Translate this page into:
A study of the clinico-histopathological features of erythematous tender nodules predominantly involving the extremities
2 Department of Pathology, All India Institute of Medical Sciences, New Delhi, India
3 Department of Rheumatology, All India Institute of Medical Sciences, New Delhi, India
Correspondence Address:
Sujay Khandpur
Departments of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi - 110 029
India
| How to cite this article: Maharaja K, Khandpur S, Ramam M, Singh MK, Kumar U, Sharma VK. A study of the clinico-histopathological features of erythematous tender nodules predominantly involving the extremities. Indian J Dermatol Venereol Leprol 2014;80:235-242 |
Abstract
Background: Erythematous tender nodules predominantly involving extremities are frequently encountered in dermatology and rheumatology practice. They are diagnosed based on distinct clinical and histopathological features. However, in clinical situations, considerable overlap is observed that poses a diagnostic challenge. We undertook a study on clinico-histological patterns of inflammatory nodules over extremities. Methods: After detailed history and examination, a preliminary clinical diagnosis was made in 43 cases, followed by skin biopsy from representative nodules. Histological diagnosis made was correlated with clinical features. Results: Of 43 cases, a single clinical diagnosis was made in 25 (58.5%) cases while in the remaining cases more than one diagnosis was considered. On correlating with the histopathological diagnosis, concordance was observed in 51% cases while the remaining showed either histological discordance with clinical diagnosis (14% cases) or were kept in the undecided category (35% cases). Conclusion: Considerable clinico-histological overlap was observed in inflammatory nodules over extremities. Histopathology alone was not helpful in differentiating one entity from another at all times since variable histo-pathological patterns were seen.INTRODUCTION
Inflammatory nodules involving the extremities are frequently encountered in dermatology and rheumatology practice. They may be the primary disease or a manifestation of underlying systemic involvement, infection, drug reaction, connective tissue disease or malignancy. This group of dermatoses has been classified based on clinical histopathological, and immunopathological features. [1],[2] Clinico-pathological features of each entity have also been evaluated independently. [3] However, considerable clinical and histopathological overlap exists making it diagnostically challenging for the treating physician. We undertook this study to evaluate histopathological patterns and establish clinico-pathological correlation in patients presenting with inflammatory nodules over extremities to our large tertiary care teaching hospital in north India.
METHODS
It was a prospective study conducted between October 2009 and June 2011. The study was cleared by the ethics committee at ourinstitute and informed consent from all patients was obtained. Consecutive patients with tender erythematous nodules predominantly involving the extremities, excluding pyogenic infections and erythema nodosum leprosum, were subjected to detailed history followed by a thorough clinical examination. A clinical diagnosis was made by two dermatologists based on characteristic clinical features described for each entity (Annexure 1). The features included 1) sites of predilection of nodules over extremities, 2) course of disease, 3) sequelae of lesions and 4) other associated signs and symptoms. If the clinical manifestations did not strictly conform to one particular disease and showed overlapping features, differential diagnoses were kept instead of a single diagnosis.
A 4-mm skin punch biopsy upto the depth of subcutis was obtained from a representative and active nodule and stained with hematoxylin and eosin (H and E) stain in all cases and special stains like Verhoeff-van Gieson (VvG) (to differentiate between an affected arteriole as in polyarteritis nodosa versus venule in superficial thrombophlebitis) AFB, PAS, Alcian blue-PAS and Giemsa stain in appropriate cases.The histopathological features were independently evaluated by two dermatopathologists independently who were blinded to clinical information to eliminate bias and a clinico-pathological correlation undertaken. The correlation between clinical diagnosis and histopathological findings was evaluated as: (1) Concordance - Histopathological findings consistent with any one of the clinical diagnosis made, (2) Discordance - histopathological findings specific to another disease which was not considered in clinical diagnosis and (3) Undecided - Histopathological findings not specific to any particular disorder.
RESULTS
A total of 43 patients were recruited. There were 21 men and 22 women with ages ranging from 11-65 years (mean ± SD: 37.41 ± 12.7 years). In 25 cases, one clinical diagnosis was considered, while differential diagnoses were kept in the remaining 18 cases. Of 25 cases in whom a single condition was suspected, there were 17 cases of erythema nodosum [6 men and 11 women, ages ranging from 13-65 years, mean ± SD: 40.41 ± 12.52 years], 3 of erythema induratum, 2 each of lupus panniculitis and cutaneous medium vessel vasculitis and one case of superficial thrombophlebitis. Overall, the clinical diagnosis of erythema nodosum was considered in 30 (70%) cases, cutaneous medium vessel vasculitis in 15 (35%), erythema induratum in 12 (28%), lupus panniculitis in 5 (11.6%), superficial thrombophlebitis in 3 (7%), subcutaneous panniculitic T-cell lymphoma (SPTCL) in 3 (7%), and other panniculitides in one patient (2.3%) each [Table - 1].
The duration of disease at the time of presentation was 8 days to 23 years (mean 2.4 ± 4.7 years, median 5 months). The period for which the nodule had been present until biopsy was taken ranged from 4 days to 20 months (mean 36 ± 95 days, median 12 days).
After histopathological examination, concordance between initial clinical impression and histological diagnosis was found in 22 of 43 cases (51%) while 21 (49%) were in the discordant (14%) and undecided category (35%). In 12 (40%) of 30 cases (40%), 5 (33.3%) of 15 cases of cutaneous medium vessel vasculitis, 3 (60%) of 5 cases of lupus panniculitis, 1 (33.3%) of 3 cases of SPTCL 2 (16.7%) of 12 erythema induratum and 0 of 3 cases of superficial thrombophlebitis, the histolopathological impression correlated with preliminary clinical diagnosis.[Table - 1]. Histological patterns observed in our cases and their correlation with clinical diagnoses are mentioned in [Table - 2] and [Figure - 1], [Figure - 2], [Figure - 3], [Figure - 4], [Figure - 5].
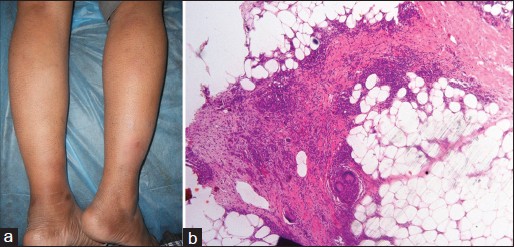 |
| Figure 1: (a) Preliminary clinical diagnosis: Medium vessel vasculitis/Erythema nodosum (b) Photomicrograph shows septal panniculitis with granulomatous infi ltrate consistent with erythema nodosum (H and E, ×10) |
 |
| Figure 2: (a) Preliminary clinical diagnosis: Erythema nodosum (b) Photomicrograph shows granulomatous lobular panniculitis with small vessel vasculitis consistent with erythema induratum (H and E, ×10) |
 |
| Figure 3: (a) Preliminary clinical diagnosis: Medium vessel vasculitis with background livido reticularis. (b) Congestion of medium caliber vessel, extravasation of RBCs with dense acute and chronic infl ammation in the vessel wall consistent with medium vessel vasculitis (H and E, ×40) |
 |
| Figure 4: (a) Preliminary clinical diagnosis: Superficial thrombophlebitis (tender cord-like thickenings on the legs) (b) Thrombus formation in medium sized vessel with dense chronic inflammation in the vessel wall (H and E, ×100) (c) Photomicrograph shows presence of internal elastic lamina with scant elastic fi bres in tunica media suggestive of arteriole. Diagnosis- medium vessel vasculitis (VvG, ×100) |
 |
| Figure 5: (a) Preliminary clinical diagnosis: Lupus panniculitis - multiple areas of subcutaneous atrophy preceded by nodules on right arm (b) Septal and lobular panniculitis with sclerosis and dense lobular infi ltrate of lympho-histiocytes and plasma cells suggestive of lupus panniculitis (H and E, ×40) |


Histopathologically diagnosed cases were again analysed to assess the various clinical patterns that emerged. In histopathologically confirmed erythema nodosum (n = 14), classically described clinical features of erythema nodosum (involvement of predominantly the anterior aspect of legs resolving with hyperpigmentation in 7 days to 2 months) were observed in 12 (85.7%) cases, while atypical features like linear distribution of nodules and involvement of predominantly the posterior aspect of legs in 2 (14.3%) each and persistence of nodules (presence for >2 months and resolving with hyperpigmentation only) in one (7%) case was also observed. Two (50%) of 4 cases with confirmed erythema induratum had lesions predominantly over the posterior legs while the other two developed lesions predominantly on the anterior legs along with lesions on arms, thighs, forearms and abdomen. In three (75%) of four cases lesions resolved with hyperpigmentation only in 2 to 12 weeks, while in one patient, the nodules ulcerated and healed with atrophy and scarring. In all seven cases with confirmed cutaneous medium vessel vasculitis, nodules occurred on both anterior and posterior aspect of limbs with predilection for sites around ankles and wrist in three (43%) cases and nodules resolved with hyperpigmentation only in a week to 2 to 6 months in six (85.7%) patients. Linear arrangement of nodules (three cases), association with livido reticularis (one case) and ulceration (one case) were the other features observed. Lupus panniculitis involved the proximal extremities with a few nodules occurring on distal extremities and face which were either persistent or subsided with atrophy or hyperpigmentation in 1 to 4 months. The only case of lupus panniculitis/subcutaneous panniculitic T-cell lymphoma overlap involved proximal extremities and trunk and the nodules resolved with subcutaneous atrophy or hyperpigmentation in 1-3 months.
DISCUSSION
We analysed the clinico-histopathological patterns of erythematous tender nodules predominantly involving the extremities in 43 cases.
After initial clinical evaluation, in 25 (59%) cases, a single diagnosis was considered since these patients showed classical manifestations of the disease while in the remaining 18 (41%), we kept more than one diagnosis because of overlapping clinical features. After histopathological examination, final diagnoses made were erythema nodosum in 14 (32.6%) cases, erythema induratum in 4 (9.3%), cutaneous medium vessel vasculitis in 7 (16.3%), lupus panniculitis in 2 (4.7%) and lupus panniculitis/subcutaneous panniculitic T-cell lymphoma overlap in one (2.3%) case while 15 (35%) cases were in the undecided category. Niemi et al.,[4] in a series of 82 cases of inflammatory leg nodules, made clinical diagnoses of erythema nodosum, erythema nodosum migrans, erythema induratum, and non-definitive panniculitis in 42.7%, 13.4%, 13.4% and 30.5% cases, respectively. Cho et al.,[5] in their series of 134 cases, based on clinicopathological findings, responsiveness to various therapeutic agents and clinical course found predominance of erythema induratum (39.5%), erythema nodosum (13.4%), and erythema nodosum-like lesions of Behcet′s disease (29.9%) respectively, besides superficial thrombophlebitis, cutaneous polyarteritis nodosa, sarcoidosis, and cutaneous lymphoma. In 55 cases of panniculitides involving legs, Chopra et al., [6] made clinical diagnosis of erythema nodosum, atypical erythema nodosum, cellulitis, unclassified panniculitis, and erythema induratum in decreasing order.
Of 17 (40%) cases where erythema nodosum was the only clinical diagnosis in our study, histopathology correlated with clinical suspicion in 8 (47%), in 4 (23.5%) there were features of erythema induratum, medium vessel vasculitis and normal histology and remaining 5 (29%) cases showed non-specific lobular panniculitis or mixed septal-lobular panniculitis. Overall, of 30 cases suspected of this condition, histopathological concordance was found in 40% and discordance in 27% cases. A few clinically suspected cases of erythema nodosum showed some infiltrate in the center of the lobules along with septal thickening and inflammation and were kept in the undecided category as the final diagnosis. It is probable that these were truly cases of erythema nodosum since at times the condition may appear lobular, as we see only two dimensions of a biopsy. In a study by Yi et al.,[7] 72% of erythema nodosum cases had predominantly septal panniculitis while 4.2% and 23% had lobular panniculitis and mixed septal-lobular panniculitis respectively. Similarly in the Niemi et al.,[4] study, clinico-histopathological concordance was observed in 77% cases. In four clinically diagnosed erythema nodosum cases, Thurber et al.,[3] observed neutrophilic lobular panniculitis with suppuration and vasculitis in two cases while the other two cases showed lobular panniculitis and septal-lobular panniculitis with vasculitis in the first biopsies. All these cases on repeat biopsy showed predominantly septal panniculitis. Unusual clinical patterns in histopathologically confirmed erythema nodosum in our study included involvement of non-classical sites (posterior > anterior leg in 14.3% cases), persistence of lesions and unusual arrangement (linear arrangement of nodules in 7% cases). Involvement of atypical sites such as thighs, upper limbs and trunk have been observed in various studies in 11-17% cases. [8],[9],[10]
In three (6.9%) cases, erythema induratum was our only clinical diagnosis; the histopathological patterns observed in these cases were septal and lobular panniculitis in two cases and predominantly septal panniculitis (consistent with erythema nodosum) in one case. Overall, of 12 cases suspected of this condition, histopathological concordance was seen in two (16.7%) and discordance in three (25%) cases, while seven cases were in the undecided category. We used a strict definition of lobular panniculitis (granulomatous, lymphohistiocytic) with vasculitis for erythema induratum and did not consider only granulomatous lobular panniculitis without evidence of vasculitis (seen in another four cases) compatible with this diagnosis. Niemi et al.,[4] observed the following histopathological patterns in 11 cases of erythema induratum: lobular panniculitis with vasculitis in four cases (36%) and lobular panniculitis with epithelioid cell or palisading granulomas without vasculitis in the remaining seven (64%) cases. Yi et al.,[7] observed predominantly lobular panniculitis in 10 of 16 cases and mixed septal-lobular panniculitis in 6 of 16 cases with 15 of 16 cases showing associated vasculits in clinically diagnosed erythema induratum. In a retrospective study, Segura et al.,[11] observed vasculitis in 90% cases of erythema induratum while in the remaining it could not be demonstrated despite serial sections. In our study, in histopathologically confirmed erythema induratum cases (n = 4), lesions were observed at atypical sites like anterior leg, thighs, arm, forearm, and abdomen, a finding that corroborates those of other studies. [12] Mascaro et al., and Requena et al., have mentioned that most erythema induratum lesions have a tendency to ulcerate and resolve within a few months with hyperpigmentation and atrophic pigmented scars. [2],[12] However, we observed lesions resolving with hyperpigmentation within 2-12 weeks in 3 of 4 cases and ulceration occurring in one patient only.
In our study, in 2 (4.7%) cases, lupus panniculitis was the only clinical diagnosis and the diagnosis was suspected in 5 (11.6%) cases overall. Histopathology consistent with this condition was observed in both (100%) cases where this was the only clinical diagnosis and in 3 (60%) cases where it was included as a differential diagnosis. No case showed lymphoid follicle formation or epidermal and dermal changes of lupus erythematosus. Sanchez et al.,[13] observed sufficient histopathological features to make a diagnosis of lupus panniculitis in 72% of cases; these changes included hyaline fat necrosis, fibrin deposits and a mixture of neutrophils, plasma cells and histiocytes in 69% of cases, lymphoid nodules in 55% of cases and epidermal and dermal changes in 24% and 6.9% of cases respectively. Ng et al.,[14] observed fat necrosis in all 12 cases of lupus panniculitis, lobular and paraseptal inflammation with lymphocytic vasculitis in four (33.3%) and dermal changes of lupus erythematosus in eight (66.7%) cases but no lymphoid nodule formation. In our histopathologically confirmed lupus panniculitis cases, the majority had a classical clinical presentation (involving proximal extremities, face) with a few developing nodules over the distal extremities and trunk, a finding that has also been reported in previous studies. [15] We had clinically suspected subcutaneous panniculitic T-cell lymphoma in three (6.9%) cases, of which one case (33.3%) showed a histolopathogical pattern overlapping with lupus panniculitis and the other two showed features of erythema induratum and resolving panniculitis. Pincus et al.,[16] have described 5 cases of lupus panniculitis/subcutaneous panniculitic T cell lymphoma overlap that showed clinical features of lupus panniculitis in some cases and serological and/or extracutaneous end-organ abnormalities of SLE in all cases. Histologically, all cases showed lobular infiltration by atypical lymphocytes with evidence of dermal changes of lupus erythemaosus in three cases and lymphoid nodules containing CD20+ cells in the lobules in one case.
In two (4.7%) cases, cutaneous medium vessel vasculitis was our single clinical diagnosis; this was corroborated histologically in one (50%) case while the other case was consistent with erythema nodosum. Overall, this diagnosis was suspected in 15 (34.9%) cases with histological agreement in 5 (33.3%) and discordance in 33% cases. Histologically confirmed cases of cutaneous medium vessel vasculitis (n = 7, 16.3%) had preferential involvement around ankles and wrist in three (43%) cases, with lesions resolving with hyperpigmentation alone in upto 6 months in a majority of cases with only one (14.3%) case developing ulceration. Linear arrangement of nodules was seen in three (43%) cases and associated livido reticularis in one (14.3%) case. Of 79 cases of cutaneous polyarteritis nodosa described by Daoud et al.,[17] lesions occurred over legs, arms, and trunk in 97.5%, 32.9% and 7.6% cases, respectively, with livido reticularis and ulceration noticed in a greater number of cases than in our series. Ishiguro et al.,[18] also reported livido reticularis and ulceration in a higher number of patients than we found in our study.
In our study, superficial thrombophlebitis was considered as the only clinical diagnosis in one case and was suspected in three (6.9%) cases. Two of these cases showed histopathological findings of medium vessel vasculitis. Verhoeff-van Gieson (VvG) stain was suggestive of an arteriole in both these cases. The third case showed histological features of erythema nodosum. VvG stain was very helpful in differentiating medium vessel vasculitis from superficial thrombophlebitis in cases that showed inflammation in the vessel wall and thrombus in the lumen but no fibrinoid necrosis. To tell the difference between arterioles and venules, we used the findings described by Chen et al.,[19] who reported that the scanty distribution of elastic fibers in the muscular wall of arterioles compared to the distribution between smooth muscle bundles in venules was more reliable than the presence or absence of the internal elastic lamina or the pattern of smooth muscle in the vessel wall.
Our study suggests a great degree of overlap in this group of dermatoses. It was limited by the fact that biopsies were taken only once in the majority of cases and serial sections of the biopsies were not obtained. By undertaking biopsies at different time intervals in each case or obtaining multiple sections, we may have been able to arrive at a conclusive diagnosis in cases that could not be categorized.
In conclusion, inflammatory leg nodules are a challenging group of disorders. In our attempt to establish a clinico-pathological correlation, we observed that histopathology alone was not helpful in differentiating one entity from another at all times since variable histopathological patterns were observed. Further studies with a larger sample size for each of the groups are required to confirm these findings and to validate the new clinical patterns observed in this study.

| 1. |
Requena L, Yus ES. Panniculits. Part I. Mostly septal panniculitis. J Am Acad Dermatol 2001;45:163-83.
[Google Scholar]
|
| 2. |
Requena L, Sánchez Yus E. Panniculits. Part II. Mostly lobular panniculitis. J Am Acad Dermatol 2001;45:325-61.
[Google Scholar]
|
| 3. |
Thurber S, Kohler S. Histopathologic spectrum of erythema nodosum. J Cutan Pathol 2006;33:18-26.
[Google Scholar]
|
| 4. |
Niemi KM, Forstrom L, Hannuksela M, Mustakallio KK, Salo OP. Nodules on the legs. A clinical, histological and immunohistological study of 82 patients representing different types of nodular panniculitis. Acta Derm Venereol 1977;57:145-54.
[Google Scholar]
|
| 5. |
Cho KH, Kim YG, Yang SG, Lee DY, Chung JH. Inflammatory nodules of the lower legs: A clinical and histological analysis of 134 cases in Korea. J Dermatol 1997;24:522-9.
[Google Scholar]
|
| 6. |
Chopra R, Chhabra S, Thami GP, Punja RP. Panniculitis: Clinical overlap and the significance of biopsy findings. J Cutan Pathol 2010;37:49-58.
[Google Scholar]
|
| 7. |
Yi SW, Kim EH, Kang HY, Kim YC, Lee ES. Erythema Nodosum: Clinicopathologic correlations and their use in differential diagnosis. Yonsei Med J 2007;48:601-8.
[Google Scholar]
|
| 8. |
Garcia-Porrua C, Gonzalez-Gay MA, Vazquez Caruncho M, López-Lazaro L, Lueiro M, Fernández ML, et al. Erythema nodosum: Etiologic and predictive factors in defined population. Arthritis Rheum 2000;43:584-92.
[Google Scholar]
|
| 9. |
Mert A, Kumbasar H, Ozaras R, Erten S, Tasli L, Tabak F, et al. Erythema nodosum: An evaluation of 100 cases. Clin Exp Rheumatol 2007;25:563-70.
[Google Scholar]
|
| 10. |
de Almeida Prestes C, Winkelmann RK, Su WP. Septal granulomatous panniculitis: Comparison of the pathology of erythema nodosum migrans (migratory panniculitis) and chronic erythema nodosum. J Am Acad Dermatol 1990;22:477-83.
[Google Scholar]
|
| 11. |
Segura S, Pujol RM, Trindade F, Requena L. Vasculitis in erythema induratum of Bazin: A histopathologic study of 101 biopsy specimens from 86 patients. J Am Acad Dermatol 2008;59:839-51.
[Google Scholar]
|
| 12. |
Mascaro JM Jr, Baselga E. Erythema induratum of bazin. Dermatol Clin 2008;26:439-45.
[Google Scholar]
|
| 13. |
Sanchez NP, Peters MS, Winkelmann RK. The histopathology of lupus erythematousus panniculitis. J Am Acad Dermatol 1981;5:673-80.
[Google Scholar]
|
| 14. |
Ng PP, Tan SH, Tan T. Lupus erythematosus panniculitis: A clinicopathologic study. Int J Dermatol 2002;41:488-90.
[Google Scholar]
|
| 15. |
Massone C, Kodama K, Salmhofer W, Abe R, Shimizu H, Parodi A, et al. Lupus erythematosus panniculitis (lupus profundus): Clinical, histopathological, and molecular analysis of nine cases. J Cutan Pathol 2005;32:396-404.
[Google Scholar]
|
| 16. |
Pincus LB, LeBoit PE, McCalmont TH, Ricci R, Buzio C, Fox LP, et al. Subcutaneous panniculitis-like T-cell lymphoma with overlapping clinicopathologic features of lupus erythematosus: Coexistence of 2 entities? Am J Dermatopathol 2009;31:520-6.
[Google Scholar]
|
| 17. |
Daoud MS, Hutton KP, Gibson LE. Cutaneous periarteritis nodosa: A clinico-pathological study of 79 cases. Br J Dermatol 1997;136:706-13.
[Google Scholar]
|
| 18. |
Ishiguro N, Kawashima M. Cutaneous polyarteritis nodosa: A report of 16 cases with clinical and histopathological analysis and a review of the published work. J Dermatol 2010;37:85-93.
[Google Scholar]
|
| 19. |
Chen KR. The misdiagnosis of superficial thrombophlebitis as cutaneous polyarteritis nodosa: Features of the internal elastic lamina and the compact concentric muscular layer as diagnostic pitfalls. Am J Dermatopathol 2010;32:688-93.
[Google Scholar]
|
Fulltext Views
4,829
PDF downloads
2,409





