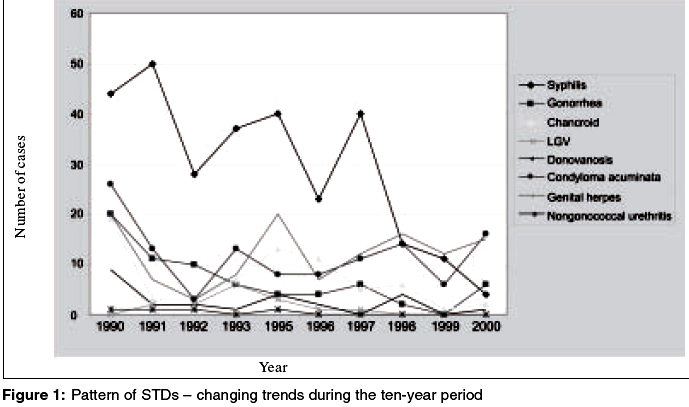
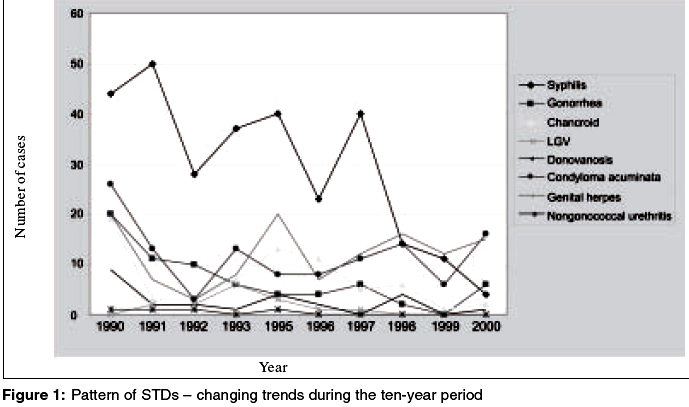
The total number of STDs showed a declining trend from 1990 to 2000. The decline was more striking in the case of bacterial STDs while being less so in the case of viral STDs [Figure - 1].
DISCUSSION
In this study, males outnumbered the females in a ratio of 2.8:1. This pattern is seen in other studies also.[1],[2],[3] This pattern of male preponderance was maintained during the entire period, though the actual ratio varied from year to year. The average age was 27.2 years for male patients and 28 years for females. This could be because in our population the age group of 21 to 30 years is the most sexually active. A similar pattern has been reported by other workers. [2],[3],[4], There was little change in the age profile of the patients during the period of study.
The majority of male patients were married while the reverse was the case with female patients. Though the ratio of married to unmarried patients showed variations in the case of male patients during the different years, there was no definite pattern. Only 9.7% of male patients gave a history of marital exposure alone while in the females the corresponding percentage was 67.6%. This finding shows that the major source of infection for female patients was their spouse while premarital and extramarital exposures were the major sources for males.
The sexual orientation as well as the nature of sexual contact showed more or less the same pattern during the ten years.
Most of the patients presented with genital ulcer diseases. There were 504 (73.5%) cases of GUDs. Of these, syphilis was the most common disease, accounting for 57.3% of the GUDs. Of the different types, secondary syphilis was the commonest. Similar observations have been made by other workers.[3],[4],[5],[6]Granuloma inguinale and lymphogranuloma venereum were found to be rare in this study. Gonorrhea accounted for 10.1% of the total cases. A higher incidence has been reported earlier.[5],[6],[7],
Antibody test for HIV was positive in 7.1% of patients who were tested. Syphilis was the commonest STD found in association with HIV infection. This pattern has been observed by many workers. [1],[2],[3],[4],[5],[6],[7],[8],[9], Increased association of HIV infection and GUD has been reported in various studies.[10],[11],[12] The association of syphilis with HIV infection in this study was found to be statistically significant (p < 0.05). However, further studies are required to confirm this association.
The study demonstrated a marked decline in the total number of patients with STDs during the ten-year period. A similar declining trend in the total number of cases has been observed by Sayal et al.[12] The total number of cases of syphilis showed a decline after 1997. Other bacterial STDs like chancroid and gonorrhea also showed a declining trend, but the fall in numbers was less significant in the case of viral STDs like herpes genitalis and condyloma acuminatum. As a result, towards the end of the study period viral STDs outnumbered bacterial STDs.
Our study shows that there is a decline in the number of patients with STDs attending the hospital. Whether this is due to an actual decrease in the incidence of STDs or due to other factors is uncertain. The increased availability of facilities for treatment of STDs at peripheral centers might be a factor leading to a decline in the number of patients with STDs approaching higher centers like the teaching hospital where this study was undertaken. The emphasis on the syndromic approach to the management of STDs might have increased the accessibility to healthcare for these patients with STDs. Awareness about HIV and fear of contracting the STDs are likely to have influenced the risk-taking behavior of people, thereby reducing the likelihood of being infected with STDs. The high literacy rate of the people in Kottayam and the surrounding areas is a factor favoring this heightened awareness of modified sexual behavior. In addition, the popularization of condoms as a means for preventing HIV and other STDs is likely to have reduced the occurrence of infections. Another factor to be considered is the widespread use of antibacterials, including quinolones and the new macrolides, for the treatment of other diseases. This can result in partial treatment or modified course of the bacterial STDs, thereby leading to apparent reduction in the total number of cases of STDs attending STD clinics as well as a decrease in the proportion of bacterial to viral STDs. The evident decline of the bacterial STDs with an apparent increase of the viral STDs, whatever the reason, is a feature to be noted.
| 1. |
Nair TV, Asha LK, Leelakumari PV. An epidemiological study of sexually transmitted diseases. Indian J Dermatol Venereol Leprol 2000;66:69-72.
[Google Scholar]
|
| 2. |
Mohanty J, Das KB, Mishra C. Clinical profile of sexually transmitted diseases in Cuttack. Indian J Dermatol Venereol Leprol 1995;61:143-4.
[Google Scholar]
|
| 3. |
Kumar B, Bakaya V. Pattern of sexually transmitted diseases in Chandigarh. Indian J Dermatol Venereol Leprol 1987;53:286-91.
[Google Scholar]
|
| 4. |
Shendre MC, Tiwari RR. Social risk factors for sexually transmitted diseases. Indian J Dermatol Venereol Leprol 2002;68:25-7.
[Google Scholar]
|
| 5. |
Kapur LT. Pattern of sexually transmitted diseases in India. Indian J Dermatol Venereol Leprol 1983;49:23-34.
[Google Scholar]
|
| 6. |
Nair BK, Viswam MP, Venugopal BS, Nair PS. An epidemiological study of venereal diseases. Indian J Med Res 1973;61:1697-707.
[Google Scholar]
|
| 7. |
Bansal KN, Khare KA, Upadhyay PO. Pattern of sexually transmitted diseases in and around Udaipur. Indian J Dermatol Venereol Leprol 1988;54:90-2.
[Google Scholar]
|
| 8. |
Karibasappa NA, Babu PN. Incidence of HIV Seropositivity in STD cases. Indian J Dermatol Venereol Leprol 1999;65:214-5.
[Google Scholar]
|
| 9. |
Meena M. Prevalence of HIV antibodies and HBsAg in risk group. Indian J Sex Trans Dis 2003; 24:25-7.
[Google Scholar]
|
| 10. |
Rottingen JA, Cameron DW, Garnett GP. A systematic review of the epidemiologic interaction between classic sexually transmitted diseases and HIV: how much really is known? Sex Transm Dis 2001;28:579-97.
[Google Scholar]
|
| 11. |
Morgan D, Mahe C, Okongo JM, Mayanja B, Whitworth JA. Genital ulceration in rural Uganda. Sexual activity, treatment- seeking behaviour and implication for HIV control. Sex Transm Dis 2001;25:431-6.
[Google Scholar]
|
| 12. |
Sayal SK, Gupta CM, Sanghi S. HIV infection in patients with sexually transmitted diseases. Indian J Dermatol Venereol Leprol 1999;65:131-3.
[Google Scholar]
|
Fulltext Views
2,938
PDF downloads
1,106





