Translate this page into:
Acroangiodermatitis of mali: A rare vascular phenomenon
Correspondence Address:
Chitra S Nayak
302 Arun, 6th Road, Santacruz (East), Mumbai-400 055
India
| How to cite this article: Mehta AA, Pereira RR, Nayak CS, Dhurat RS. Acroangiodermatitis of mali: A rare vascular phenomenon. Indian J Dermatol Venereol Leprol 2010;76:553-556 |
Abstract
Acroangiodermatitis (synonym pseudo-Kaposi sarcoma) is an unusual, benign condition which clinically presents as purple-colored patches, plaques or nodules, mostly on the extensor surfaces of lower extremities in patients with chronic venous insufficiency and arteriovenous malformations. It resembles aggressive conditions like Kaposi's sarcoma and requires histopathological examination for its diagnosis. We report two such cases of acroangiodermatitis. Histopathology of both the cases showed dilated capillaries in the dermis with extravasated red blood corpuscles (RBCs), hemosiderin deposits, and hyperplastic granulation tissue. Both were treated with oral antibiotics and topical steroids. The ulcers showed a good response within 2 months of treatment.Introduction
Acroangiodermatitis is a reactive angiodysplasia of cutaneous blood vessels associated with venous insufficiency or with vascular anomalies such as Klippel-Trenaunay syndrome or stump dermatosis in amputees. Exaggerated stasis dermatitis begins as violaceous macules and patches that gradually develop into papule, nodules, or indurated plaques often bilateral, and usually located on the lower extremities with edema. Although benign, it may mimic malignant conditions like Kaposi′s sarcoma and therefore requires histopathological examination for its diagnosis and differentiation.
Here, we report two such cases presenting with nodulo-ulcerative lesions, with histological features of acroangiodermatitis, emphasizing the importance of histopathology in differentiating this from similarly presenting conditions.
Case Reports
Case 1
A 41-year-old farmer in good health presented with a 4 year history of two raised lesions over dorsum of the left foot. There was a 2 year history of recurrent bleeding and persistent swelling over the left ankle. He was a diagnosed case of varicose veins in both lower extremities for which he was treated with vein stripping and laser sclerotherapy, 2 years prior to presentation. On examination, there were two well-defined, soft, compressible hyperpigmented nodules of approximate dimensions 1 Χ 1 Χ 1 cm and 3 Χ 3 Χ 1.5 cm, respectively, over the dorsum of left foot. The larger nodule showed surface ulceration with a hemorrhagic crust [Figure - 1]. There was no local tenderness or palpable thrill. The peripheral pulsations were felt. The saphenofemoral junction was competent on the Brodie-Trendelenburg test and perforators of the left leg were incompetent on the multiple tourniquet test. There were ill-defined hyperpigmented scaly, lichenified plaques on the volar aspect of the left foot, and left medial malleolus with minute hyperpigmented macules coalescing to form patches on inferomedial aspect of left leg. Examination of the right leg was within normal limits. A differential diagnosis of keratoacanthoma and Kaposi′s sarcoma was considered in a patient of varicose veins.
 |
| Figure 1 :Hyperpigmented nodule with surface ulceration and hemorrhagic crust (Case 1) |
Case 2
A 26-year-old man presented with a single, pus discharging verrucous growth and swelling over the left ankle for 4 years. There was history of recurrent bleeding from the lesion. On examination, an ulcerated plaque with lobulated surface and serosanguinous discharge was found to be present on the lateral aspect of the left leg. The skin surrounding the ulcer showed dilated tortuous veins [Figure - 2]. There was no local tenderness, palpable thrill, or bruit. The arterial pulsations were felt. The saphenofemoral junction was competent on the Brodie-Trendelenburg test but the lower perforator of the left leg was incompetent on the multiple tourniquet test. Examination of the right leg revealed no abnormality.
 |
| Figure 2 :Ulcerated plaque with lobulated surface on lateral aspect of the left leg (Case 2) |
A differential diagnosis of Kaposi′s sarcoma and chromoblastomycosis was considered.
In both the cases, hematological and biochemical investigations were normal. Serological testing for HIV was negative. A lesional skin biopsy from both cases showed hyperkeratotic stratum corneum, dilated capillaries with plump endothelial cells, extravasated RBCs, and hemosiderin, surrounded by hyperplastic granulation tissue with perivascular mononuclear infiltrate in the upper dermis [Figure - 3]a, b. No vascular slits were seen. The hemosiderin deposits were confirmed on Perl′s stain.
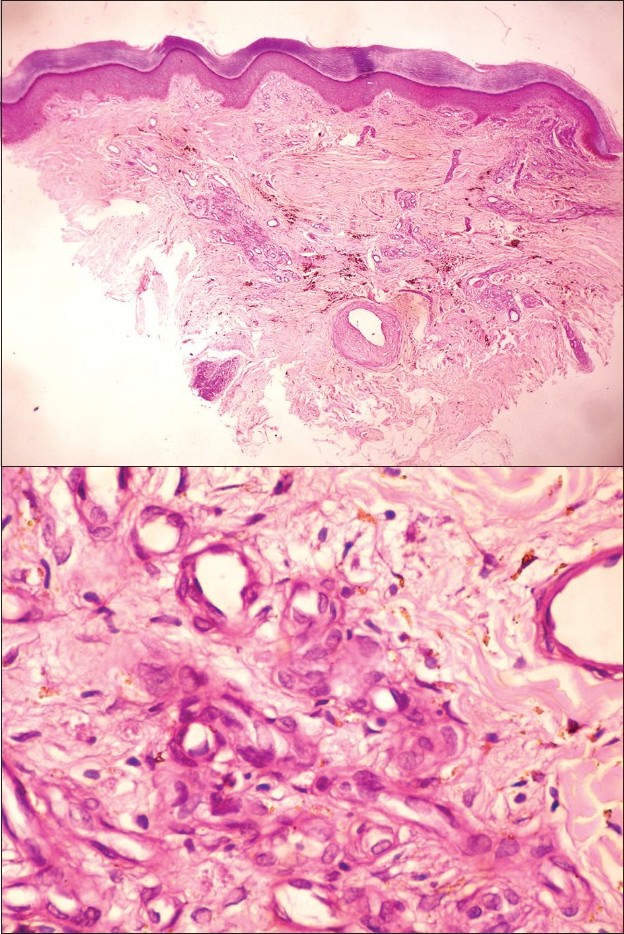 |
| Figure 3 :(a) Hyperkeratotic stratum corneum with proliferation of capillaries in upper and mid-dermis (H and E, ×40) Figure 3b: Capillaries showing plump endothelial cells and perivascular mononuclear infiltrate (H and E, ×400) |
In the first case, venous Doppler showed multiple varicosities along course of the great saphenous vein with four incompetent perforators (mid thigh, upper leg, mid leg and lower leg) in the left lower extremity. The second case showed normal venous flow in left iliac vein with dilated left popliteal vein and patent venous valves. The saphenofemoral junction was competent in both the cases.
On the basis of the history, examination and biopsy findings, a final diagnosis of acroangiodermatitis of Mali was made in both the cases.
The first case was treated with oral erythromycin, topical clobetasol propionate (0.05%) cream, oral calcium dobesilate 500 mg twice daily, and emollients for 3 weeks. In addition, he was advised leg elevation and compression therapy with an elastocrepe bandage. After 3 weeks, calcium dobesilate was continued along with compression therapy. The ulcers responded well and healed with hyperpigmentation in 2 months but the nodular lesions persisted.
The second case was treated with oral doxycycline, oral metronidazole, topical clobetasol propionate (0.05%) cream, oral calcium dobesilate 500 mg twice daily, and emollients initially for 15 days. He was advised leg elevation and compression with elastocrepe bandage. The ulcers responded well and started to heal with scar formation. Antibiotics were discontinued and the calcium dobesilate and compression therapy were continued. The ulcers healed completely with scarring and dyspigmentation over the next 4 months [Figure - 4].
 |
| Figure 4 :Healing of ulcer at 2 months of treatment (Case 2) |
Discussion
Acroangiodermatitis (Synonyms: pseudo-Kaposi′s sarcoma, acroangiodermatitis of Mali-Kuiper, gravitational purpura, stasis purpura) was first coined by Mali in 1965. [1] It is a proliferation of pre-existing vasculature seen in venous hypertension, arteriovenous malformation, or acquired iatrogenic arteriovenous (AV) fistula. A variety of vascular conditions giving rise to this venous pathology include Klippel-Trenaunay syndrome, stump dermatosis in amputees, paralyzed limb, and intravenous drug abuse. It is rarely reported in hereditary coagulation defects (carrier of the thrombophilic 20210A mutation in the prothrombin gene and homozygous activated protein C resistance). [2],[3] Most of the cases of acroangiodermatitis have been associated with some signs of venous insufficiency however Barbar et al. reported no venous insufficiency in 9 of their 10 cases of acroangiodermatitis, and similar spontaneous acroangiodermatitis in a young woman has been reported. [4],[5] Our first case had venous insufficiency but in the second case, though there was normal Doppler study, the patient had localized dilated and tortuous veins around the lesion suggesting some degree of venous insufficiency as an etiologic factor in the development of the lesions.
There are various variants of acroangiodermatitis:
- Stewart-Bluefarb syndrome is a congenital arteriovenous malformation of the lower leg with multiple arteriovenous shunts. It begins early in life unilaterally over lower extremities with painful purple papules and macules, which may ulcerate. The affected limb may show increased warmth with varicose veins and a palpable thrill can be felt. [1]
- Mali type is an exaggerated stasis dermatitis seen in elderly patients, usually bilateral with chronic venous insufficiency on dorsum of feet, hallux, and second toe or on medial aspect of lower legs. The lesions begin as violaceous macules and patches that develop slowly into soft, nontender, red to purple papules and nodules or indurated plaques. [1] Both our patients had this variant of acroangiodermatitis.
- Acroangiodermatitis in first pregnancy appears as gravity purpura (Dermite ocre of Favre) on lower legs over site of venous varicosities extending to the dorsa of feet and toes. [6]
- Angiodermatitis occurring after placement of the arteriovenous shunt for hemodialysis in chronic renal failure. [6]
Although precise etiology is unknown, it is postulated that severe chronic venous stasis with insufficiency of the calf muscle pump elevates the capillary pressure and leads to chronic tissue hypoxia from chronic edema which induces neovascularisation and fibroblast proliferation. [6],[7]
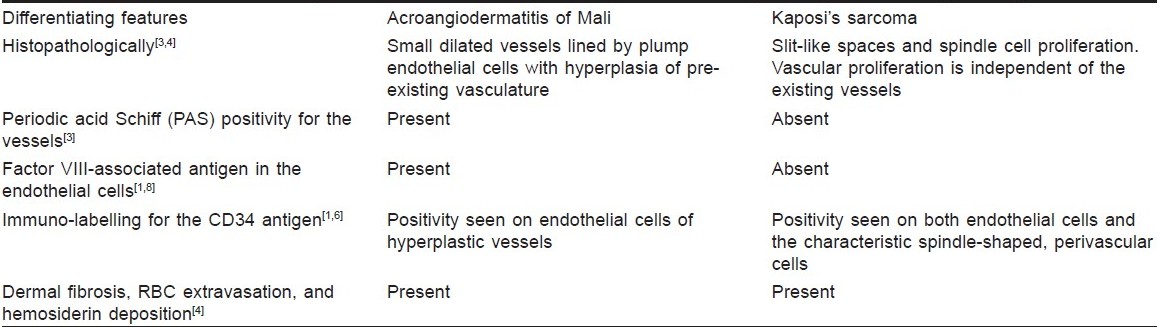
The histopathologic differentials for acroangiodermatitis are Kaposi′s sarcoma [Table - 1], pigmented purpuric dermatitis (PPD), vasculitis, and stasis dermatitis. [4]
PPD has dilated capillaries with the absence of plump endothelial cells, dermal fibrosis, or eosinophils in dermal infiltrates as seen in acroangiodermatitis. Fibrinoid necrosis of the vessels is seen in vasculitis as opposed to acroangiodermatitis. Stasis dermatitis differs from acroangiodermatitis by epidermal changes (parakeratosis and spongiosis), deeper dermal involvement, and greater hemosiderin deposition. [4]
Treatment of acroangiodermatitis involves correction of the underlying vascular pathology with mainstay of therapy being compression stockings or a compression pump for venous stasis and local wound care for ulcers. Various medical modalities of therapy have been tried with favorable results but options are limited. Oral erythromycin 500 mg four times a day or dapsone 50 mg twice a day for 3 months in combination with compression therapy has been tried with good results. [3] Topical therapy with local corticosteroid preparations is often useful. [6] Underlying vascular pathology like arteriovenous malformations can be surgically managed with elimination of the shunts and embolization for small fistulae. [1],[2],[9] Laser ablation, such as pulsed-dye laser, may clear some individual lesions. [2]
We would like to emphasize the importance of histopathology in distinguishing this benign condition from similar looking malignant conditions, even in the absence of predisposing factors such as varicose veins.
| 1. |
Agrawal S, Rizal A, Agrawal C, Agrawal A. Pseudo-Kaposi′s sarcoma (Bluefarb-Stewart type). Int J Dermatol 2005;44:136-8.
[Google Scholar]
|
| 2. |
Rongioletti F, Rebora A. Cutaneous reactive angiomatoses: Patterns and classification of reactive vascular proliferation. J Am Acad Dermatol 2003;49:887-96.
[Google Scholar]
|
| 3. |
Heller M, Karen JK, Fangman W. Acroangiodermatitis. Dermatol Online J 2007;13:2. Available from: http://www.dermatologys10.cdlib.org/131/cases/NYUcases/101805_3.html . [last cited on 2010 Feb 3].
[Google Scholar]
|
| 4. |
Rao B, Unis M, Poulos E. Acroangiodermatitis: A study of ten cases. Int J Dermatol 1994;33:179-83.
[Google Scholar]
|
| 5. |
Hung NA, Strack M, Rij AV, North CJ, Blennerhassett JB. Spontaneous acroangiodermatitis in a young woman. Dermatol Online J 2004;10:8. Available from: http://www.dermatology-s10.cdlib.org/131/cases/NYUcases/101805_3.html . [last cited on 2010 Feb 3].
[Google Scholar]
|
| 6. |
Lugovic L, Pusic J, Situm M, Buljan M, Vedrana B, Klaudija S, et al. Acroangiodermatitis (Pseudo-Kaposi sarcoma): Three case reports. Acta Dermatovenerol Croat 2007;15:152-7.
[Google Scholar]
|
| 7. |
Philips T. Acroangiodermatitis of Mali. In: Bolognia JL, Jorizzo JL, Rapini RP, editors. Bolognia Textbook of Dermatology. 2 nd ed. Spain: Mosby Elsevier publishing; 2008. p. 1604.
[Google Scholar]
|
| 8. |
Kapdagli H, Gunduz K, Ozturk G, Kandiloglu G. Pseudo-Kaposi′s sarcoma (Mali type). Int J Dermatol 1998;37:221-30.
[Google Scholar]
|
| 9. |
Zutt M, Emmert S, Moussa I, Haas E, Mitteldorf C, Bertsch HP, et al. Acroangiodermatitis of Mali resulting from arteriovenous malformation: report of a case of Stewart-Bluefarb syndrome. Clin Exp Dermatol 2007;33:22-5.
[Google Scholar]
|
Fulltext Views
15,822
PDF downloads
2,613





