Translate this page into:
Acral papular eruption
Correspondence Address:
Balkrishna Nikam
Department of Dermatology, T N Medical College and B Y L Nair Hospital, Mumbai Central, Mumbai - 400008
India
| How to cite this article: Nikam B, Amladi S, Bingewar G, Nayak C, Wadhwa S L. Acral papular eruption. Indian J Dermatol Venereol Leprol 2005;71:447-448 |
 |
 |
 |
 |
 |
 |
A 16-year-old boy presented with a sudden onset of asymptomatic skin eruption since the past seven days. The lesions initially appeared on the thighs and lower legs, followed by ankles, hands, forearms, feet and progressed to elbows, arms and ear lobes. He also complained of decreased appetite, high colored urine and yellowish discoloration of the eyes since the last two weeks.
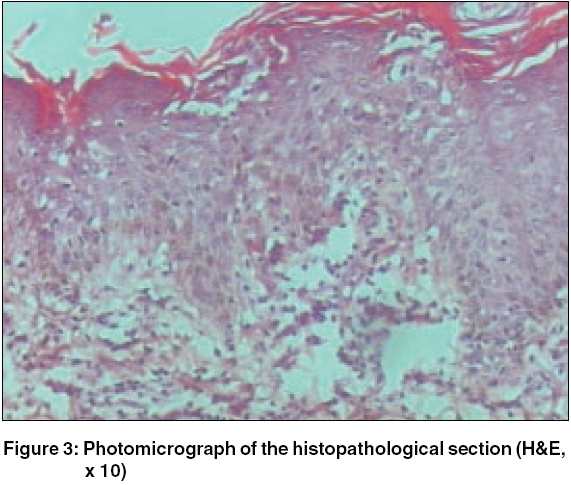
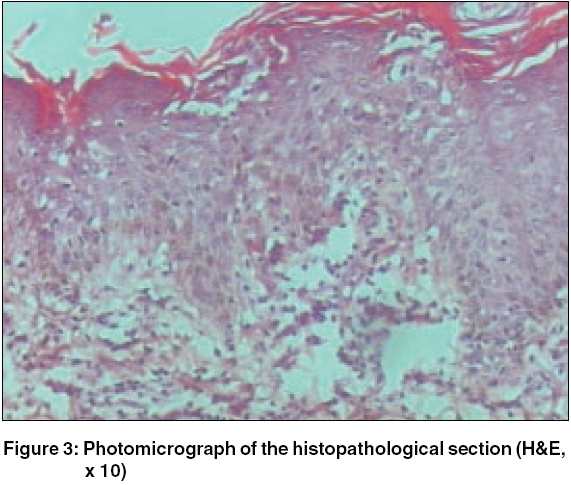
On examination, there were multiple skin colored to erythematous and edematous papules of about 1 to 5 mm size [Figure - 1]. Many of the lesions, located over the extensor aspects of hands [Figure - 2], forearms, elbows and upper arms were topped with tiny crusts and scales whereas others showed a central dusky hue. Examination of the conjunctiva revealed mild icterus. Bilateral axillary, epitrochlear and inguinal nodes were enlarged, non tender, mobile and firm. There was no hepato-splenomegaly.
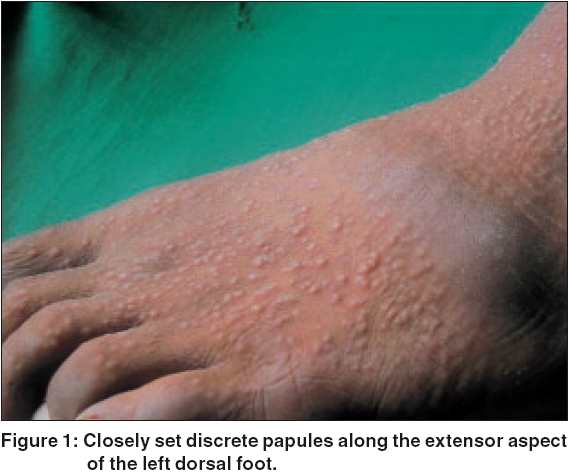
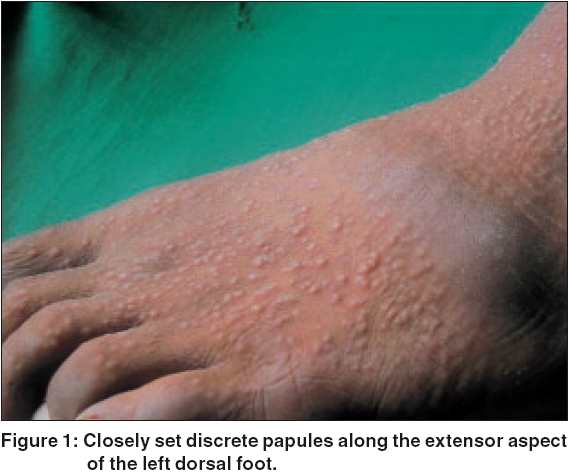
A skin biopsy taken from a papule is presented in [Figure - 3]. On further investigation, he was found to have deranged liver function tests with total bilirubin 1.7 mg%, SGOT 230 U/l, SGPT 375 U/l and serum alkaline phosphatase 502 U/l. He was tested positive for HBsAg.
What is your diagnosis?
Histopathological findings: Haematoxylin and eosin stained histopathological section showed hyperkeratosis, epidermal spongiosis with upper dermal edema and lymphohistiocytic infiltrate, consistent with Gianotti Crosti syndrome.
Diagnosis: Gianotti Crosti Syndrome (GCS)
Treatment and follow-up No topical or systemic medication was prescribed for the rash. On follow up after 7 days, the lesions had regressed spontaneously by about 60%, and complete resolution was noted at the end of 2 weeks.
Discussion
GCS, also known as papular acrodermatitis of childhood, (Gianotti and Crosti, 1955) is a widespread infectious disease seen in childhood.[1] It is characterized by a non-relapsing erythemato-papular dermatitis lasting for about 3 weeks, para-cortical hyperplasia of the lymph nodes, acute hepatitis, usually anicteric, lasting for a minimum period of 2 months and hepatitis B surface antigenemia.[1] Following the initial report, subsequent cases have been found to be associated with a wide range of viruses such as hepatitis B and A virus , Epstein Barr virus , Coxsackie A16 , B4 and B5, echovirus, polio virus, cytomegalovirus, respiratory syncytial virus, parainfluenza virus, parvovirus and human immunodeficiency virus .[2],[3]
The term GCS has now been accepted to include all acrally located eruptive dermatoses clinically characterized by papular or papulovesicular lesions caused by different viruses and running a benign, self limiting course.[4] The condition appears to be a cutaneous response to viral infection that regresses spontaneously. The clinical manifestations are variable with individual patient characteristics rather than the associated virus.[4]
GCS[1] mainly affects children between the ages of 6 months to 12 years, though rarely adults can be the sufferers. The eruption consists of monomorphic, flat, lentil-sized, erythemato-papular, non-itchy lesions symmetrically distributed over face, buttocks and limbs. The lesions may be dense but do not coalesce and occasionally become purpuric, especially over the lower legs. Onset of the rash is acute over a few days and lasts for 2 to 8 weeks with spontaneous regression. Recurrences are unlikely. Lymph nodes, mainly axillary and inguinal, are moderately enlarged, firm and freely movable and may persist for 2 to 3 months.
Biopsy of the skin lesion shows hyperkeratosis with mild to moderate acanthosis, papillary dermal edema and superficial perivascular infiltrate of mononuclear cells and histiocytes. Diagnosis is usually based on the typical clinical features;[5] however conditions such as papular urticaria, scabies, lichen planus, hand-foot-mouth disease, erythema multiforme, pityriasis lichenoides and Henoch-Schonlein purpura may have to be differentiated.[5] Extensive truncal and scaly lesions are proposed to be negative clinical features. No treatment is required for the skin lesions. Patients suffering from hepatitis B need prolonged treatment and follow-up.
In hepatitis-associated GCS,[1] the patient is usually anicteric. However, icterus may develop concurrent with the rash or after its subsidence. Moderate hepatomegaly and deranged liver function tests may be seen and HBsAg may be positive. Changes in the laboratory parameters usually persist for 1-3 months but in 50% cases, may persist for years.
| 1. |
Gianotti F. Papular acrodermatitis of childhood and other papulo-vesicular acro-located syndromes. Br J Dermatol 1979;100:49-59.
[Google Scholar]
|
| 2. |
Gelmetti C. Gianotti Crosti Syndrome. In: John Harper, Arnold Oranje, Neil Prose, editors. Textbook of Pediatric Dermatology. Oxford: Blackwell Science; 2000. p. 347-51.
[Google Scholar]
|
| 3. |
Blauvelt A, Turner M. Gianotti-Crosti syndrome and human immunodeficiency virus infection. Arch Dermatol 1994:130;481-3.
[Google Scholar]
|
| 4. |
Caputo R, Gelmetti C, Ermacora E. Gianotti-Crosti syndrome: A retrospective analysis of 308 cases. J Am Acad Dermatol 1992:26;207-10.
[Google Scholar]
|
| 5. |
Chuh A, Lee A, Zawar V. The diagnostic criteria of Gianotti Crosti syndrome - are they applicable to children in India? Pediatr Dermatol 2004;21:542-7.
[Google Scholar]
|
Fulltext Views
6,267
PDF downloads
1,757





