Translate this page into:
A study of skin disorders in patients with primary psychiatric conditions
Correspondence Address:
Pratik Gahalaut
Department of Dermatology, Venereology and Leprology, Kasturba Medical College Hospital, Attavar, Mangalore - 575001
India
| How to cite this article: Kuruvila M, Gahalaut P, Zacharia A. A study of skin disorders in patients with primary psychiatric conditions. Indian J Dermatol Venereol Leprol 2004;70:292-295 |
Abstract
BACKGROUND: The skin occupies a powerful position as an organ of communication and plays an important role in socialization throughout life. The interface between dermatology and psychiatry is complex and of clinical importance. AIMS: To document the incidence of cutaneous disorders in patients with primary psychiatric conditions. METHODS: Three hundred patients with a primary psychiatric condition who had cutaneous disease were entered into the study group. The patients were classified appropriately based on the classification of psychocutaneous disorders. The control group included 300 patients presenting with a skin disorder and without any known psychiatric complaint. RESULTS: The majority of the cases in the study group were in the 3rd-5th decade. In this study, the most common primary psychiatric conditions were manic depressive psychosis (53.33%), depression (36.33%), schizophrenia (8.33%) and anxiety (2%). Of the study group, 68.66% patients had infective dermatoses and the rest had non-infective dermatoses. A high incidence of pityriasis versicolor and dermatophyte infections was noted in males from the study group. Among non-infective dermatoses, 8% had eczema, and psychogenic skin disorders were seen in 4.67% of the study group. Of these, delusions of parasitosis were the commonest (2%) followed by venereophobia (1%). CONCLUSIONS: A statistically significant higher incidence of tinea versicolor and dermatophyte infections was seen in the study group. Delusion of parasitosis was the most common psychogenic skin disorder seen in the study group, followed by venereophobia.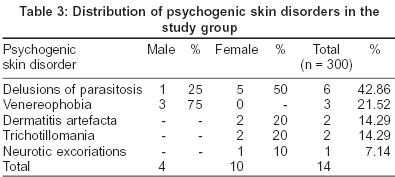


INTRODUCTION
A patient may use the skin to communicate emotional distress. Psychiatric patients often have a defensive need to deny their psychopathology, and seek dermatological care for their prominent cutaneous symptoms.[1] It has been estimated that the effective management of at least one-third of the patients attending the skin department depends, to some extent, upon the recognition of emotional factors.[2] However, there is very little published data on the incidence of dermatoses in patients with primary psychiatric conditions and hence this study was undertaken to document the incidence of cutaneous disorders in patients with primary psychiatric conditions.
METHODS
The study was conducted during a period of 18 months. Three hundred patients with a primary psychiatric condition, who had cutaneous disease, attending the outpatient departments or admitted to the skin and psychiatry wards of Wenlock District Hospital, KMC Hospital Attavar and Fr. Muller′s Hospital, in Mangalore, were entered in the study group. Three hundred patients who presented with a skin disorder, but with no known psychiatric complaint served as the control group. For the classification of psychocutaneous disorders in the study group, the following clinical grouping served as a general guide:[1]
A. Conditions that are primarily psychiatric but which commonly present to dermatologists. e.g. delusions of parasitosis, delusions of body image (e.g. dysmorphophobia, glossodynia, and vulvodynia), phobic states (e.g. venereophobia)
B. Dermatoses primarily emotional in origin e.g. dermatitis artefacta, neurotic excoriations, trichotillomania
C. Dermatoses aggravated by self-induced trauma e.g. lichen simplex chronicus, acne excoriée, prurigo, autoerythrocytic sensitization
D. Dermatoses due to accentuated physiological responses e.g. hyperhidrosis, blushing
E. Dermatoses in which emotional or precipitating factors may be important. e.g. vesicular eczema of the palms and soles, atopic dermatitis, psoriasis, alopecia areata, rosacea, chronic urticaria
A detailed dermatological evaluation was carried out in all patients. Relevant investigations like scraping for fungus and biopsy were done when required. The information was duly documented and compiled. Statistical significance was tested by comparing the means of the study and the control groups to derive the ′P′ Values.[3] Dermatological aspects of all the patients were managed in the department of dermatology and active intervention of the department of psychiatry was sought for the treatment of the psychiatric aspect of the disease.
RESULTS
There were 132 males (44%) and 168 females (56%), giving a male-female ratio of 1:1.27. The majority of the cases (63.33%) were in the third to fifth decades of life. In contrast, most of the patients (50.33%) in the control group fell in the second to fourth decades of life. A higher incidence of dermatoses was seen in the males in the fourth decade while in the females a higher incidence was seen in the third decade. The primary psychiatric conditions [Table - 1] seen in the study were manic depressive psychosis (53.33%), depression (36.33%), schizophrenia (8.33%) and anxiety (2%).
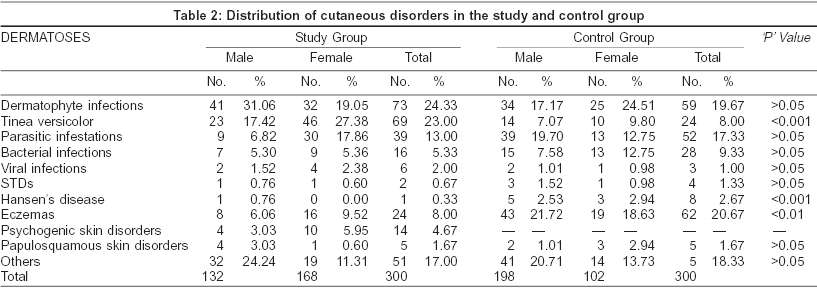
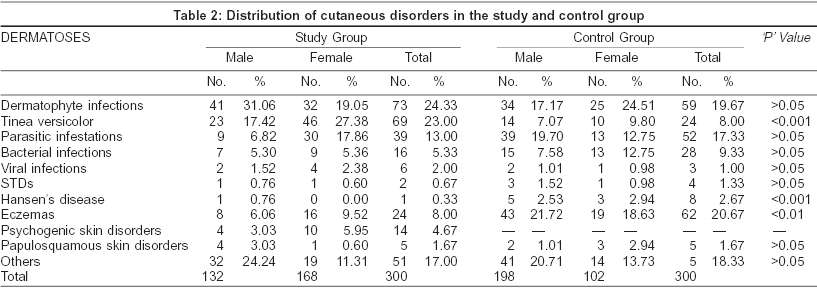
Of the study group, 68.66% patients had infective dermatoses while non-infective dermatoses were seen in 31.33% of patients [Table - 2]. Among infective dermatoses, a higher incidence of dermatophyte infections (31.06%) was noted in the males of the study group. A female preponderance of pityriasis versicolor (27.38%) and parasitic infestations (17.86%) was seen. On the whole, parasitic infestations were seen in 13% of the study group patients. Of these, scabies was present in 7.67%, pediculosis capitis in 4.33%, pediculosis pubis in 0.67% and pediculosis corporis in 0.33% of the patients.
Among non-infective dermatoses, eczemas occurred in 8.00% of the patients, and included lichen simplex chronicus in 3.33% and seborrhoeic dermatitis in 1.67%. This was followed by psychogenic skin disorders (4.67%) and papulosquamous skin disorders (1.67%). In the papulosquamous skin disorders, psoriasis was seen in 3 (1%) patients followed by lichen planus and pityriasis rosea, which were seen in 1 (0.33%) patient each.
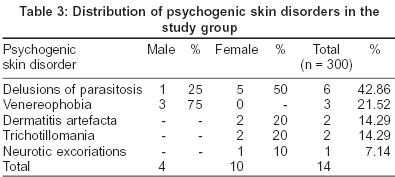
Psychogenic skin disorders [Table - 3] were seen in 14 patients, of which 4 were males and 10 were females. In delusional parasitosis (6/14), the primary psychiatric conditions seen were schizophrenia in 3 patients, depression in 2 patients and bipolar disorder in 1 patient. The primary psychiatric condition in the patients of venereophobia (3/14) and dermatitis artefacta (2/14) was depression. Trichotillomania was seen in 2 female patients, a four-year-old child with subnormal intelligence, and a 43-year-old adult having depression. Neurotic excoriations were seen in a 45-year-old female with underlying depression, who gave history of exacerbation of the lesions during periods of stress.
Among the dermatoses aggravated by self-induced trauma, lichen simplex chronicus (3.33%) was most commonly associated with manic depressive psychosis. Acne excoriée was seen in a 32-year-old female who had depressive psychosis. Prurigo nodularis was seen in 6 female patients with underlying mania and depression.
DISCUSSION
A female preponderance in the study group conformed to finding of other studies.[4] However, the presence of manic depressive psychosis and depression as the most common primary psychiatric conditions in the present study, does not corroborate with other studies,[5] where depression and anxiety were the most common primary psychological disorders.
Dermatophyte infections formed the majority of cutaneous disorders in both the study and control groups. This may be attributed to the humid climate and hence increased sweating. There was a higher incidence of dermatophyte infection in the study group (24.33%) as compared to the control group (19.67%). The difference observed was significant in males (p < 0.001), but did not reach conventional levels of statistical significance in females (p>0.05). In the study group, tinea corporis totaled 11.67% followed by tinea cruris (10.67%). In secondary psychiatric patients the incidence of tinea corporis and tinea cruris was 4.6% and 1.5% respectively.[4]
Pityriasis versicolor was also seen more frequently in the study group (23%) than in the controls (8%). This difference was statistically very highly significant (p < 0.001). It may be attributed to relatively poor personal hygiene, negligence and non-compliance of the patient with the treatment.
Lichen simplex chronicus is one of the dermatoses aggravated or perpetuated by self-induced trauma with a reported incidence of 11.4%.[4] In our study group, lichen simplex chronicus was seen in only 3.33% of the patients. The lower incidence (3.33%) may be because patients with only primary psychiatric disorders were included in this study. Psychiatric disorders, like anxiety neurosis and neurotic depression, are common among people with lichen simplex chronicus.[4],[6] In our study, the most common primary psychiatric condition seen in lichen simplex chronicus was manic depressive psychosis. Usually, both sexes are equally affected in prurigo nodularis,[7] but in our study, all the patients were females, with underlying mania and depression. Acne excoriée has been reported before with phobic states,[8] depression and delusional disorders.[9] In our study it was seen with depressive psychosis.
Delusional parasitosis affects both sexes equally below the age of 50[10],[11] and is associated with schizophrenia,[12] paranoid states, bipolar disorders, depression, anxiety disorders and obsessional states.[2] In this study, delusional parasitosis showed a female preponderance and was seen with schizophrenia in 3 patients, depression in 2 patients and bipolar disorder in 1 patient.
Published reports have shown that patients with overvalued ideas about the possibility of venereal disease, including AIDS and herpes simplex, may be anxious or depressed.[13] In this study all the three patients with venereophobia, had depression.
Dermatitis artefacta is ′an appeal for help′ and the most common psychopathologic factor appears to be an underlying immature personality.[14] Dermatitis artefacta has been reported most commonly in females with the highest onset in adolescence and in the early adult group. In our study, a similar pattern of age and sex distribution was seen. Trichotillomania has a bimodal age of presentation and patients deny that their alopecia is self-induced in up to 43% of the cases.[15] The present study showed similar findings in two cases. Neurotic excoriations, exacerbated by stress, were seen in 0.33% of the study group. Psychosocial stresses have been reported to precede exacerbations of excoriations in 30-98% of patients.[16]
Among papulosquamous disorders psoriasis was seen in 1.0% of the study group. Psoriasis was seen in 10.6% of the secondary psychiatric patients. In our study, the primary psychiatric conditions were anxiety, depression, mania and schizophrenia. Several studies support the importance of psychosocial factors in the onset or exacerbation of psoriatic symptoms in 40-90% of patients.[2],[17],[18] Studies have also found that psoriatics have increased levels of anxiety, depression and aggression.[2] Feelings of stigmatization and other emotional sequelae have also been suggested.[19]
A larger multicentric study, with patients of primary psychiatric disorders, is required to substantiate these results.
| 1. |
Savin JA, Cotterill JA. Psychocutaneous Disorders. In: Champion RH, Burton JL, Ebling FJ. editors. Rook/Wilkinson/Ebling Textbook of Dermatology. 5th Ed. Oxford: Blackwell Scientific Publications; 1992. p. 2482-3.
[Google Scholar]
|
| 2. |
Gupta MA, Gupta AK. Psychodermatology: An Update. J Am Acad Dermatol 1996;34:1030-46.
[Google Scholar]
|
| 3. |
Daly LE, Bourke GJ, McGilvary J. Interpretation and uses of medical statistics. 4th Ed. Oxford: Blackwell; 1991. p. 106.
[Google Scholar]
|
| 4. |
Attah Johnson FY, Mostaghini H. Co - Morbidity between Dermatologic Diseases and Psychiatric disorders in Papua New Guinea. Int J Dermatol 1995;34:244-8.
[Google Scholar]
|
| 5. |
Cotterill JA, Millard LG. Psychocutaneous Disorders. In: Champion RH, Burton JL, Burns DA, Breathnach SM, editors. In: Rook / Wilkinson / Ebling Textbook of Dermatology. 6th Ed. Oxford: Blackwell; 1998. p. 2785-813.
[Google Scholar]
|
| 6. |
Koblenzer CS. Psychiatric syndromes of interest to dermatologists. Int J Dermatol 1993;32:82-8.
[Google Scholar]
|
| 7. |
Burton JL, Holden CA. Eczema, Lichenification and Prurigo. In: Champion RH, Burton JL, Burns DA, Breathnach SM, editors. In: Rook / Wilkinson / Ebling Textbook of Dermatology. 6th Ed. Oxford: Blackwell Science; 1998. p. 629-80.
[Google Scholar]
|
| 8. |
Sneddon J, Sneddon I. Acne excori�e; a protective device. Clin Exp Dermatol 1983;8:65-8.
[Google Scholar]
|
| 9. |
Koo JM, Smith LL. Psychologic aspects of acne. Pediatr Dermatol 1991;8:185-9.
[Google Scholar]
|
| 10. |
Lyell A. Delusion of parasitosis. Semin Dermatol 1983;2:189-95.
[Google Scholar]
|
| 11. |
Lyell A. The Michelson Lecture. Delusion of parasitosis. Br J Dermatol 1983;108:485-99.
[Google Scholar]
|
| 12. |
Hay CG. Dysmorphophobia. Br J Psychiatry 1970;116:399-406.
[Google Scholar]
|
| 13. |
Oates JK, Gomaz J. Venereophobia. Br J Hosp Med 1984;31:435-6.
[Google Scholar]
|
| 14. |
Fabisch W. Psychiatric aspects of Dermatitis Artefacta. Br J Dermatol 1980;102:29-34.
[Google Scholar]
|
| 15. |
Christenson GA, Mackenzie TB, Mitchell JE. Characteristics of 60 adult chronic hair pullers. Am J Psychiatry 1991;148:365-70.
[Google Scholar]
|
| 16. |
Hatch ML, Paradis C, Friedman S, Popkin M, Shalita AR. Obsessive - Compulsive disorder in patients with chronic pruritic conditions: Case studies and discussion. J Am Acad Dermatol 1992;26:549-51.
[Google Scholar]
|
| 17. |
Seville RH. Psoriasis and Stress. Br J Dermatol 1977;97:297-302.
[Google Scholar]
|
| 18. |
Nyfors A, Lemholt K. Psoriasis in children. Br J Dermatol 1975;92:437-42.
[Google Scholar]
|
| 19. |
Hardy GE, Coterrill JA. A study of depression and obsessionality in dysmorphophobic and psoriatic patients. Br J Psychiatry 1982;140:19-22.
[Google Scholar]
|
Fulltext Views
2,412
PDF downloads
951





