Translate this page into:
Acral angioosteoma cutis: A rare case
2 Department of Pathology, Okmeydanı Training and Research Hospital, İstanbul, Turkey
3 Department of Pathology, Ağrı State Hospital, Ağrı, Turkey
4 Department of Pathology, Kırklareli State Hospital, Kırklareli, Turkey
Correspondence Address:
Senay Erdogan-Durmus
Çat avenue, Erzurum Region Training and Research Hospital 2nd floor, Department of Pathology, Erzurum
Turkey
| How to cite this article: Erdogan-Durmus S, Ozekinci S, Yarikkaya E, Erzurumluoglu N. Acral angioosteoma cutis: A rare case. Indian J Dermatol Venereol Leprol 2018;84:685-686 |
Abstract
Acral angioosteoma cutis is a rare and benign cutaneous lesion clinically characterized by an exophytic growth resembling pyogenic granuloma on the acral skin; first described in 2006. Its pathogenesis is still unclear while well-formed capillaries, pale stroma, bland fibroblast-like cells, and multiple tiny spicules of woven bone constitute the histological hallmarks. Here, we present a case of acral angioosteoma cutis in a 34-year-old man to increase awareness regarding this rare condition.
Introduction
Acral angioosteoma cutis is rare condition clinically mimicking pyogenic granuloma which was first described in 2006 as a benign tumor demonstrating vascular proliferation, calcification, or ossification.[1],[2]
It occurs on the acral skin resembling pyogenic granuloma, however their histopathological features are widely different.[3] Lobular capillary proliferation, a typical histopathological feature of pyogenic granuloma is absent in acral angioosteoma cutis. Metaplastic cutaneous ossification is associated with multiple skin diseases and inflammatory conditions such as scars, nevi, basal cell carcinomas, pilomatricomas, chondroid syringomas, and venous stasis. It is rarely associated with vasoproliferative diseasessuch as hemangiomas and pyogenic granulomas.[1],[4]
Case Report
A 34-year-old man presented with a 1.5 × 1.5 cm, solitary, ulcerative, erythematous nodule on his left thumb which developed approximately 6 months following trauma. The patient also complained of had mild pain in the affected area. The past history was unremarkable. Clinically, the lesion was suspected to be pyogenic granuloma or proliferative granulation tissue. Subsequently excision biopsy was performed. Almost the entire skin surface was ulcerative while the cut surface was hemorrhagic with focal calcification [Figure - 1]. Histopathology revealed epithelial ulceration, dilated capillary network, and chronic inflammatory infiltrate comprised of lymphocytes, eosinophils, and plasma cells. Deeper areas showed definite bony trabeculae, foci of basophilic calcification along with transitions of bony vascular components [Figure - 2]. Vascular network showed positive CD34 staining while the bony component showed positive von Kossa staining [Figure - 3]a and [Figure - 3]b. These findings supported a diagnosis of acral angioosteoma cutis.
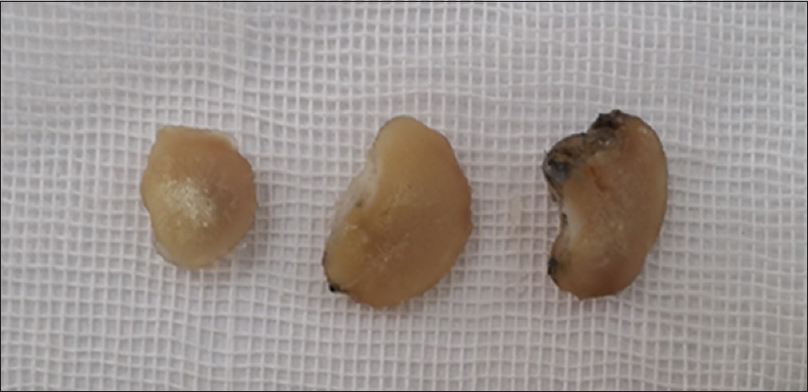 |
| Figure 1: Macroscopic appearance of lesion |
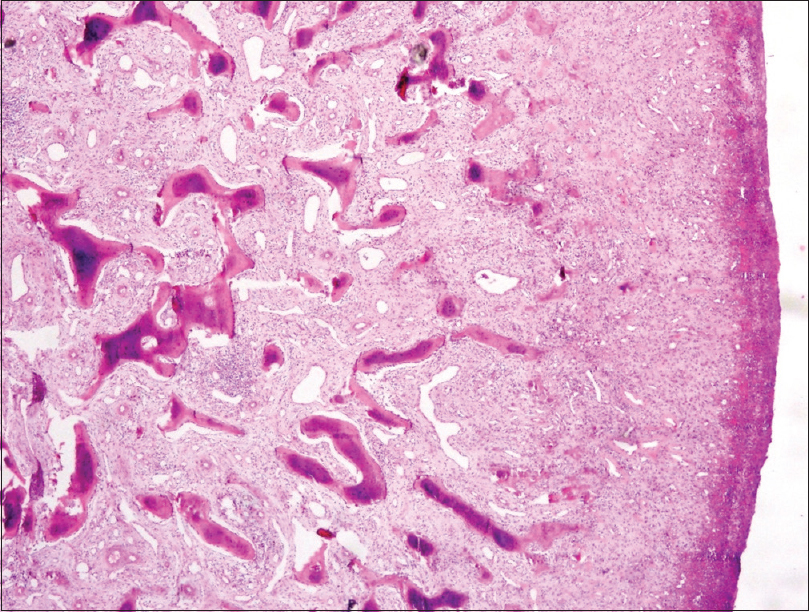 |
| Figure 2: Dermal proliferation of bony spicules and scattered capillaries without lobular pattern (H and E, ×40) |
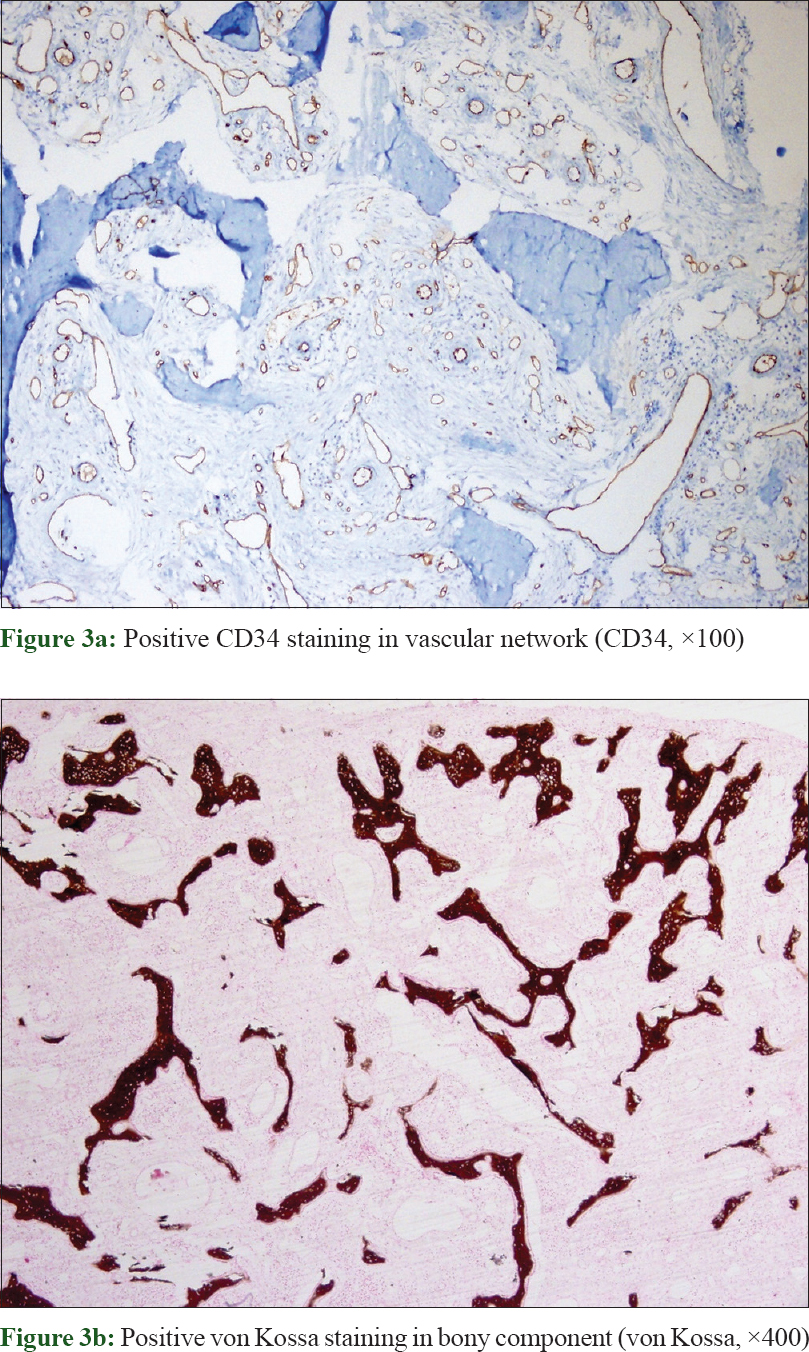 |
| Figure 3: |
Discussion
Acral angioosteoma cutis has been reported sparsely in the English literature. These reports have reflected a wide age range ranging from 12 – 72 years with a female preponderance.[1],[2],[3],[5] Interestingly, our patient was a 34-year-old man. Although acral angioosteoma cutis can involve both toes and fingers, most of the reported cases have affected the toes.[1],[2],[5],[6] However, in our case, the thumb has been affected. To the best of our knowledge, this is the first acral angioosteoma cutis case described in the thumb.
Acral angioosteoma cutis is a benign lesion occurring on the acral skin characterized by vascular and bony proliferation.[2] It is composed of well-formed capillaries, pale stroma, bland fibroblast-like cells, and multiple tiny spicules of woven bone. However, there is no lobular pattern in the capillary proliferation which is a typical histopathological feature in pyogenic granuloma.[1],[6] Our case demonstrated the histologic features of acral angioosteoma cutis.
The pathogenesis of acral angioosteoma cutis is still unclear. It is thought that the pathogenesis of acral angioosteoma cutis is similar to the process of ossification in other hemagiomas.[1],[3] However, the pathogenesis of metaplastic ossification has not yet been elucidated. Vascular endothelial growth factor and bone morphogenetic proteins may play a role in ectopic bone formation insuch cases.[1],[4],[5] Vascular endothelial growth factors and bone morphogenetic proteins are synthesized by various cells including endothelial cells and osteoblasts in response to hypoxia, trauma, or inflammation.[3],[4] Our case provided a history of preceding trauma.
Differential diagnoses include subungal exostosis (fibrocartilaginous cap surrounding the lesion without vascular proliferation having typical X-ray findings), osteoma cutis (ectopic ossification withou proliferation of vascular channels), and fibro-osseous pseudotumor (ossification without vascular proliferation). Our case showed vascular proliferation thus ruling out these differentials.[1],[3],[5],[7] Based on the absence of lobular capillary proliferation in the biopsy, a pyogenic granuloma with ossification was also excluded.
Only few cases of acral angioosteoma cutis have been reported till date. However, some authors feel many cases of acral angioosteoma cutis are misdiagnosed as pyogenic granuloma or other acral lesions.[3],[6]
Surgical excision of acral angioosteoma cutis is the treatment of choice. Chance of recurrence is minimal as it has been reported in only one of 14 cases in literature[6] Recurrence was not observed after 1 year follow-up in our case.
Thus, we have reported a case of acral angioosteoma cutis which is a rare and recently described entity. Cutaneous ossification tumours should be considered for such presentations.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Lee EJ, Lee JH, Shin MK, Lee SW, Haw CR. Acral angioosteoma cutis. Ann Dermatol 2011;23 Suppl 1:S105-7.
[Google Scholar]
|
| 2. |
Googe PB, Page RN, King R, Griffin WC. Acral angioosteoma cutis. Am J Dermatopathol 2006;28:228.
[Google Scholar]
|
| 3. |
Won CY, Cho BK, Park HJ. Acral angioosteoma cutis on the great toe mimicking pyogenic granuloma. Ann Dermatol 2015;27:480-1.
[Google Scholar]
|
| 4. |
Kim ES, Kim KJ, Chang SE, Lee MW, Choi JH, Moon KC, et al. Metaplastic ossification in a cutaneous pyogenic granuloma: A case report. J Dermatol 2004;31:326-9.
[Google Scholar]
|
| 5. |
Song HJ, Hong WK, Han SH, Byun JW, Lee HS, Choi GS, et al. Acral angioosteoma cutis. Am J Dermatopathol 2010;32:477-8.
[Google Scholar]
|
| 6. |
Wang AL, Vandergriff T, Srivastava D, Nijhawan RI. Recurrent acral angioosteoma cutis in a pregnant patient. JAAD Case Rep 2016;2:430-2.
[Google Scholar]
|
| 7. |
Choi KH, You JS, Huh JW, Jeong YI, Kim MS, Jue MS, et al. Fibro-osseous pseudotumor of the digit: A diagnostic pitfall of extraskeletal osteosarcoma. Ann Dermatol 2016;28:495-6.
[Google Scholar]
|
Fulltext Views
3,226
PDF downloads
1,926





