Translate this page into:
Acquired generalised cutis laxa with visceral involvement in a patient with rheumatoid arthritis and monoclonal gammopathy of uncertain significance
Corresponding author: Dr. Vishal Gupta, All India Institute of Medical Sciences, New Delhi, India. doctor.vishalgupta@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Manandhar K, Lal A, Manchanda S, Gupta V. Acquired generalised cutis laxa with visceral involvement in a patient with rheumatoid arthritis and monoclonal gammopathy of uncertain significance. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_824_2023
Dear Editor,
Cutis laxa is a rare disorder of elastic tissue characterised by lax pendulous skin and variable systemic involvement. It may be inherited or acquired; the acquired forms being more prevalent.1,2 We report acquired generalised cutis laxa in a patient with rheumatoid arthritis, who was subsequently found to have visceral involvement and monoclonal gammopathy of uncertain significance.
A 38-year-old man consulted us for generalised ‘loosening’ of the skin. He had first noticed it on the face 3 years ago and it gradually progressed to involve other sites, particularly axillae and groins. His past medical history was relevant for rheumatoid arthritis (RA) of 9 years’ duration, being treated with intermittent use of oral complementary and alternative medicine with a waxing and waning course. The family history was non-contributory. General physical examination was unremarkable. Mucocutaneous examination was striking for generalised laxity and sagging of the skin with poor elastic recoil, particularly prominent over the chest, axillae, and groins [Figures 1a and 1b]. With a diagnosis of generalised acquired cutis laxa, the patient was evaluated for internal organ involvement and any underlying associated conditions. His routine haemogram and biochemistry were within normal limits. Serum titres for RA factor (96.9 IU/mL, reference <14 IU/mL) and CCP (58.2 U/mL, reference <5 U/mL) were raised. Chest X-ray showed emphysematous changes in bilateral lung lower lobes [Figure 2a]. High-resolution computed tomography (HRCT) of the chest showed centrilobular emphysematous changes in bilateral upper lobes, panlobular emphysematous changes in bilateral lower lobes, and fibrotic opacities in the left lower lobe [Figures 2b and 2c]. Pulmonary function test results FEV1 22%, FVC 43%, FEV1/FVC 51%) were suggestive of an obstructive lung disease. Micturating cystourethrogram and retrograde urethrogram revealed an anterior urethral diverticulum [Figures 3a–3c]. Computerised tomographic (CT) enterography and echocardiography were normal. Serum electrophoresis revealed an M band (0.69g/dl, 10.2%), while serum-free light chain assay showed an elevated serum-free kappa light chain (156.29 mg/L, reference 3.3–19.4 mg/L) and lambda light chain (378.38 mg/L, reference 5.710–26.3 mg/L) but a normal kappa/lambda ratio (0.41, reference 0.26–1.65), suggestive of monoclonal gammopathy of uncertain significance. Positron emission tomography (PET) scan did not reveal any site with increased metabolic uptake. Following a rheumatology- consult for RA, the patient was started on oral weekly methotrexate (15 mg) and daily naproxen (500 mg). He was counselled about the nature and course of his skin disease and was advised an annual follow-up.
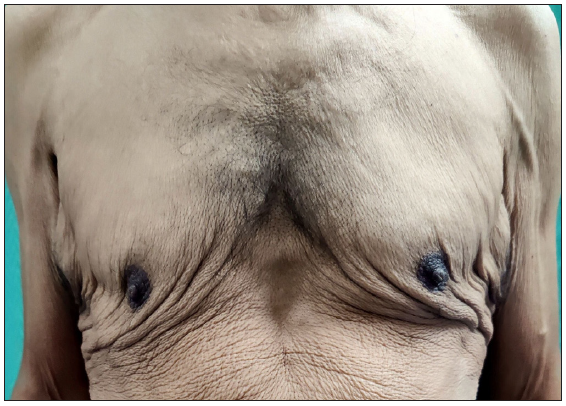
- Generalised skin laxity on the trunk with loose hanging skin on the chest.

- Lax skin on the axilla.

- Bilateral hyperinflated lung fields with bullous emphysematous changes in bilateral lower lobes (white arrows).

- Coronal reformatted lung window images of HRCT chest showing centrilobular emphysematous changes in bilateral upper lobes (*), panlobular emphysematous changes in bilateral lower lobes (arrowheads)

- Coronal reformatted lung window images of HRCT chest showing l fibrotic opacities in left lower lobe (dotted arrow).

- Retrograde urethrogram shows retrograde filling in the smooth tubular dilatation of the left Cowper duct (white arrow), likely a simple Cowper duct syringocele.

- Micturating cystourethrogram. Full bladder spot reveals normal bladder capacity and outline (*).

- Micturating cystourethrogram. Full bladder reveals normal posterior urethra (dotted arrow) and the left simple Cowper duct syringocele (white arrow).
Cutis laxa is characterised by loose hanging skin that can be stretched easily and returns to its original position slowly (poor elastic recoil). Systemic involvement may be present in a variable proportion of patients. The underlying defect is an abnormal elastic fibre network in the skin and internal organs. Inherited forms can have various modes of transmission with overlapping clinical expressions and occur due to mutations in elastin, fibulin 5 and 4, or ATP6V0A2 genes. Acquired forms of cutis laxa are more common and have a later onset, usually in adulthood.1,2 Diagnosis is largely clinical, based on distinctive cutaneous findings. Generalised loose easily stretchable skin is also a characteristic feature of Ehlers Danlos syndrome, but the elastic recoil is normal.3 Skin biopsy in cutis laxa typically shows loss or fragmentation of elastic fibres, though normal histopathology does not exclude the diagnosis.4
Acquired cutis laxa can be classified as type I (generalised) or type II (localised). Generalised form often starts on the face (‘old man’ appearance) and progresses cephalocaudally. Aetiology remains uncertain, but several associations have been reported, including drugs, inflammatory skin and systemic diseases, amyloidosis, infections, and malignancies. There are reports of cutis laxa in patients with inflammatory arthritis, including a report of acral localised cutis laxa in a patient with long-standing RA. About half of the cases are associated with inflammatory dermatoses.1–3 Marshall syndrome is a distinct type of localised cutis laxa affecting children and occurs due to post-inflammatory elastolysis after neutrophilic dermatosis.4 Some patients with acquired disease may have internal organ involvement, such as emphysema, bronchiectasis, intestinal and urinary tract diverticula, genital prolapse, and vascular dilatations.1,2 In a series of 14 cases (9 males: 5 females, mean age- 56 years) of acquired cutis laxa with monoclonal gammopathy (four had multiple myeloma, six had monoclonal gammopathy of uncertain significance and four had heavy chain deposition disease), systemic manifestations included emphysema (n = 8), gastrointestinal (n = 6) and genitourinary involvement (n = 1).5
There is no effective treatment, though excision of lax skin can produce temporary cosmetic improvement. In contrast to the Ehlers–Danlos syndrome, cutis laxa does not involve vascular fragility. Therefore, surgery is not contraindicated as it does not adversely affect wound healing. Anecdotal reports have shown benefits with procedures including rhytidectomy and blepharoplasty but the effect is mostly temporary, and repeated procedures may be needed.6
To conclude, we present this case for its rarity. Dermatologists should perform a careful screening for underlying internal organ involvement and associated conditions [Table 1], including monoclonal gammopathies.
| Triggers and associations |
|---|
|
Past medical history of urticarial eruption, inflammatory skin disease, or any systemic illness History of significant weight loss, B symptoms Drug history Serum and protein electrophoresis, serum-free light chain assay ANA, RA factor, anti-CCP, and alpha1 antitrypsin levels (depending on clinical clues) |
| Systemic involvement |
|
Pulmonary involvement: Chest X-ray, HRCT, Pulmonary function test Cardiac involvement: ECG, Echocardiography, Computersied tomographic (CT) angiography Gastrointestinal involvement: Ultrasound abdomen, Colonoscopy, CT enterography Urogenital involvement: X-ray KUB, Retrograde and micturating cystourethrography |
ANA: Antinuclear antibody; RA factor: Rheumatoid factor; KUB: Kidney, ureter, bladder; Anti-CCP: Anti cyclic citrullinated peptide; HRCT: High resolution computed tomography, ECG: electrocardiography.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Acral localized acquired cutis laxa associated with rheumatoid arthritis. J Am Acad Dermatol. 2002;46:128-30.
- [CrossRef] [PubMed] [Google Scholar]
- Acquired cutis laxa type II (Marshall syndrome) in a 3-month-old boy. Pediatr Dermatol. 2022;39:312-3.
- [CrossRef] [PubMed] [Google Scholar]
- Cutis laxa associated with monoclonal gammopathy: 14 new cases and review of the literature. J Am Acad Dermatol. 2018;79:945-7.
- [CrossRef] [PubMed] [Google Scholar]
- Acquired localized cutis laxa: A case report and the role of plastic surgery. Indian J Dermatol. 2019;64:55-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





