Translate this page into:
Acute erythematous pustular plaques on the hands triggered by driving
Corresponding author: Dr. Erika L Alba-Rojas, Department of Dermatology, Hospital Universitario Dr. José Eleuterio González, Universidad Autónoma de Nuevo León, Av. Madero and Gonzalitos Mitras Centro, Monterrey-64460, Mexico. eri9ar@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Luna-Garza DK, Aguilar-Calderón PE, Rodriguez-Tamez G, Brown-Herrera A, Brussolo-Marroquin E, Ocampo-Candiani J, et al. Acute erythematous pustular plaques on the hands triggered by driving. Indian J Dermatol Venereol Leprol. 2024;90:676-7. doi: 10.25259/IJDVL_1143_2023
A 67-year-old taxi driver with type 2 diabetes and systemic hypertension, presented with a 2-week history of symmetrical edematous dusky erythematous plaques with overlying bullae on both hands [Figure 1]. The patient denied any personal history of medications, recent infections, weight loss, or other relevant skin manifestations. Further questioning revealed that he spent a significant amount of his time driving, applying constant pressure in the areas of the lesions. A skin biopsy was taken for histopathological examination [Figure 2].

- Symmetrical edematous violaceous plaques and bullae on both hands.
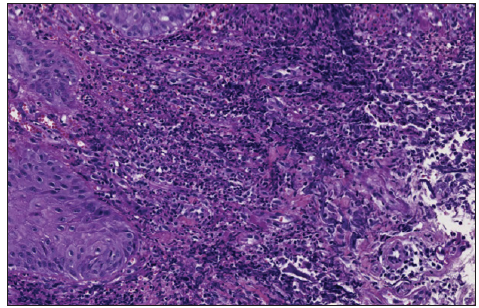
- Dense dermal neutrophilic infiltrate (Haematoxylin and eosin stain, x40).
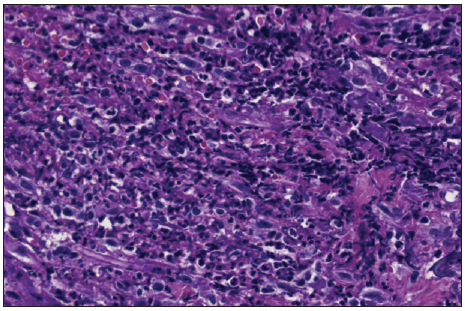
- Dense dermal neutrophilic infiltrate (Haematoxylin and eosin stain, x100).
Question
What is your diagnosis?
Answer
Diagnosis: Neutrophilic dermatosis of the dorsal hands (NDDH)
Investigations and follow-up
Histopathology revealed slight spongiosis in the epidermis, and dense neutrophilic infiltrate with focal leukocytoclasia in the reticular dermis [Figure 2]. A diagnosis of neutrophilic dermatosis of the dorsal hands (NDDH) was established. Blood tests revealed a borderline elevated C reactive protein (CRP) (6.35 mg/L; normal range 1–3) with remaining parameters within normal ranges. Malignancy screening revealed the absence of any neoplastic processes. Treatment with prednisone, 40 mg daily, was started in a tapering regimen for 4 weeks, resulting in complete resolution at the 2-month follow-up [Figure 3].

- Improvement of neutrophilic dermatosis of dorsal hands after treatment.
Discussion
Neutrophilic dermatosis of the dorsal hands (NDDH) was categorised as a localised variant of Sweet syndrome by Galaria et al.1 in the year 2000. It was first described as ‘pustular vasculitis’ by Strutton et al. in 1995, who presented six patients with similar Sweet syndrome-like histopathological and clinical features limited to the dorsa of hands.2
Neutrophilic dermatosis comprises a group of skin disorders characterised by a dense dermal, epidermal, and/or subcutaneous neutrophilic infiltrate. Lesions are mostly located on the dorsum of the hands, nonetheless, they may present in other locations.1 They manifest as papules, nodules plaques, bullae, and pustules, and may be associated with necrosis and ulceration giving an infectious appearance.2 Hence, being a relatively new entity, it may be mistreated with antibiotics or unnecessary procedures.
When assessing a patient exhibiting cutaneous manifestations resembling NDDH, it is essential to explore a spectrum of differential diagnoses due to the overlapping clinical features. The differential diagnosis ranges from herpetiform dermatitis, erysipelas, erythema elevatum diutinum, contact dermatitis, pyoderma gangrenosum, dyshidrotic eczema, infections, or palmoplantar pustulosis.3,4 In the present case, our differentials were contact dermatitis or neutrophilic dermatosis.
The diagnosis is established on histopathology characterised by the presence of a dense neutrophilic infiltrate in the dermis. Moreover, it is pathologically classified as a variant of Sweet syndrome with indistinguishable histological findings.3
Most patients have a history of triggering traumas, such as gardening injuries, cooking burns, intravenous line insertions, and intravenous drug use, which present within 7–10 days after the event. Furthermore, it is crucial to intentionally interrogate for a history of trauma, as the pathergy phenomenon is described in other neutrophilic disorders.5
Some haematological disorders, recent infections, solid organ tumours, and inflammatory bowel disease have been associated with NDDH. Therefore, a thorough systematic evaluation with full blood count and serum protein electrophoresis is recommended to exclude any associated diseases. The first-line treatment is systemic steroids. However, many cases have been successfully treated with topical steroids.3
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Neutrophilic dermatosis of the dorsal hands: Pustular vasculitis revisited. J Am Acad Dermatol. 2000;43:870-4.
- [CrossRef] [PubMed] [Google Scholar]
- Pustular vasculitis of the hands. J Am Acad Dermatol. 1995;32:192-8.
- [CrossRef] [PubMed] [Google Scholar]
- Neutrophilic dermatosis of the dorsal hands: A review of 123 cases. J Am Acad Dermatol. 2023;88:1338-44.
- [CrossRef] [PubMed] [Google Scholar]
- A case of neutrophilic dermatosis of the dorsal hands with concomitant involvement of the lips. Ann Dermatol. 2010;22:106-9.
- [CrossRef] [PubMed] [Google Scholar]
- Neutrophilic dermatosis of the dorsal hands triggered by mechanical trauma. J Eur Acad Dermatol Venereol. 2021;35:20-1.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





